Abstract
Purpose of Review
To provide consultation–liaison psychiatrists with an updated resource that can assist in the treatment and management of geriatric patients.
Recent Findings
The current available literature has not shown any differences in efficacy between haloperidol and second-generation antipsychotics in patients with delirium. When considering relative advantages of forms of antipsychotic administration, there is no support for a superior safety profile of oral compared to intramuscular or intravenous administration. A recent meta-analysis of four randomized controlled trials concluded that when melatonin was administered to older age patients on medical wards, it significantly prevented the incidence of delirium when compared with the control group. While suvorexant administered nightly to elderly patients in acute care settings may lower the incidence of delirium, larger studies are needed to confirm this finding. Despite the black box warning of increased mortality risk in older patients with dementia, antipsychotics may be used with caution by the consultation–liaison (CL) psychiatrist to treat the neuropsychologic symptoms of dementia including hallucinations and psychosis in the hospital setting. While antidepressant studies have focused primarily on citalopram and escitalopram in the treatment of agitation in the setting of dementia, these two medications have not been adequately compared directly to other SSRIs for this condition. It is therefore not clear whether citalopram and escitalopram are more efficacious in treating agitation in the setting of dementia when compared to other SSRIs. While the evidence supporting trazodone’s use is limited, it is generally well tolerated and is an option as a PRN for irritability and agitation in patients with Alzheimer’s and mixed dementia. While there is some evidence to support the use of acetylcholinesterase inhibitors for treating cognitive impairments and hallucinations in Lewy body dementia, the usefulness of these agents in other forms of dementia is not well studied, and those studies did not show any benefit in the management of acute agitation. It is important to note that memantine can cause or exacerbate agitation and may be the cause of behavioral dysregulation. There is no evidence to support the routine use of benzodiazepines for behavioral improvement in patients with dementia. Escitalopram and citalopram do have a unique pharmacokinetic properties in the sense that they have been found to have 50–56% plasma protein binding, compared to sertraline, fluoxetine, and paroxetine (95% or more). Pooled analyses suggest that antidepressants are more effective than placebo in reducing the symptoms of post-stroke depression. SSRIs are considered first-line antidepressants in stroke patients, who are often elderly with underlying cardiovascular problems. Although treatment with SSRIs is recommended for post-stroke depression, there are no studies providing conclusive data on the superiority of a specific drug. Older age is associated with a better outcome from ECT, with remission rates of approximately 73% to 90% in patients over 65 years. ECT is the treatment of choice for patients with psychotic depression, and elderly patients with psychotic depression have been shown to have a higher remission rate and faster time to response than depressed patients without psychotic symptoms.
Summary
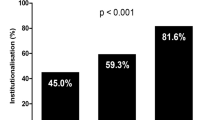
With the average life expectancy increase, it is projected that 19 million people will reach the age of 85 or higher, an increase from 5.5 million in 2010. With an increasing older population, psychiatric consultation in the management of geriatric patients is becoming more necessary. Psychiatrists must be aware of the unique considerations in elderly patients. In this article, we provide evidence-based guidance to the CL psychiatrist on major issues relating to the older age patient, highlighting recent trends in treatment. First, we provide background on the evaluation of the medically hospitalized geriatric patient. As rates of medical and psychiatric illnesses increase with advancing age, elderly patients are more likely to be taking a higher number of medications as compared to younger patients, and physicians must pay special attention to polypharmacy, including side effects and drug interactions in this group. Next, we focus on the diagnosis, management, and unique needs of the geriatric patient presenting with common clinical syndromes of delirium, dementia, and depression. Delirium and dementia are among the most common causes of cognitive impairment in clinical settings yet are often either unrecognized or misdiagnosed as they may have similar signs and symptoms. In addition, depression is prevalent in older adults, especially in those with comorbid medical illness. Depression can be fatal as the rates of suicide are higher in later life than in any other age group. Consultation can improve the management of elderly patients and prevent unnecessary nursing home placement.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Stern TA, Fricchione GL, Cassem NH, Jellinke MS, Rosenbaum JF. Massachusetts general hospital handbook of general hospital psychiatry. 6th ed. Philadelphia, PA: Saunders, Elsevier; 2010.
Hybels C, Blazer D. Demography and epidemiology of psychiatric disorders in late life. In: Steffens D, Blazer D, Thakur M, editors. The American Psychiatric Publishing Textbook of Geriatric Psychiatry. Fifth ed. Arlington, VA: American Psychiatric Publishing; 2015. p. 22209–3901.
