Abstract
Purpose of Review
This review aims to discuss sex differences observed in preclinical rodent models of opioid reward.
Recent Findings
Utilizing a variety of methodological approaches and drug regimens, no clear consensus has emerged regarding the effects of opiates between males and females. This is quite dissimilar to work examining psychostimulants, where female animals reliably exhibit stronger behavioral responses.
Summary
With opioid research quickly expanding to determine the neural underpinnings of opioid addiction, further research is essential to determine the conditions wherein sex differences may occur and how they may relate to the human condition.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Brownstein MJ. A brief history of opiates, opioid peptides, and opioid receptors. Proc Natl Acad Sci. 1993;90:5391–3. https://doi.org/10.1073/pnas.90.12.5391.
Courtwright DT. Dark paradise : a history of opiate addiction in America: Harvard University Press; 2001.
Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States. JAMA Psychiatry. 2014;71:821.
Van Zee A. The promotion and marketing of oxycontin: commercial triumph, public health tragedy. Am J Public Health. 2009;99:221–7.
Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths — United States, 2013–2017. MMWR Morb Mortal Wkly Rep. 2018. https://doi.org/10.15585/mmwr.mm6751521e1.
ASAM (2016) Opioid addiction 2016 facts & figures. https://doi.org/10.15585/mmwr.mm655051e1.
CDC (2018) Prescription painkiller overdoses.
Back SE, Payne RL, Wahlquist AH, Carter RE, Stroud Z, Haynes L, et al. Comparative profiles of men and women with opioid dependence: results from a National Multisite Effectiveness Trial. Am J Drug Alcohol Abuse. 2011;37:313–23.
Bose J, Hedden SL, Lipari RN, Park-Lee E (2017) 2017 NSDUH Annual National Report | CBHSQ.
Wesson DR, Ling W. The clinical opiate withdrawal scale (COWS). J Psychoactive Drugs. 2003;35:253–9.
•• Volkow ND, Koob GF, McLellan AT. Neurobiologic advances from the brain disease model of addiction. N Engl J Med. 2016;374:363–71 Reviews how drugs of abuse blunt brain reward circuitry, co-opt learning networks, and weaken frontal-lobe executive function to increase probability of relapse.
•• Shansky RM (2019) Are hormones a “female problem” for animal research? Science (80- ) 364:825 Discusses the historical view surrounding female research and why that view is outdated.
Phoenix C, Goy R, Gerall A, Young W. Organizing action of prenatally administered testosterone propionate on the tissues mediating mating behavior in the female guinea pig. Endocrinology. 1959;65:369–82.
Marrocco J, McEwen BS. Sex in the brain: hormones and sex differences. Dialogues Clin Neurosci. 2016;18:373.
Deroo BJ, Korach KS. Estrogen receptors and human disease. J Clin Invest. 2006;116:561–70.
Driggers PH, Segars JH. Estrogen action and cytoplasmic signaling pathways. Part II: the role of growth factors and phosphorylation in estrogen signaling. Trends Endocrinol Metab. 2002;13:422–7.
Pedram A, Razandi M, Levin ER. Nature of functional estrogen receptors at the plasma membrane. Mol Endocrinol. 2006;20:1996–2009.
•• Krentzel AA, Meitzen J. Biological sex, estradiol and striatal medium spiny neuron physiology: a mini-review. Front Cell Neurosci. 201812:496. https://doi.org/10.3389/fncel.2018.00492Reviews how estradiol can modulate intrinsic and synaptic properties of medium spiny neurons in the rat estrus cycle and the human menstrual cycle. Also describes possible roles of both estradiol and membrane estrogen receptors in these changes.
Meitzen J, Luoma JI, Boulware MI, Hedges VL, Peterson BM, Tuomela K, et al. Palmitoylation of estrogen receptors is essential for neuronal membrane signaling. Endocrinology. 2013;154:4293–304.
Revankar CM, Cimino DF, Sklar LA, Arterburn JB, Prossnitz ER. A transmembrane intracellular estrogen receptor mediates rapid cell signaling. Science. 2005;307:1625–30.
Liu NJ, Chakrabarti S, Schnell S, Wessendorf M, Gintzler AR. Spinal synthesis of estrogen and concomitant signaling by membrane estrogen receptors regulate spinal κ- and μ-opioid receptor heterodimerization and female-specific spinal morphine antinociception. J Neurosci. 2011;31:11836–45.
Lagrange AH, Ronnekleiv OK, Kelly MJ. Modulation of G protein-coupled receptors by an estrogen receptor that activates protein kinase A. Mol Pharmacol. 1997;51:605–12.
Micevych PE, Rissman EF, Gustafsson J-A, Sinchak K. Estrogen receptor-α is required for estrogen-induced μ-opioid receptor internalization. J Neurosci Res. 2003;71:802–10.
