Abstract
Purpose of Review
We review recent findings concerning the implications of borderline personality disorder (BPD) on parenting behaviors, the parent-child relationships, and parental and child outcomes. We focus on self-report and interview data characterizing parents with BPD and their children as well as on observational paradigms investigating parent-child relationships and the quality of dyadic interactions. Novel treatment approaches are discussed.
Recent Findings
Parents with BPD suffer from increased parenting stress and display characteristic behavioral patterns towards their children, impeding the formation of a healthy parent-child relationship and disrupting offspring emotional development. Offspring are at greater risk of maltreatment and developing BPD themselves, with parental affective instability playing a substantial mediating role.
Summary
Mothers with BPD face a meaningful burden in their parenting role. Mechanisms of the transmission of BPD pathology onto the following generation are beginning to be understood. Targeted interventions have been devised recently, with preliminary testing producing encouraging results.
Similar content being viewed by others
Notes
Tronick’s still face paradigm is a standardized, video-taped procedure in which following a 2-min period of normal interaction with her child, the mother is required to keep a still-face for another 2 min facing her child, again followed by 2 min of normal interaction.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Gunderson JG, Herpertz SC, Skodol AE, Torgersen S, Zanarini MC. Borderline personality disorder. Nat Rev Dis Primers. 2018;4:18029. https://doi.org/10.1038/nrdp.2018.29.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC. 2013.
Skodol AE, Bender DS. Why are women diagnosed borderline more than men? Psychiatr Q. 2003;74(4):349–60.
Zanarini MC, Frankenburg FR, Hennen J, Silk KR. The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. Am J Psychiatry. 2003;160(2):274–83. https://doi.org/10.1176/appi.ajp.160.2.274.
Laporte L, Paris J, Zelkowitz P. Estimating the prevalence of borderline personality disorder in mothers involved in youth protection services. Personal Ment Health. 2018;12(1):49–58. https://doi.org/10.1002/pmh.1398.
Eizirik M, Fonagy P. Mentalization-based treatment for patients with borderline personality disorder: an overview. Rev Bras Psiquiatr. 2009;31(1):72–5.
Stepp SD, Whalen DJ, Pilkonis PA, Hipwell AE, Levine MD. Children of mothers with borderline personality disorder: identifying parenting behaviors as potential targets for intervention. Personal Disord. 2012;3(1):76–91. https://doi.org/10.1037/a0023081.
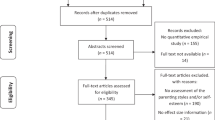
• Petfield L, Startup H, Droscher H, Cartwright-Hatton S. Parenting in mothers with borderline personality disorder and impact on child outcomes. Evid Based Ment Health. 2015;18(3):67–75. https://doi.org/10.1136/eb-2015-102163 In this recent systematic review with very restrictive quality criteria, characteristics and effects of parenting in parents with BPD are summarized.
•• Eyden J, Winsper C, Wolke D, Broome MR, MacCallum F. A systematic review of the parenting and outcomes experienced by offspring of mothers with borderline personality pathology: potential mechanisms and clinical implications. Clin Psychol Rev. 2016;47:85–105. https://doi.org/10.1016/j.cpr.2016.04.002 This is a very recent and extensive systematic review of the existing literature on parenting in parents with BPD.
Ramsauer B, Muhlhan C, Mueller J, Schulte-Markwort M. Parenting stress and postpartum depression/anxiety in mothers with personality disorders: indications for differential intervention priorities. Eur Child Adolesc Psychiatry. 2016;25(6):589–600. https://doi.org/10.1007/s00787-015-0775-4.
•• Elliot RL, Campbell L, Hunter M, Cooper G, Melville J, McCabe K, et al. When I look into my baby’s eyes…infant emotion recognition by mothers with borderline personality disorder. Infant Ment Health J. 2014;35(1):21–32. https://doi.org/10.1002/imhj.21426 In this facial emotion recognition paradigm study, the authors could demonstrate that the negativity bias in the facial recognition of neutral faces in BPD patients known from the literature extends to mothers with BPD and their offspring’s neutral facial expressions.