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43.
Ng TP, Feng L, Chiam PC, Kua EH. Psychiatric morbidity and acute hospitalization in elderly people. Int Psychogeriatr. 2006;18(4):701–11.
Brahma DK, Wahlang JB, Marak MD, Ch Sangma M. Adverse drug reactions in the elderly. J Pharmacol Pharmacother. 2013;4(2):91–4.
Levenson JL. The American Psychiatric Association Publishing textbook of psychosomatic medicine and consultation-liaison psychiatry. Third ed. Washington, D.C.: American Psychiatric Association Publishing; 2018.
Fountoulakis KN, O'Hara R, Iacovides A, Camilleri CP, Kaprinis S, Kaprinis G, et al. Unipolar late-onset depression: a comprehensive review. Ann Gen Hosp Psychiatry. 2003;2(1):11.
Nardone R, Holler Y, Storti M, Christova M, Tezzon F, Golaszewski S, et al. Thiamine deficiency induced neurochemical, neuroanatomical, and neuropsychological alterations: a reappraisal. ScientificWorldJournal. 2013;2013:309143.
Mikkelsen K, Stojanovska L, Apostolopoulos V. The effects of vitamin B in depression. Curr Med Chem. 2016;23(38):4317–37.
Hermida AP, Janjua AU, Glass OM, Vaughan CP, Goldstein F, Trotti LM, et al. A case of lithium-induced parkinsonism presenting with typical motor symptoms of Parkinson’s disease in a bipolar patient. Int Psychogeriatr. 2016;28(12):2101–4.
Hijazi Z, Lange P, Watson R, Maier AB. The use of cerebral imaging for investigating delirium aetiology. Eur J Intern Med. 2018;52:35–9.
Olszewska DA, Costello DJ. Assessment of the usefulness of magnetic resonance brain imaging in patients presenting with acute seizures. Ir J Med Sci. 2014;183(4):621–4.
Lovblad KO, Altrichter S, Mendes Pereira V, Vargas M, Marcos Gonzalez A, Haller S, et al. Imaging of acute stroke: CT and/or MRI. J Neuroradiol. 2015;42(1):55–64.
Tombaugh TN, McIntyre NJ. The mini-mental state examination: a comprehensive review. J Am Geriatr Soc. 1992;40(9):922–35.
Smith T, Gildeh N, Holmes C. The Montreal Cognitive Assessment: validity and utility in a memory clinic setting. Can J Psychiatr. 2007;52(5):329–32.
•• Fisher TJ, Schwartz AC, Greenspan HN, Heinrich TW. Dementia: a complex disease with multiple etiologies and multiple treatments. Int J Psychiatry Med. 2016;51(2):171–81. This article discusses practical methods for monitoring the progression of dementia.
Irwin SA, Pirrello RD, Hirst JM, Buckholz GT, Ferris FD. Clarifying delirium management: practical, evidenced-based, expert recommendations for clinical practice. J Palliat Med. 2013;16(4):423–35.
Downing LJ, Caprio TV, Lyness JM. Geriatric psychiatry review: differential diagnosis and treatment of the 3 D’s - delirium, dementia, and depression. Curr Psychiatry Rep. 2013;15(6):365.
Milton JC, Hill-Smith I, Jackson SH. Prescribing for older people. BMJ (Clin Res Ed). 2008;336(7644):606–9.
Frank C. Pharmacologic treatment of depression in the elderly. Can Fam Physician. 2014;60(2):121–6.
Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911–22.
Schwartz AC, Fisher TJ, Greenspan HN, Heinrich TW. Pharmacologic and nonpharmacologic approaches to the prevention and management of delirium. Int J Psychiatry Med. 2016;51(2):160–70.
van Velthuijsen EL, Zwakhalen SMG, Mulder WJ, Verhey FRJ, Kempen G. Detection and management of hyperactive and hypoactive delirium in older patients during hospitalization: a retrospective cohort study evaluating daily practice. Int J Geriatr Psychiatry. 2018;33(11):1521–9.
Morandi A, Di Santo SG, Cherubini A, Mossello E, Meagher D, Mazzone A, et al. Clinical features associated with delirium motor subtypes in older inpatients: results of a multicenter study. Am J Geriatr Psychiatry. 2017;25(10):1064–71.
