Abstract
Measuring biological sex differences and socio-cultural gender diversity provides insights into individual variation in stress physiology and the development of “sex-specific” diseases.
Purpose of Review
In this selective review, we summarize recent findings that assess sex and gender in relation to the stress hormone cortisol and multi-systemic physiological dysregulation called allostatic load. The focus of this research centers on workers as well as sexual and gender minorities as these populations provide unique insights into sex and gender at various levels of analysis from the micro-level to the macro-level.
Recent Findings
Male/female sex, sex hormones, gender identity, gender roles, and sexual orientation are all variables that are distinctly correlated with stress physiology. Beyond identifying patterns of vulnerability to stress-related diseases, pathways towards resilience are of high priority in emerging literature.
Summary
Stress scientists must account for both sex and gender in biobehavioral research. Future directions should assess macro-level constructs like institutionalized gender, occupational sex composition, and structural stigma to better understand the social determinants of health.






Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Joel D, McCarthy MM. Incorporating sex as a biological variable in neuropsychiatric research: where are we now and where should we be? Neuropsychopharmacology. 2017;42(2):379–85. Excellent dialogue and reflections by two leading researchers on sex differences in neuropsychiatry with solid recommendations for the future.
Plotnikoff R. Women, heart disease and stroke in Canada: issues and options. Ottawa: Heart and Stroke Foundation of Canada; 1997.
Regitz-Zagrosek V. Sex and gender differences in health. Science & Society Series on Sex and Science. EMBO Rep. 2012;13(7):596–603.
Johnson, J.L., Greaves, L., & Repta, R. Better Science with Sex and Gender: a primer for health research. In. Edited by Women’s Health Research Network. Vancouver, British-Columbia, Canada; 2007. http://bccewh.bc.ca/wp-content/uploads2012/05/2007_BetterSciencewithSexandGenderPrimerforHealthResearch.pdf.
Bem SL. On the utility of alternative procedures for assessing psychological androgyny. J Consult Clin Psychol. 1977;45(2):196–205.
McEwen BS. Allostasis and the epigenetics of brain and body health over the life course: the brain on stress. JAMA Psychiatry. 2017;74(6):551–2.
Taylor SE, Klein LC, Lewis BP, Gruenewald TL, Gurung RA, Updegraff JA. Biobehavioral responses to stress in females: tend-and-befriend, not fight-or-flight. Psychol Rev. 2000;107(3):411–29.
Klein SL, Schiebinger L, Stefanick ML, Cahill L, Danska J, de Vries GJ, et al. Opinion: sex inclusion in basic research drives discovery. Proc Natl Acad Sci U S A. 2015;112(17):5257–8.
Kirschbaum C, Wust S, Hellhammer D. Consistent sex differences in cortisol responses to psychological stress. Psychosom Med. 1992;54(6):648–57.
Kirschbaum C, Pirke KM, Hellhammer DH. The ‘Trier social stress Test’--a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology. 1993;28(1–2):76–81.
Stroud LR, Tanofsky-Kraff M, Wilfley DE, Salovey P. The Yale Interpersonal Stressor (YIPS): affective, physiological, and behavioral responses to a novel interpersonal rejection paradigm. Ann Behav Med. 2000;22(3):204–13.
Stroud LR, Salovey P, Epel ES. Sex differences in stress responses: social rejection versus achievement stress. Biol Psychiatry. 2002;52(4):318–27.
Kajantie E, Phillips DI. The effects of sex and hormonal status on the physiological response to acute psychosocial stress. Psychoneuroendocrinology. 2006;31(2):151–78.
• Juster RP, Raymond C, Desrochers AB, et al. Sex hormones adjust “sex-specific” reactive and diurnal cortisol profiles. Psychoneuroendocrinology. 2016;63:282–90. Study demonstrates that adjusting for salivary testosterone, estradiol, and progesterone concentrations in both sexes unmasks higher diurnal cortisol among women and eliminates sex differences in cortisol reactivity.
• Juster RP, Almeida D, Cardoso C, et al. Gonads and strife: sex hormones vary according to sexual orientation for women and stress indices for both sexes. Psychoneuroendocrinology. 2016;72:119–30. Study showing that lesbian/bisexual women show higher testosterone and progesterone than heterosexual women and these sex hormone profiles are correlated with biopsychosocial indices.
Sterling P, Eyer J. Allostasis: a new paradigm to explain arousal pathology. In: Fisher S, Reason J, editors. Handbook of life stress, cognition and health. New York: John Wiley & Sons; 1988. p. 629–49.
