Abstract
Purpose of Review
We performed a systematic review of the literature on the epidemiology, pathogenesis, clinical and laboratory characterization, and treatment of calcinosis in patients with juvenile dermatomyositis (JDM). A qualitative systematic review was conducted from January 1975 to April 2023 according to the PRISMA protocol using three electronic databases: PubMed, Web of Science, and Scopus. Studies were analyzed based on the following eligibility criteria: at least one combination of the terms described in the search strategy appeared in the title, written in English, Portuguese, or Spanish, and addressed the epidemiology, pathogenesis, diagnosis, and treatment of calcinosis in juvenile dermatomyositis. Systematic or scoping reviews, letters, clinical images, book chapters, abstracts, inflammatory myopathy in other connective tissue diseases, idiopathic inflammatory myopathies in adults, and purely qualitative studies were excluded.
Recent Findings
Seventy-five studies were included. According to the literature, calcinosis is common in women, around five years old, with three years of disease in association with osteoarticular, cutaneous, pulmonary manifestations, and fever. The pathogenesis is still unknown, but the participation of interleukin 1 and 6, tumor necrosis factor alpha, and innate immunity dysregulation seem to be involved. Common autoantibodies are anti-NXP-2, anti-MDA-5, and anti-Mi-2, and their treatment remains controversial. Prospective, randomized, controlled studies are needed to evaluate treatment protocols and map the natural history of this serious complication.
Summary
Calcinosis seems to be more common in White female children with muscle weakness, fever, arthritis, severe pulmonary, and skin involvement with anti-NXP-2, anti-MDA-5, and anti-Mi-2 autoantibodies. The multitargets and aggressive treatment is recommended.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Davuluri S, Duvuri B, Lood C, Faghihi-Kashani S, Chung L. Calcinosis in dermatomyositis: Origins and possible therapeutic avenues. Best Pract Res Clin Rheumatol. 2022;36: 101768. https://doi.org/10.1016/j.berh.2022.101768.
Lundberg I, Fujimoto M, Vencovsky J, et al. Idiopathic inflammatory myopathies. Nat Rev Dis Primers. 2021;7:86. https://doi.org/10.1038/s41572-021-00321-x.
• McCann LJ, Juggins AD, Maillard SM, et al. The Juvenile Dermatomyositis National Registry and 290 Repository (UK and Ireland) - clinical characteristics of children recruited within the first 5 yr. Rheumatology. 2006;45:1255–60. https://doi.org/10.1093/rheumatology/kel099. This study describes a cohort that helps understand the natural history of the disease.
Clemente G, Piotto DGP, Barbosa C, et al. High frequency of calcinosis in juvenile 293 dermatomyositis: a risk factor study. Rev Bras Reumatol. 2012;52:549–53.
Chander S, Gordon P. Soft tissue and subcutaneous calcification in connective tissue diseases. Curr Opin Rheumatol. 2012;24:158–64. https://doi.org/10.1097/BOR.0b013e32834ff5cd.
Chung MP, Richardson C, Kirakossian D, et al. Calcinosis biomarkers in adult and juvenile dermatomyositis. Autoimmun Rev. 2020;19: 102533. https://doi.org/10.1016/j.autrev.2020.102533.
Elahmar H, Feldman BM, Johnson SR. Management of calcinosis cutis in rheumatic diseases. J Rheumatol. 2022;49:980–9. https://doi.org/10.3899/jrheum.211393.
Shinjo SK, Souza FH. Update on the treatment of calcinosis in dermatomyositis. Rev Bras Reumatol. 2013;53:211–4.
Traineua H, Aggarwal R, Monfort J-B, et al. Treatment of calcinosis cutis in systemic sclerosis and dermatomyositis: A review of the literature. J Am Acad Dermatol. 2022;82:317–25. https://doi.org/10.1016/j.jaad.2019.07.006.
Bohan A, Peter JB. Polymyositis and dermatomyositis (first of two parts). N Engl J Med. 1975;292:344–7. https://doi.org/10.1056/NEJM197502132920706.