Wei LA, Fearing MA, Sternberg EJ, Inouye SK. The Confusion Assessment Method: a systematic review of current usage. J Am Geriatr Soc. 2008;56(5):823–30.
Brown TM. Drug-induced delirium. Semin Clin Neuropsychiatry. 2000;5(2):113–24.
Markowitz JD, Narasimhan M. Delirium and antipsychotics: a systematic review of epidemiology and somatic treatment options. Psychiatry (Edgmont). 2008;5(10):29–36.
Gilmore ML, Wolfe DJ. Antipsychotic prophylaxis in surgical patients modestly decreases delirium incidence--but not duration--in high-incidence samples: a meta-analysis. Gen Hosp Psychiatry. 2013;35(4):370–5.
Schrijver EJ, de Vries OJ, Verburg A, de Graaf K, Bet PM, van de Ven PM, et al. Efficacy and safety of haloperidol prophylaxis for delirium prevention in older medical and surgical at-risk patients acutely admitted to hospital through the emergency department: study protocol of a multicenter, randomised, double-blind, placebo-controlled clinical trial. BMC Geriatr. 2014;14:96.
Neufeld KJ, Yue J, Robinson TN, Inouye SK, Needham DM. Antipsychotic medication for prevention and treatment of delirium in hospitalized adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2016;64(4):705–14.
•• Maldonado JR. Acute brain failure: pathophysiology, diagnosis, management, and sequelae of delirium. Crit Care Clin. 2017;33(3):461–519. This reference discusses the similar efficacy shared between haloperidol and second-generation antipsychotics in patients with delirium.
Narang P, El-Refai M, Parlapalli R, Danilov L, Manda S, Kaur G, et al. Antipsychotic drugs: sudden cardiac death among elderly patients. Psychiatry (Edgmont). 2010;7(10):25–9.
Meyer-Massetti C, Cheng CM, Sharpe BA, Meier CR, Guglielmo BJ. The FDA extended warning for intravenous haloperidol and torsades de pointes: how should institutions respond? J Hosp Med. 2010;5(4):E8–16.
Oh ES, Fong TG, Hshieh TT, Inouye SK. Delirium in older persons: advances in diagnosis and treatment. JAMA. 2017;318(12):1161–74.
Bakken MS, Schjott J, Engeland A, Engesaeter LB, Ruths S. Antipsychotic drugs and risk of hip fracture in people aged 60 and older in Norway. J Am Geriatr Soc. 2016;64(6):1203–9.
Stroup TS, Gray N. Management of common adverse effects of antipsychotic medications. World Psychiatry. 2018;17(3):341–56.
Tisdale JE, Rasty S, Padhi ID, Sharma ND, Rosman H. The effect of intravenous haloperidol on QT interval dispersion in critically ill patients: comparison with QT interval prolongation for assessment of risk of Torsades de Pointes. J Clin Pharmacol. 2001;41(12):1310–8.
Attard A, Ranjith G, Taylor D. Delirium and its treatment. CNS Drugs. 2008;22(8):631–44.
Lonergan E, Luxenberg J, Areosa Sastre A, Wyller TB. Benzodiazepines for delirium. Cochrane Database Syst Rev. 2009;1:CD006379.
Zaal IJ, Devlin JW, Hazelbag M, Klein Klouwenberg PM, van der Kooi AW, Ong DS, et al. Benzodiazepine-associated delirium in critically ill adults. Intensive Care Med. 2015;41(12):2130–7.
Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009;5(4):210–20.
Bellapart J, Boots R. Potential use of melatonin in sleep and delirium in the critically ill. Br J Anaesth. 2012;108(4):572–80.
Artemiou P, Bily B, Bilecova-Rabajdova M, Sabol F, Torok P, Kolarcik P, et al. Melatonin treatment in the prevention of postoperative delirium in cardiac surgery patients. Kardiochir Torakochirurgia Pol. 2015;12(2):126–33.
• Chen S, Shi L, Liang F, Xu L, Desislava D, Wu Q, et al. Exogenous melatonin for delirium prevention: a meta-analysis of randomized controlled trials. Mol Neurobiol. 2016;53(6):4046–53. This study presents evidence supporting the use of melatonin to prevent delirium in high-risk older age patients.
Inoue T, Morita M, Wada A, Kasai K, Kondo S. A case of persistent delirium resolved promptly with suvorexant. Prim Care Companion CNS Disord. 2017;19(2).