McEwen BS, Lasley EN. The end of stress as we know it. Washington, D.C.: Joseph Henry Press; 2002.
Koob GF, Le Moal M. Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology. 2001;24(2):97–129.
McEwen BS, Stellar E. Stress and the individual. Mechanisms leading to disease. Arch Intern Med. 1993;153(18):2093–101.
Seeman E, Singer BH, Rowe J, Horwitz RI, McEwen B. Price of adaptation - allostatic load and its health consequences. Arch Intern Med. 1997;157:2259–68.
Seeman TE, Singer BH, Rowe JW, Horwitz RI, McEwen BS. Price of adaptation--allostatic load and its health consequences. MacArthur studies of successful aging. Arch Intern Med. 1997;157(19):2259–68.
McCaffery JM, Marsland AL, Strohacker K, Muldoon MF, Manuck SB. Factor structure underlying components of allostatic load. PLoS One. 2012;7(10):e47246.
Beckie TM. A systematic review of allostatic load, health, and health disparities. Biological research for nursing. 2012;14(4):311–46.
Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci Biobehav Rev. 2010;35(1):2–16.
Singer B, Ryff CD, Seeman T. Operationalizing allostatic load. In: Schulkin J, editor. Allostasis, homeostasis, and the costs of psychological adaptation. New York: Cambridge University Press; 2004. p. 113–49.
• Juster RP, Russell JJ, Almeida D, Picard M. Allostatic load and comorbidities: a mitochondrial, epigenetic, and evolutionary perspective. Development & Psychopathology. 2016;28(4pt1):1117–46. Selective review of allostatic load and comorbidities.
Juster RP, Bizik G, Picard M, Arsenault-Lapierre G, Sindi S, Trepanier L, et al. A transdisciplinary perspective of chronic stress in relation to psychopathology throughout life span development. Dev Psychopathol. 2011;23(3):725–76.
Juster RP, Seeman T, McEwen BS, et al. Social inequalities and the road to allostatic load: from vulnerability to resilience. In: Cicchetti D, editor. Developmental psychopathology handbook. Third edn. Cambridge: Cambridge Press; 2016.
Crews DE, Harada H, Aoyagi K, Maeda T, Alfarano A, Sone Y, et al. A pilot study of allostatic load among elderly Japanese living on Hizen-Oshima Island. J Physiol Anthropol. 2012;31:18.
Juster RP, Lupien SJ. Chronic stress and allostatic load. In: Schenck-Gustafsson K, DeCola PR, Pfaff DW, Pisetsky DS, editors. Handbook of clinical gender medicine. Basel: Karger AG; 2012. p. 70–81.
Lundberg U. Stress hormones in health and illness: the roles of work and gender. Psychoneuroendocrinology. 2005;30:1017–21.
Seeman T, Glei D, Goldman N, Weinstein M, Singer B, Lin YH. Social relationships and allostatic load in Taiwanese elderly and near elderly. Soc Sci Med. 2004;59(11):2245–57.
Kubzansky LD, Kawachi I, Sparrow D. Socioeconomic status, hostility, and risk factor clustering in the Normative Aging Study: any help from the concept of allostatic load? Ann Behav Med. 1999;21(4):330–8.
Sun J, Wang S, Zhang JQ, Li W. Assessing the cumulative effects of stress: the association between job stress and allostatic load in a large sample of Chinese employees. Work Stress. 2007;21(4):333–47.
WHO. Gender equality, work and health: a review of the evidence. Geneva: World Health Organization; 2006.
Lundberg U, Frankenhaeuser M. Stress and workload of men and women in high-ranking positions. J Occup Health Psychol. 1999;4(2):142–51.
Lupien SJ, Ouellet-Morin I, Hupbach A, et al. Beyond the stress concept: allostatic load - a developmental biological and cognitive perspective. In: Cicchetti D, editor. Handbook series on developmental psychopathology. Hoboken: Wiley; 2006. p. 784–809.
Clow BN, Dederson A, Haworth-Brockman M, Bernier J. Rising to the challenge: sex- and gender-based analysis of health planning, policy and research in Canada. Halifax: Atlantic Centre of Excellent for Women’s Health; 2009.
Frankenhaeuser M. Stress and gender. European Review. 1996;4:313–27.
• Pelletier R, Ditto B, Pilote L: A composite measure of gender and its association with risk factors in patients with premature acute coronary syndrome. Psychosom Med. 2015. Creative approach to indexing gender using psychosocial data demonstrating that a greater propensity towards femininity is associated with cardiovascular disease.