•• Duvvuri B, Pachman LM, Hermanson P, et al. Role of mitochondria in the myopathy of juvenile dermatomyositis and implications for skeletal muscle calcinosis. J Autoimmun. 2023;138: 103061. https://doi.org/10.1016/j.jaut.2023.103061. This study highlights possible pathophysiological pathways of calcinosis in JDM.
Mastrolia MV, Orsini SI, Marrani E, et al. Efficacy of Janus kinase inhibitor baricitinib in the treatment of refractory juvenile dermatomyositis complicated by calcinosis. Clin Exp Rheumatol. 2023;41:402–3. https://doi.org/10.55563/clinexprheumatol/7k9ajj.
• Sener S, Basaran O, Batu ED, et al. Early-onset juvenile dermatomyositis: A tertiary referral center experience and review of the literature. Semin Arthritis Rheum. 2023;58: 152133. https://doi.org/10.1016/j.semarthrit.2022.152133. This study describes a cohort that helps understand the natural history of the disease.
• Cancarini P, Nozawa T, Whitney K, et al. The clinical features of juvenile dermatomyositis: A single-centre inception cohort. Semin Arthritis Rheum. 2022;57: 152104. https://doi.org/10.1016/j.semarthrit.2022.152104. This study describes a cohort that helps understand the natural history of the disease.
• El-Garf K, El-Garf A, Salah S, Marzouk H, Farag Y, Mostafa N. A juvenile dermatomyositis: demographics, characteristics and disease outcome in an Egyptian cohort. Clin Exp Rheumatol. 2022;40:450–6. https://doi.org/10.55563/clinexprheumatol/h0s7tq. This study describes a cohort that helps understand the epidemiology of the disease.
Janarthanan M, Mohan M, Murali A. Bisphosphonate therapy for juvenile dermatomyositis-associated calcinosis and metaphyseal zebra lines. BMJ Case Rep. 2022;15: e252814. https://doi.org/10.1136/bcr-2022-252814.
Jin J, Yu H. Use of adalimumab in a child with juvenile dermatomyositis and calcinosis. Indian J Pediatr. 2022;89:1270. https://doi.org/10.1007/s12098-022-04332-8.
Linan-Barroso JM, Gonzalez-Estrada A, García-Morillo JS. Therapy-resistant dermatomyositis with extensive ‘lumbar belt’ calcinosis. BMJ Case Rep. 2022;15: e249110. https://doi.org/10.1136/bcr-2022-249110.
Neely J, Long CS, Sturrock H, Kim S. Association of short-term ultraviolet radiation exposure and disease severity in juvenile dermatomyositis: results from the Childhood Arthritis and Rheumatology Research Alliance Legacy Registry. Arthritis Care Res (Hoboken). 2019;71:1600–5. https://doi.org/10.1002/acr.23840.
Nitiyarom R, Charuvanji S, Likasitwattanakul S, et al. Juvenile dermatomyositis in Thai children: Retrospective review of 30 cases from a tertiary care center. Indian J Dermatol Venereol Leprol. 2023;88:162–70. https://doi.org/10.25259/IJDVL_297_20.
Toplak N, Pimpale Chavan P, et al. Is Anti-NXP2 autoantibody a risk factor for calcinosis and poor outcome in juvenile dermatomyositis patients? Case Series Front Pediatr. 2022;9: 810785. https://doi.org/10.3389/fped.2021.810785.
Concannon A, Han DY. Incidence, severity and clinical manifestations of juvenile dermatomyositis among Maori and Pacific Island compared to European children. J Paediatr Child Health. 2021;57:1881–5. https://doi.org/10.1111/jpc.15595.
Chung CH. Calcinosis universalis in juvenile dermatomyositis. Chonnam Med J. 2020;56: 212213. https://doi.org/10.4068/cmj.2020.56.3.212.
• Campanilho-Marques R, Deakin CT, Simou S, et al. Retrospective analysis of infliximab and adalimumab treatment in a large cohort of juvenile dermatomyositis patients. Arthritis Res Ther. 2020;22:79. https://doi.org/10.1186/s13075-020-02164-5. This study describes a cohort that helps understand the disease's response to immunobiologicals.