Hatta K, Kishi Y, Wada K, Takeuchi T, Ito S, Kurata A, et al. Preventive effects of suvorexant on delirium: a randomized placebo-controlled trial. J Clin Psychiatry. 2017.
Masuyama T, Sanui M, Yoshida N, Iizuka Y, Ogi K, Yagihashi S, et al. Suvorexant is associated with a low incidence of delirium in critically ill patients: a retrospective cohort study. Psychogeriatrics : the official journal of the Japanese Psychogeriatric Society. 2018;18(3):209–15.
Hugo J, Ganguli M. Dementia and cognitive impairment: epidemiology, diagnosis, and treatment. Clin Geriatr Med. 2014;30(3):421–42.
Hope T, Keene J, Fairburn C, McShane R, Jacoby R. Behaviour changes in dementia. 2: are there behavioural syndromes? Int J Geriatr Psychiatry. 1997;12(11):1074–8.
Kales HC, Gitlin LN, Lyketsos CG. Management of neuropsychiatric symptoms of dementia in clinical settings: recommendations from a multidisciplinary expert panel. J Am Geriatr Soc. 2014;62(4):762–9.
Fong TG, Davis D, Growdon ME, Albuquerque A, Inouye SK. The interface between delirium and dementia in elderly adults. Lancet Neurol. 2015;14(8):823–32.
Gustafsson M, Karlsson S, Gustafson Y, Lövheim H. Psychotropic drug use among people with dementia--a six-month follow-up study. BMC Pharmacol Toxicol. 2013;14:56.
Devanand DP, Pelton GH, Cunqueiro K, Sackeim HA, Marder K. A 6-month, randomized, double-blind, placebo-controlled pilot discontinuation trial following response to haloperidol treatment of psychosis and agitation in Alzheimer’s disease. Int J Geriatr Psychiatry. 2011;26(9):937–43.
Dorsey ER, Rabbani A, Gallagher SA, Conti RM, Alexander GC. Impact of FDA black box advisory on antipsychotic medication use. Arch Intern Med. 2010;170(1):96–103.
Kuehn BM. FDA: antipsychotics risky for elderly. JAMA. 2008;300(4):379–80.
Steinberg M, Lyketsos CG. Atypical antipsychotic use in patients with dementia: managing safety concerns. Am J Psychiatry. 2012;169(9):900–6.
Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA. 2005;294(15):1934–43.
Lonergan E, Luxenberg J, Colford J. Haloperidol for agitation in dementia. Cochrane Database Syst Rev. 2001;(4):Cd002852.
De Deyn PP, Buitelaar J. Risperidone in the management of agitation and aggression associated with psychiatric disorders. Eur Psychiatry. 2006;21(1):21–8.
Tampi RR, Tampi DJ, Balachandran S, Srinivasan S. Antipsychotic use in dementia: a systematic review of benefits and risks from meta-analyses. Ther Adv Chronic Dis. 2016;7(5):229–45.
Schneider LS, Tariot PN, Dagerman KS, Davis SM, Hsiao JK, Ismail MS, et al. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer’s disease. N Engl J Med. 2006;355(15):1525–38.
Schneider LS, Dagerman K, Insel PS. Efficacy and adverse effects of atypical antipsychotics for dementia: meta-analysis of randomized, placebo-controlled trials. Am J Geriatr Psychiatry. 2006;14(3):191–210.
Porsteinsson AP, Keltz MA, Smith JS. Role of citalopram in the treatment of agitation in Alzheimer’s disease. Neurodegenerative Dis Manag. 2014;4(5):345–9.
Hutton LMJ, Cave AJ, St-Jean R, Banh HL. Should we be worried about QTc prolongation using citalopram? A Review. J Pharm Pract. 2017;30(3):353–8.
Do A, Noohi S, Elie D, Mahdanian AA, Yu C, Segal M, et al. Health Canada warning on citalopram and escitalopram--its effects on prescribing in consultation-liaison psychiatry. Psychosomatics. 2016;57(1):57–63.
Drye LT, Spragg D, Devanand DP, Frangakis C, Marano C, Meinert CL, et al. Changes in QTc interval in the citalopram for agitation in Alzheimer’s disease (CitAD) randomized trial. PLoS One. 2014;9(6):e98426.