Lagerlof E. Global gender issues in relation to health and industrial work. Geneva: World Health Organization; 2005.
Lundberg U. Stress hormones in health and illness: the roles of work and gender. Psychoneuroendocrinology. 2005;XX:1–5.
Juster RP, Lupien S. A sex- and gender-based analysis of allostatic load and physical complaints. Gender Medicine. 2012;9(6):511–23.
Pilote L, Dasgupta K, Guru V, Humphries KH, McGrath J, Norris C, et al. A comprehensive view of sex-specific issues related to cardiovascular disease. Can Med Assoc J. 2007;176(6):S1–S44.
Bem SL. Gender schema theory: a cogntive account of sex typing. Psychol Rev. 1981;88(4):354–64.
• Juster RP, Pruessner JC, Desrochers AB, et al. Sex and gender roles in relation to mental health and allostatic load. Psychosom Med. 2016;78(7):788–804. Study showing a sex- by gender-role interaction such that androgynous men (high masculinity and high femininty) evidence the lowest allostatic load.
• Legato MJ, Johnson PA, Manson JE. Consideration of sex differences in medicine to improve health care and patient outcomes. JAMA : the journal of the American Medical Association. 2016;316(18):1865–6. Excellent recommendations on sex as a biological variable and gender medicine.
Juster RP, Moskowitz DS, Lavoie J, D’Antono B. Sex-specific interaction effects of age, occupational status, and workplace stress on psychiatric symptoms and allostatic load among healthy Montreal workers. Stress. 2013;16(6):616–29.
United Nations: The World’s Women 2015: Trends and statistics. In. New York: United Nations, Department of Economic and Social Affairs, Statistics Division; 2015: 87–118.
Taylor CJ. occupational sex composition and the gendered availability of workplace support Gend Soc. 2010;24(2):189–212. https://doi.org/10.1177/0891243209359912.
Gross E. Plus ca change . . . ? The sexual structure of occupations over time. Soc Probl. 1968;16(2):198–208.
Richardsen AM, Traavik LEM, Burke RJ. Women and work stress: more and different? In: Connerley ML, Wu J, editors. Handbook on well-being of working women. Dordrecht: Springer Netherlands; 2016. p. 123–40.
Sobiraj S, Rigotti T, Weseler D, Mohr G. Masculinity ideology and psychological strain: considering men’s social stressors in female-dominated occupations. Psychol Men Masc. 2015;16(1):54–66.
Hensing G, Alexanderson K. The association between sex segregation, working conditions, and sickness absence among employed women. Occup Environ Med. 2004;61(2):e7.
Eriksen W, Einarsen S. Gender minority as a risk factor of exposure to bullying at work: the case of male assistant nurses. European Journal of Work and Organizational Psychology. 2004;13(4):473–92.
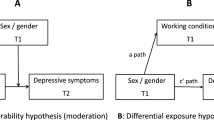
• Nyberg A, Magnusson Hanson LL, Leineweber C, Hammarstrom A, Theorell T. Occupational gender composition and mild to severe depression in a Swedish cohort: the impact of psychosocial work factors. Scandinavian Journal of Public Health. 2018;46(3):425–32. In this analysis of the Swedish Longitudinal Occupational Survey of Health, mild to severe depression appeared to vary by occupational sex composition among Swedish men but not women.
• Milner A, King T. Men’s work, women’s work and suicide: a retrospective mortality study in Australia. Aust N Z J Public Health. 2019;43(1):27–32. In this analysis of the Australian Census and the National Coronial Information System, those in male-dominated occupations experienced higher suicide rates, especially among men.
• Qian Y, Fan W: Men and women at work: occupational gender composition and affective well-being in the United States. J Happiness Stud. 2018. Study showing that working in occupations with higher percentages of male workers is associated with higher levels of unpleasantness and lower levels of meaningfulness at work for women but these associations are not significant for men.
Leijon M, Hensing G, Alexanderson K. Sickness absence due to musculoskeletal diagnoses: association with occupational gender segregation. Scandinavian Journal of Public Health. 2004;32(2):94–101. https://doi.org/10.1080/14034940310006195
Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychol Bull. 2009;135(5):707–30.
Lick DJ, Durso LE, Johnson KL. Minority stress and physical health among sexual minorities. Perspect Psychol Sci. 2013;8:521–48.
IOM. The health of lesbian, gay, bisexual, and transgender people: building a foundation for better understanding. Washinton, DC: The National Academies Press; 2011.
Lewis NM. Mental health in sexual minorities: recent indicators, trends, and their relationships to place in North America and Europe. Health Place. 2009;15(4):1029–45.