Giri S, Parida JR, Dash M, Panda M. pamidronate in treatment of calcinosis in juvenile dermatomyositis. Indian Pediatr. 2020;57:75–6.
Lebrón CV, Montesino MDR, Navarrete VM, Miera FJTS. Treatment with rituximab in juvenile dermatomyositis: effect on calcinosis. Reumatol Clin. 2020;16:368–70. https://doi.org/10.1016/j.reuma.2018.06.010.
Moegle C, Lipsker D. Juvenile dermatomyositis: A series of 22 cases. Ann Dermatol Venereol. 2020;147:494–503. https://doi.org/10.1016/j.annder.2020.04.016.
Tsaltskan V, Aldous A, Serafi S, et al. Long-term outcomes in juvenile myositis patients. Semin Arthritis Rheum. 2020;50:149–55. https://doi.org/10.1016/j.semarthrit.2019.06.014.
Rathore U, Gupta L. Scalp calcinosis in juvenile dermatomyositis. Rheumatology. 2020;60:1569. https://doi.org/10.1093/rheumatology/keaa566.
Sukumaran S, Vijayan V. Abatacept in the treatment of juvenile dermatomyositis-associated calcifications in a 16-year-old girl. Case Rep Rheumatol. 2020;28:4073879. https://doi.org/10.1155/2020/4073879.
Li J, Zhou Z. Calcinosis in juvenile dermatomyositis. N Engl J Med. 2019;381: e31. https://doi.org/10.1056/nejmicm1809669.
Gupta P, Shruti S, Chaudhary V, Khullar G, Siraj F. Juvenile dermatomyositis: A case report and review of literature. Cureus. 2019;11: e3935. https://doi.org/10.7759/cureus.3935.
Çakan M, Karadağ ŞG, Ayaz NA. Complete and sustained resolution of calcinosis universalis in a juvenile dermatomyositis case with mycophenolate mofetil. Turk J Pediatr. 2019;61:771–5. https://doi.org/10.24953/turkjped.2019.05.018.
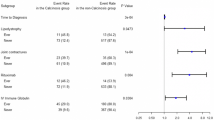
• Orandi AB, Dharnidharka VR, Al-Hammadi N, et al. Clinical phenotypes and biologic treatment use in juvenile dermatomyositis-associated calcinosis. Pediatr Rheumatol Online J. 2018;16:84. https://doi.org/10.1186/s12969-018-0299-9. This study helps understand the disease's response to immunobiologicals.
Al-Mayouf SM, Al Mutiari N, Muzaffer M, et al. Phenotypic characteristics and outcome of juvenile dermatomyositis in Arab children. Rheumatol Int. 2017;37:1513–7. https://doi.org/10.1007/s00296-017-3770-x.
Barut K, Ydin POA, Adrovic A, Sahin S, Kasapcopur O. Juvenile dermatomyositis: a tertiary center experience. Clin Rheumatol. 2017;36:361–6. https://doi.org/10.1007/s10067-016-3530-4.
Grijsen ML, Mchaile D, Geult I, et al. Juvenile dermatomyositis in a 4-year-old Kenyan girl. Clin Case Rep. 2017;5:134–8. https://doi.org/10.1002/ccr3.816.
Phillippi K, Hoeltzel M, Byun Robinson A, et al. Race, income, and disease outcomes in juvenile dermatomyositis. J Pediatr. 2017;184(38–44): e1. https://doi.org/10.1016/j.jpeds.2017.01.046.
Ibarra M, Rigsby C, Morgan GA, Sammet CL, et al. Monitoring change in volume of calcifications in juvenile idiopathic inflammatory myopathy: a pilot study using low dose computed tomography. Pediatr Rheumatol Online J. 2016;14:64. https://doi.org/10.1186/s12969-016-0123-3.
Okong’o LO, Esser M, Wilmshurst J, Scott C. Characteristics and outcome of children with juvenile dermatomyositis in Cape Town: a cross-sectional study. Pediatr Rheumatol Online J. 2016;14:60. https://doi.org/10.1186/s12969-016-0118-0.