Tonn Eisinger KR, Gross KS, Head BP, Mermelstein PG. Interactions between estrogen receptors and metabotropic glutamate receptors and their impact on drug addiction in females. Horm Behav. 2018;104:130–7. https://doi.org/10.1016/j.yhbeh.2018.03.001.
Frye CA, Rhodes ME, Rosellini R, Svare B. The nucleus accumbens as a site of action for rewarding properties of testosterone and its 5alpha-reduced metabolites. Pharmacol Biochem Behav. 2002;74:119–27.
•• Carroll ME, Lynch WJ. How to study sex differences in addiction using animal models. Addict Biol. 2016. https://doi.org/10.1111/adb.12400Discusses what to consider when studying sex differences in addiction, such as the role of sex hormones and how they interact with other vulnerabilities in addiction such as age and impulsivity.
Lee CW-S, Ho I-K. Sex differences in opioid analgesia and addiction: interactions among opioid receptors and estrogen receptors. Mol Pain. 2013;9:45.
McEwen BS, Milner TA. Understanding the broad influence of sex hormones and sex differences in the brain. J Neurosci Res. 2017;95:24–39.
• Huhn AS, Berry MS, Dunn KE. Systematic review of sex-based differences in opioid-based effects. Int Rev Psychiatry. 2018;30:107–16 Opioid receptors are modulated by the presence of exogenous and endogenous hormones; ovarian hormones may be responsible for the differences seen between males and females.
Chartoff EH, McHugh RK. Translational studies of sex differences in sensitivity to opioid addiction. Neuropsychopharmacology. 2016;41:383–4.
Enforcement Administration D (2017) Drugs of abuse A DEA RESOURCE GUIDE.
Sternini C, Patierno S, Selmer I-S, Kirchgessner A. The opioid system in the gastrointestinal tract. Neurogastroenterol Motil. 2004;16:3–16.
Law P-Y, Wong YH, Loh HH. Molecular mechanisms and regulation of opioid receptor signaling. Annu Rev Pharmacol Toxicol. 2000;40:389–430.
Bohn LM, Gainetdinov RR, Lin FT, Lefkowitz RJ, Caron MG. μ-Opioid receptor desensitization by β-arrestin-2 determines morphine tolerance but not dependence. Nature. 2000;408:720–3.
Bohn LM, Dykstra LA, Lefkowitz RJ, Caron MG, Barak LS. Relative opioid efficacy is determined by the complements of the G protein-coupled receptor desensitization machinery. Mol Pharmacol. 2004;66:106–12.
Whalen EJ, Rajagopal S, Lefkowitz RJ. Therapeutic potential of β-arrestin- and G protein-biased agonists. Trends Mol Med. 2011;17:126–39.
• Abraham A, Schattauer S, Reichard K, Cohen J, Fontaine H, Song A, et al. Estrogen regulation of GRK2 inactivates kappa opioid receptor signaling mediating analgesia, but not aversion. J Neurosci. 2018;38:8031–43 Estradiol in OVX mice inhibits kappa-opioid receptor mediated analgesia, suggesting a possible pathway for differential effects of opioids in male and female subjects.
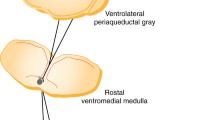
Doyle HH, Eidson LN, Sinkiewicz DM, Murphy AZ. Sex differences in microglia activity within the periaqueductal gray of the rat: a potential mechanism driving the dimorphic effects of morphine. J Neurosci. 2017;37:3202–14.
Russell SE, Rachlin AB, Smith KL, Muschamp J, Berry L, Zhao Z, et al. Sex differences in sensitivity to the depressive-like effects of the kappa opioid receptor agonist U-50488 in rats. Biol Psychiatry. 2014;76:213–22.
Johnson SW, North RA. Opioids excite dopamine neurons by hyperpolarization of local interneurons. J Neurosci. 1992;12:483–8.
Xia Y, Driscoll JR, Wilbrecht L, Margolis EB, Fields HL, Hjelmstad GO. Nucleus accumbens medium spiny neurons target non-dopaminergic neurons in the ventral tegmental area. J Neurosci. 2011;31:7811–6.
Tzschentke TM. Measuring reward with the conditioned place preference paradigm: a comprehensive review of drug effects, recent progress and new issues. Prog Neurobiol. 1998;56:613–72.
McBride WJ, Murphy JM, Ikemoto S. Localization of brain reinforcement mechanisms: intracranial self-administration and intracranial place-conditioning studies. Behav Brain Res. 1999;101:129–52.
Cicero TJ, Ennis T, Ogden J, Meyer ER. Gender differences in the reinforcing properties of morphine. Pharmacol Biochem Behav 2000;65:91–96.