Coker TR, Austin SB, Schuster MA. The health and health care of lesbian, gay, and bisexual adolescents. Annu Rev Public Health. 2010;31:457–77.
King M, Semlyen J, Tai SS, Killaspy H, Osborn D, Popelyuk D, et al. A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry. 2008;8:70.
Brooks VR. Minority stress and lesbian women. Lexington: Lexington Books, D. C. Health and Co.; 1981.
Meyer IH. Minority stress and mental health in gay men. J Health Soc Behav. 1995;36(1):38–56.
Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–97.
Bockting WO, Miner MH, Swinburne Romine RE, Hamilton A, Coleman E. Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health. 2013;103(5):943–51.
Herek GM. Sexual stigma and sexual predudice in the United States: a conceptual framework. In: Hope DA, editor. Contemporary perspectives on lesbian, gay, and bisexual identities. New York: Springer Science + Business Media; 2009. p. 65–111.
Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–21.
Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgedner and gender nonconforming clients: an adaptation of the minority stress model. Progressional Psychology: Research and Practice. 2012;43:460–7.
Juster RP, Smith NG, Ouellet E, Sindi S, Lupien SJ. Sexual orientation and disclosure in relation to psychiatric symptoms, diurnal cortisol, and allostatic load. Psychosom Med. 2013;75(2):103–16.
Austin SB, Rosario M, McLaughlin KA, et al. Sexual orientation and diurnal cortisol patterns in a cohort of U.S. young adults. Psychoneuroendocrinology. 2016;69:197–208.
Parra LA, Benibgui M, Helm JL, Hastings PD. Minority stress predicts depression in lesbian, gay, and bisexual emerging adults via elevated diurnal cortisol. Emerging Adulthood. 2016;4:1–8.
• DuBois LZ, Powers S, Everett BG, Juster RP. Stigma and diurnal cortisol among transitioning transgender men. Psychoneuroendocrinology. 2017;82:59–66. Study showing that transgender men that experience more stigma related to transitioning, “coming out,” and public restrooms show higher diurnal cortisol than those that experience less stigma.
Huebner DM, Davis MC. Gay and bisexual men who disclose their sexual orientations in the workplace have higher workday levels of salivary cortisol and negative affect. Ann Behav Med. 2005;30(3):260–7.
• Juster RP, Hatzenbuehler ML, Mendrek A, et al. Sexual orientation modulates endocrine stress reactivity. Biol Psychiatry. 2015;77(7):668–76. Study demonstrating that gay/bisexual men show flattened cortisol reactivity and lesbian/bisexual women show amplified cortisol reactivty compared with heterosexual controls.
Juster RP, Ouellet E, Lefebvre-Louis JP, Sindi S, Johnson PJ, Smith NG, et al. Retrospective coping strategies during sexual identity formation and current biopsychosocial stress. Anxiety Stress Coping. 2016;29:119–38.
• Mays VM, Juster RP, Williamson TJ, Seeman TE, Cochran SD. Chronic physiologic effects of stress among lesbian, gay, and bisexual adults: results from the National Health and Nutrition Examination Survey. Psychosom Med. 2018;80:551–63. Study of nearly 14,000 Americans showing that gay men have the lowest allostatic load while bisexual men have the highest allostatic load compared with heterosexual men. No differences in allostatic load were detected among women by sexual orientation.
• Cook SH, Juster RP, Calebs BJ, Heinze J, Miller AL. Cortisol profiles differ by race/ethnicity among young sexual minority men. Psychoneuroendocrinology. 2017;75:1–4. Study showing that Black gay/bisexual men show elevated bedtime cortisol concentrations and flattened diurnal variation compared with White gay/bisexual men.
Acknowledgments
The corresponding author thanks Sonia Lupien for her mentorship.
Funding
Funding for this article is supported by la Foundation of l'Institut universitaire en santé mentale de Montréal (Montreal Mental Health University Institute) as well as by les Fonds de la recherche en santé du Québec (Quebec Health Research Fund).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
The human studies that are part of the corresponding authors’ research program all involve ethically sound research and informed consent following international standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Sex and Gender Issues in Behavioral Health
Rights and permissions
About this article
Cite this article
Juster, RP., de Torre, M.B., Kerr, P. et al. Sex Differences and Gender Diversity in Stress Responses and Allostatic Load Among Workers and LGBT People. Curr Psychiatry Rep 21, 110 (2019). https://doi.org/10.1007/s11920-019-1104-2
Published:
DOI: https://doi.org/10.1007/s11920-019-1104-2