Saini I, Kalaivani M, Kabra SK. Calcinosis in juvenile dermatomyositis: frequency, risk factors and outcome. Rheumatol Int. 2016;36:961–5. https://doi.org/10.1007/s00296-016-3467-6.
Nagar RP, Bharati J, Sheriff A, Priyadarshini P, Chumber S, Kabra SK. Calcinosis in juvenile dermatomyositis mimicking cold abscess. Natl Med J India. 2016;29:87–8.
Tayfur AC, Topaloglu R, Gulhan B, Bilginer Y. Bisphosphonates in juvenile dermatomyositis with dystrophic calcinosis. Mod Rheumatol. 2015;25:615–20. https://doi.org/10.3109/14397595.2014.988197.
Turan E, Yesilova Y, Surucu HA, et al. Juvenile dermatomyositis with joint contractures and calcinosis cutis. Dermatol Online J. 2015;21:13030/qt1cg4c5pn.
Faller G, Mistry BJ, Tikly M. Juvenile dermatomyositis in South African children is characterised by frequent dystrophic calcification: a cross sectional study. Pediatr Rheumatol Online J. 2014;12:2. https://doi.org/10.1186/1546-0096-12-2.
Martillotti J, Moote D, Zemel L. Improvement of calcinosis using pamidronate in a patient with juvenile dermatomyositis. Pediatr Radiol. 2014;44:115–8. https://doi.org/10.1007/s00247-013-2738-6.
Meher BK, Mishra P, Sivaraj P, Padhan P. Severe calcinosis cutis with cutaneous ulceration in juvenile dermatomyositis. Indian Pediatr. 2014;251:925–7. https://doi.org/10.1007/s13312-014-0531-8.
Pagnini I, Simonini G, Giani T, et al. Sodium thiosulfate for the treatment of calcinosis secondary to juvenile dermatomyositis. Clin Exp Rheumatol. 2014;32:408–9.
Palaniappan P, Lionel A, Kumar S. Successful treatment of calcinosis cutis in juvenile dermatomyositis with pamidronate. J Clin Rheumatol. 2014;20:454–5. https://doi.org/10.1097/rhu.0000000000000199.
Sanyal S, Atwal SS, Mondal D, Garga UC. Radiographic patterns of soft tissue calcinosis in juvenile dermatomyositis and its clinical implications. J Clin Diagn Res. 2014;8:RD08-11. https://doi.org/10.7860/JCDR/2014/10787.5321.
Tansley SL, Betteridge ZE, Shaddick G, et al. Calcinosis in juvenile dermatomyositis is influenced by both anti-NXP2 autoantibody status and age at disease onset. Rheumatology (Oxford). 2014;53:2204–8. https://doi.org/10.1093/rheumatology/keu259.
Gowdie PJ, Allen RC, Kornberg AJ, Akikusa JD. Clinical features and disease course of patients with juvenile dermatomyositis. Int J Rheum Dis. 2013;16:561–7. https://doi.org/10.1111/1756-185X.12107.
Prasad S, Misra R, Agarwal V, Lawrece A, Aggarwal A. Juvenile dermatomyositis at a tertiary care hospital: is there any change in the last decade? Int J Rheum Dis. 2013;16:556–60. https://doi.org/10.1111/1756-185X.12053.
Toumiy M, Janani S, Rachidi W, Etaouil N, Mkinsi O. Calcinosis universalis complicating juvenile dermatomyositis: improvement after intravenous immunoglobulin therapy. Joint Bone Spine. 2013;80:108–9. https://doi.org/10.1016/j.jbspin.2012.07.001.
Ya-ling L, Jing H, Qian L. A severe case of universal calcinosis with juvenile dermatomyositis. Indian J Dermatol Venereol Leprol. 2021;78:774. https://doi.org/10.4103/0378-6323.102395.