Carceller-Sindreu M, de Diego-Adelino J, Portella MJ, Garcia-Moll X, Figueras M, Fernandez-Vidal A, et al. Lack of relationship between plasma levels of escitalopram and QTc-interval length. Eur Arch Psychiatry Clin Neurosci. 2017.
Davies SJ, Burhan AM, Kim D, Gerretsen P, Graff-Guerrero A, Woo VL, et al. Sequential drug treatment algorithm for agitation and aggression in Alzheimer’s and mixed dementia. J Psychopharmacol (Oxford, England). 2018;32(5):509–23.
Lopez-Pousa S, Garre-Olmo J, Vilalta-Franch J, Turon-Estrada A, Pericot-Nierga I. Trazodone for Alzheimer’s disease: a naturalistic follow-up study. Arch Gerontol Geriatr. 2008;47(2):207–15.
Aisen PS, Johannessen DJ, Marin DB. Trazodone for behavioral disturbance in Alzheimer’s disease. Am J Geriatr Psychiatry. 1993;1(4):349–50.
Lebert F, Stekke W, Hasenbroekx C, Pasquier F. Frontotemporal dementia: a randomised, controlled trial with trazodone. Dement Geriatr Cogn Disord. 2004;17(4):355–9.
Trinh NH, Hoblyn J, Mohanty S, Yaffe K. Efficacy of cholinesterase inhibitors in the treatment of neuropsychiatric symptoms and functional impairment in Alzheimer disease: a meta-analysis. JAMA. 2003;289(2):210–6.
Tariot PN, Farlow MR, Grossberg GT, Graham SM, McDonald S, Gergel I, et al. Memantine treatment in patients with moderate to severe Alzheimer disease already receiving donepezil: a randomized controlled trial. JAMA. 2004;291(3):317–24.
Velayudhan L, Ffytche D, Ballard C, Aarsland D. New therapeutic strategies for Lewy body dementias. Curr Neurol Neurosci Rep. 2017;17(9):68.
Ukai K, Fujishiro H, Iritani S, Ozaki N. Long-term efficacy of donepezil for relapse of visual hallucinations in patients with dementia with Lewy bodies. Psychogeriatrics : the official journal of the Japanese Psychogeriatric Society. 2014.
Da Re F, Rucci F, Isella V. Retrospective study on agitation provoked by memantine in dementia. J Neuropsychiatry Clin Neurosci. 2015;27(1):e10–3.
Unutzer J, Simon G, Belin TR, Datt M, Katon W, Patrick D. Care for depression in HMO patients aged 65 and older. J Am Geriatr Soc. 2000;48(8):871–8.
Callahan CM, Hendrie HC, Nienaber NA, Tierney WM. Suicidal ideation among older primary care patients. J Am Geriatr Soc. 1996;44(10):1205–9.
Waern M, Rubenowitz E, Runeson B, Skoog I, Wilhelmson K, Allebeck P. Burden of illness and suicide in elderly people: case-control study. BMJ (Clin Res Ed). 2002;324(7350):1355.
Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol. 2009;5:363–89.
Koenig HG, George LK. Depression and physical disability outcomes in depressed medically ill hospitalized older adults. Am J Geriatr Psychiatry. 1998;6(3):230–47.
Muliyala KP, Varghese M. The complex relationship between depression and dementia. Ann Indian Acad Neurol. 2010;13(Suppl 2):S69–73.
Kok RM, Reynolds CF 3rd. Management of depression in older adults: a review. Jama. 2017;317(20):2114–22.
Kang H, Zhao F, You L, Giorgetta C, Venkatesh D, Sarkhel S, et al. Pseudo-dementia: a neuropsychological review. Ann Indian Acad Neurol. 2014;17(2):147–54.
Steffens DC. Late-life depression and the prodromes of dementia. JAMA Psychiatry. 2017;74(7):673–4.
Neubauer AB, Wahl HW, Bickel H. Depressive symptoms as predictor of dementia versus continuous cognitive decline: a 3-year prospective study. Eur J Ageing. 2013;10(1):37–48.
Franchini L, Serretti A, Gasperini M, Smeraldi E. Familial concordance of fluvoxamine response as a tool for differentiating mood disorder pedigrees. J Psychiatr Res. 1998;32(5):255–9.
Gelhorn HL, Sexton CC, Classi PM. Patient preferences for treatment of major depressive disorder and the impact on health outcomes: a systematic review. Prim Care Companion CNS Disord. 2011;13(5).