Zarrindast MR, Bahreini T, Adl M. Effect of imipramine on the expression and acquisition of morphine-induced conditioned place preference in mice. Pharmacol Biochem Behav. 2002;73:941–9. https://doi.org/10.1016/S0091-3057(02)00951-6.
Sahraei H, Ghazzaghi H, Zarrindast MR, Ghoshooni H, Sepehri H, Haeri-Rohan A. The role of alpha-adrenoceptor mechanism(s) in morphine-induced conditioned place preference in female mice. Pharmacol Biochem Behav. 2004;78:135–41. https://doi.org/10.1016/j.pbb.2004.03.004.
Alexander BK, Coambs RB, Hadaway PF. The effect of housing and gender on morphine self-administration in rats. Psychopharmacology. 1978;58:175–9.
Hadaway PF, Alexander BK, Coambs RB, Beyerstein B. The effect of housing and gender on preference for morphine-sucrose solutions in rats. Psychopharmacology. 1979;66:87–91.
Craft RM, Stoffel EC, Stratmann JA. Effects of chronic morphine treatment on responding for intracranial stimulation in female versus male rats. Exp Clin Psychopharmacol. 2001;9:198–208.
Mavrikaki M, Pravetoni M, Page S, Potter D, Chartoff E. Oxycodone self-administration in male and female rats. Psychopharmacology. 2017;234:977–87.
Lacy RT, Strickland JC, Feinstein MA, Robinson AM, Smith MA. The effects of sex, estrous cycle, and social contact on cocaine and heroin self-administration in rats. Psychopharmacology. 2016;233:3201–10. https://doi.org/10.1007/s00213-016-4368-9.
Craft RM, Clark JL, Hart SP, Pinckney MK. Sex differences in locomotor effects of morphine in the rat. Pharmacol Biochem Behav. 2006;85:850–8.
Roth ME, Casimir AG, Carroll ME. Influence of estrogen in the acquisition of intravenously self-administered heroin in female rats. Pharmacol Biochem Behav. 2002;72:313–8.
Bonansco C, Martínez-Pinto J, Silva RA, Velásquez VB, Martorell A, Selva MV, et al. Neonatal exposure to oestradiol increases dopaminergic transmission in nucleus accumbens and morphine-induced conditioned place preference in adult female rats. J Neuroendocrinol. 2018;30:e12574.
Bakker J, De Mees C, Douhard Q, Balthazart J, Gabant P, Szpirer J, et al. Alpha-fetoprotein protects the developing female mouse brain from masculinization and defeminization by estrogens. Nat Neurosci. 2006;9:220–6.
Velásquez VB, Zamorano GA, Martínez-Pinto J, Bonansco C, Jara P, Torres GE, et al. Programming of dopaminergic neurons by early exposure to sex hormones: effects on morphine-induced accumbens dopamine release, reward, and locomotor behavior in male and female rats. Front Pharmacol. 2019;10:295.
Klein LC, Popke EJ, Grunberg NE. Sex differences in effects of predictable and unpredictable footshock on fentanyl self-administration in rats. Exp Clin Psychopharmacol. 1997;5:99–106.
Wang D-M, Zhang J-J, Huang Y-B, Zhao Y-Z, Sui N. Peripubertal stress of male, but not female rats increases morphine-induced conditioned place preference and locomotion in adulthood. Dev Psychobiol. 2019;61:920–9. https://doi.org/10.1002/dev.21839.
• Bravo IM, Luster BR, Flanigan ME, Perez PJ, Cogan ES, Schmidt KT, et al. Divergent behavioral responses in protracted opioid withdrawal in male and female C57BL/6J mice. Eur J Neurosci. 2020;51:742–54 After prolonged morphine abstinence, female mice show greater anxiety-like behavior than males, while locomotor responses to morphine challenge did not differ, indicating highly selective sex diferences in behavioral consequences of withdrawal.
Varholick JA, Pontiggia A, Murphy E, Daniele V, Palme R, Voelkl B, et al. Social dominance hierarchy type and rank contribute to phenotypic variation within cages of laboratory mice. Sci Rep. 2019;9:1–11.
Acknowledgments
The authors would like to thank S. Swanson, A. Chapp, J. Borland, and E. Kim for their assistance with editing the manuscript (University of Minnesota). We would like to thank S. Swanson (University of Minnesota) for his assistance with mouse behavior testing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to report.
Human and Animal Rights
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Topical Collection on Preclinical and Psychophysiology
Rights and permissions
About this article
Cite this article
Lopresti, N.M., Esguerra, M. & Mermelstein, P.G. Sex Differences in Animal Models of Opioid Reward. Curr Sex Health Rep 12, 186–194 (2020). https://doi.org/10.1007/s11930-020-00266-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11930-020-00266-4