Arabshahi B, Silverman RA, Jones OY, Rider LG. Abatacept and sodium thiosulfate for treatment of recalcitrant juvenile dermatomyositis complicated by ulceration and calcinosis. J Pediatr. 2012;160:520–2. https://doi.org/10.1016/j.jpeds.2011.11.057.
Cairoli E, Garra V, Bruzzone MJ, Gambini JP. Extensive calcinosis in juvenile dermatomyositis. Acta Reumatol Port. 2011;36:180–1.
Lorenzoni PJ, Scola RH, Kay CSK, et al. Idiopathic inflammatory myopathies in childhood: a brief review of 27 cases. Pediatr Neurol. 2011;45:17–22. https://doi.org/10.1016/j.pediatrneurol.2011.01.018.
Al-Mayouf SM, Alsonbul A, Alismail K. Localized calcinosis in juvenile dermatomyositis: successful treatment with intralesional corticosteroids injection. Int J Rheum Dis. 2010;13:e26–8. https://doi.org/10.1111/j.1756-185X.2010.01483.x.
Miyamae T, Sano F, Ozawa R, et al. Efficacy of thalidomide in a girl with inflammatory calcinosis, a severe complication of juvenile dermatomyositis. Pediatr Rheumatol Online J. 2010;8:6. https://doi.org/10.1186/1546-0096-8-6.
Puche AM, Penades IC, Montesinos BL. Effectiveness of the treatment with intravenous pamidronate in calcinosis in juvenile dermatomyositis. Clin Exp Rheumatol. 2010;28:135–40.
Ravelli A, Trail L, Ferrari C, et al. Long-term outcome and prognostic factors of juvenile dermatomyositis: a multinational, multicenter study of 490 patients. Arthritis Care Res (Hoboken). 2010;62:63–72. https://doi.org/10.1002/acr.20015.
Rider LG, Lachenbruch PA, Monroe JB, et al. Damage extent and predictors in adult and juvenile dermatomyositis and polymyositis as determined with the myositis damage index. Arthritis Rheum. 2009;60:3425–35. https://doi.org/10.1002/art.24904.
Slimani S, Abdessemed A, Haddouche A, Ladjouze-Rezig A. Complete resolution of universal calcinosis in a patient with juvenile dermatomyositis using pamidronate. Joint Bone Spine. 2010;77:70–2. https://doi.org/10.1016/j.jbspin.2009.04.011.
Sato JO, Sallum AME, Ferriani VPL, et al. A Brazilian registry of juvenile dermatomyositis: onset features and classification of 189 cases. Clin Exp Rheumatol. 2009;27:1031–8.
Ayala ZM, Ramírez RM, Zerón SM, Fuentes EF, Velázquez RM. Dermatomiositis juvenil y calcinosis extensa. Tratamiento con metilprednisolona y metotrexato. Reumatol Clin. 2008;4:248–50. https://doi.org/10.1016/S1699-258X(08)75546-3.
Riley P, McCann LJ, Maillard SM, et al. Effectiveness of infliximab in the treatment of refractory juvenile dermatomyositis with calcinosis. Rheumatology (Oxford). 2008;47:877–80. https://doi.org/10.1093/rheumatology/ken074.
Jat KR, Singh S. Calcinosis in juvenile dermatomyositis. Indian Pediatr. 2008;45:784.
Salum AME, Pivato FCMM, Doria-Filho U, et al. Risk factors associated with calcinosis of juvenile dermatomyositis. J Pediatr. 2008;84:68–74. https://doi.org/10.2223/JPED.1746.
Wu JJ, Metz BJ. Calcinosis cutis of juvenile dermatomyositis treated with incision and drainage. Dermatol Surg. 2008;34:575–7. https://doi.org/10.1111/j.1524-4725.2007.34106.x.
Constatin T, Ponyi A, Orbán I, et al. National registry of patients with juvenile idiopathic inflammatory myopathies in Hungary-clinical characteristics and disease course of 44 patients with juvenile dermatomyositis. Autoimmunity. 2006;39:223–32. https://doi.org/10.1080/08916930600622819.