Hawton K, Bergen H, Simkin S, Cooper J, Waters K, Gunnell D, et al. Toxicity of antidepressants: rates of suicide relative to prescribing and non-fatal overdose. Br J Psychiatry. 2010;196(5):354–8.
van Harten J. Clinical pharmacokinetics of selective serotonin reuptake inhibitors. Clin Pharmacokinet. 1993;24(3):203–20.
Rao N. The clinical pharmacokinetics of escitalopram. Clin Pharmacokinet. 2007;46(4):281–90.
Westenberg HG, Sandner C. Tolerability and safety of fluvoxamine and other antidepressants. Int J Clin Pract. 2006;60(4):482–91.
• Villa RF, Ferrari F, Moretti A. Post-stroke depression: mechanisms and pharmacological treatment. Pharmacol Ther. 2018;184:131–44. This study emphasizes the impact of post-stroke depression on cognitive recovery, functional outcomes, and quality of life.
Chen Y, Patel NC, Guo JJ, Zhan S. Antidepressant prophylaxis for poststroke depression: a meta-analysis. Int Clin Psychopharmacol. 2007;22(3):159–66.
Mead GE, Hsieh CF, Hackett M. Selective serotonin reuptake inhibitors for stroke recovery. Jama. 2013;310(10):1066–7.
Xu XM, Zou DZ, Shen LY, Liu Y, Zhou XY, Pu JC, et al. Efficacy and feasibility of antidepressant treatment in patients with post-stroke depression. Medicine. 2016;95(45):e5349.
Paolucci S. Advances in antidepressants for treating post-stroke depression. Expert Opin Pharmacother. 2017;18(10):1011–7.
Esparrago Llorca G, Castilla-Guerra L, Fernandez Moreno MC, Ruiz Doblado S, Jimenez Hernandez MD. Post-stroke depression: an update. Neurologia (Barcelona, Spain). 2015;30(1):23–31. This study provides support for SSRIs as a first-line treatment modality in post-stroke depression.
Tirmizi O, Raza A, Trevino K, Husain MM. Electroconvulsive therapy: how modern techniques improve patient outcomes: refinements have decreased memory loss, other adverse effects while retaining efficacy: refinements have decreased memory loss, other adverse effects while retaining efficacy. Curr Psychiatr Ther. 2012;11(10):24–46.
•• Hermida AP, Glass OM, Shafi H, McDonald WM. Electroconvulsive therapy in depression: current practice and future direction. Psychiatr Clin North Am. 2018;41(3):341–53. This reference highlights the improved safety and tolerability of ECT in the last several years.
Riva-Posse P, Hermida AP, McDonald WM. The role of electroconvulsive and neuromodulation therapies in the treatment of geriatric depression. Psychiatr Clin North Am. 2013;36(4):607–30.
O'Connor MK, Knapp R, Husain M, Rummans TA, Petrides G, Smith G, et al. The influence of age on the response of major depression to electroconvulsive therapy: a C.O.R.E. Report. Am J Geriatr Psychiatry. 2001;9(4):382–90.
Petrides G, Fink M, Husain MM, Knapp RG, Rush AJ, Mueller M, et al. ECT remission rates in psychotic versus nonpsychotic depressed patients: a report from CORE. J ECT. 2001;17(4):244–53.
Kellner CH, Fink M, Knapp R, Petrides G, Husain M, Rummans T, et al. Relief of expressed suicidal intent by ECT: a consortium for research in ECT study. Am J Psychiatry. 2005;162(5):977–82.
Fink M, Kellner CH, McCall WV. Optimizing ECT technique in treating catatonia. J ECT. 2016;32(3):149–50.
Hermida AP, Tang YL, Glass O, Janjua AU, McDonald WM. Efficacy and safety of ECT for Behavioral and Psychological Symptoms of Dementia (BPSD): a retrospective chart review. Am J Geriatr Psychiatry. 2020;28(2):157–63.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Oliver M. Glass, Adriana P. Hermida, Rachel Hershenberg, and Ann C. Schwartz each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Geriatric Disorders
Rights and permissions
About this article
Cite this article
Glass, O.M., Hermida, A.P., Hershenberg, R. et al. Considerations and Current Trends in the Management of the Geriatric Patient on a Consultation–Liaison Service. Curr Psychiatry Rep 22, 21 (2020). https://doi.org/10.1007/s11920-020-01147-2
Published:
DOI: https://doi.org/10.1007/s11920-020-01147-2