Chiu SK, Yang YH, Wang LC, Chiang BL. Ten-year experience of juvenile dermatomyositis: a retrospective study. J Microbiol Immunol Infect. 2007;40:68–73.
Pachman LM, Veis A, Stock S, et al. Composition of calcifications in children with juvenile dermatomyositis: association with chronic cutaneous inflammation. Arthritis Rheum. 2006;54:3345–50. https://doi.org/10.1002/art.22158.
Singh S, Bansal A. Twelve years experience of juvenile dermatomyositis in North India. Rheumatol Int. 2006;26:510–5. https://doi.org/10.1007/s00296-005-0030-2.
Briso-Montiano ME, Sánchez PS, Velasco MB, et al. Juvenile amyopathic dermatomyositis and calcinosis. An Pediatr (Barc). 2005;62:286–8. https://doi.org/10.1157/13071846.
Sallum AM, Kiss MHB, Sachetti S, et al. Juvenile dermatomyositis: clinical, laboratorial, histological, therapeutical and evolutive parameters of 35 patients. Arq Neuropsiquiatr. 2022;60:889–99. https://doi.org/10.1590/S0004-282X2002000600001.
Harel L, Harel G, Korenreich L, Straussberg R, Amir J. Treatment of calcinosis in juvenile dermatomyositis with probenecid: the role of phosphorus metabolism in the development of calcifications. J Rheumatol. 2001;28:1129–32.
Mukamel M, Horev G, Mimouni M. New insight into calcinosis of juvenile dermatomyositis: a study of composition and treatment. J Pediatr. 2001;138:763–6. https://doi.org/10.1067/mpd.2001.112473.
•• Huber AM, Lang B, LeBlanc CM, et al. Medium- and long-term functional outcomes in a multicenter cohort of children with juvenile dermatomyositis. Arthritis Rheum. 2000;43:541–9. https://doi.org/10.1002/1529-0131(200003)43:3%3c541::AID-ANR9%3e3.0.CO;2-T. This study describes a cohort that helps understand the natural history of the disease.
Pachman LM, Hayford JR, Chung A, et al. Juvenile dermatomyositis at diagnosis: clinical characteristics of 79 children. J Rheumatol. 1998;25:1198–204.
Kobayashi S, Higuchi K, Tamaki H, et al. Characteristics of juvenile dermatomyositis in Japan. Pediatr Int. 1997;39:257–62. https://doi.org/10.1111/j.1442-200x.1997.tb03595.x.
Wanakul S, Pongprasit P, Wattakankrai P. Calcinosis cutis presenting years before other clinical manifestations of juvenile dermatomyositis: report of two cases. Australas J Dermatol. 1997;38:202–5. https://doi.org/10.1111/j.1440-0960.1997.tb01698.x.
Oliveri MB, Palermo R, Mautalen C, Hübscher O. Regression of calcinosis during diltiazem treatment in juvenile dermatomyositis. J Rheumatol. 1996;23:2152–5.
Nakagawa T, Taikawa T. Calcinosis cutis in juvenile dermatomyositis responsive to aluminum hydroxide treatment. J Dermatol. 1993;20:558–90. https://doi.org/10.1111/j.1346-8138.1993.tb01338.x.
Agud-Dios M, Arroyo-Andres J, Rubio-Muñiz C, et al. Juvenile dermatomyositis-associated calcinosis successfully treated with combined immunosuppressive, bisphosphonate, oral baricitinib and physical therapy. Dermatol Ther. 2022;35: e15960. https://doi.org/10.1111/dth.15960.
Funding
The authors have received no funding.
Author information
Authors and Affiliations
Contributions
All authors carried out the collection, analysis, discussion and final appreciation of the paper.
Corresponding author
Ethics declarations
Human and Animal Rights Statement
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gonçalves Júnior, J., Shinjo, S.K. Calcinosis in Juvenile Dermatomyositis—Epidemiology, Pathogenesis, Clinical Features, and Treatment: A Systematic Review. Curr Rheumatol Rep 26, 53–68 (2024). https://doi.org/10.1007/s11926-023-01126-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11926-023-01126-5