Macfie J, Swan SA, Fitzpatrick KL, Watkins CD, Rivas EM. Mothers with borderline personality and their young children: adult attachment interviews, mother-child interactions, and children's narrative representations. Dev Psychopathol. 2014;26(2):539–51. https://doi.org/10.1017/S095457941400011X.
Mena CG, Macfie J, Strimpfel JM. Negative affectivity and effortful control in mothers with borderline personality disorder and in their young children. J Personal Disord. 2017;31(3):417–32. https://doi.org/10.1521/pedi_2016_30_258.
• Zalewski M, Stepp SD, Whalen DJ, Scott LN. A qualitative assessment of the parenting challenges and treatment needs of mothers with borderline personality disorder. J Psychother Integr. 2015;25(2):71–89. https://doi.org/10.1037/a0038877 In this qualitative study, suggestions and wishes for therapy in parents with BPD were gathered by systematically questioning the patients themselves.
• Renneberg B, Rosenbach C. “There is not much help for mothers like me”: parenting skills for mothers with borderline personality disorder - a newly developed group training program. Borderline Personal Disord Emot Dysregul. 2016;3:16. https://doi.org/10.1186/s40479-016-0050-4 This is the first psychotherapy program specifically developed for parents with BPD. In this study its feasibility and acceptance by patients as well as its subjective effectivity was tested.
Huntley F, Wright N, Pickles A, Sharp H, Hill J. Maternal mental health and child problem behaviours: disentangling the role of depression and borderline personality dysfunction. BJPsych Open. 2017;3(6):300–5. https://doi.org/10.1192/bjpo.bp.117.005843.
Kaufman EA, Puzia ME, Mead HK, Crowell SE, McEachern A, Beauchaine TP. Children’s emotion regulation difficulties mediate the association between maternal borderline and antisocial symptoms and youth behavior problems over 1 year. J Personal Disord. 2017;31(2):170–92. https://doi.org/10.1521/pedi_2016_30_244.
•• Zalewski M, Stepp SD, Scott LN, Whalen DJ, Beeney JF, Hipwell AE. Maternal borderline personality disorder symptoms and parenting of adolescent daughters. J Personal Disord. 2014;28(4):541–54. https://doi.org/10.1521/pedi_2014_28_131 In this population-based study with a very large sample size, the authors managed to demonstrate the impact of BPD traits on parenting even in the absence of a BPD diagnosis, highlighting the influence of BPD traits in the general population.
• Kiel EJ, Viana AG, Tull MT, Gratz KL. Emotion socialization strategies of mothers with borderline personality disorder symptoms: the role of maternal emotion regulation and interactions with infant temperament. J Personal Disord. 2017;31(3):399–416. https://doi.org/10.1521/pedi_2016_30_256 In this observational paradigm study, the authors demonstrated that the negativity bias in interpersonal relationships characteristic of BPD patients extends to mothers with BPD and their children.
Hiraoka R, Crouch JL, Reo G, Wagner MF, Milner JS, Skowronski JJ. Borderline personality features and emotion regulation deficits are associated with child physical abuse potential. Child Abuse Negl. 2016;52:177–84. https://doi.org/10.1016/j.chiabu.2015.10.023.
Dittrich K, Boedeker K, Kluczniok D, Jaite C, Hindi Attar C, Fuehrer D, et al. Child abuse potential in mothers with early life maltreatment, borderline personality disorder and depression. Br J Psychiatry. 2018;213(1):412–8. https://doi.org/10.1192/bjp.2018.74.
• Kurdziel G, Kors S, Macfie J. Effect of maternal borderline personality disorder on adolescents’ experience of maltreatment and adolescent borderline features. Personal Disord, 2017. https://doi.org/10.1037/per0000265 In this interesting study, the authors assessed the association between different forms and severity of child abuse, maternal BPD pathology and adolescents’ BPD features.
• Reichl C, Brunner R, Fuchs A, Holz B, Parzer P, Fischer-Waldschmidt G, et al. Mind the fathers: associations of parental childhood adversities with borderline personality disorder pathology in female adolescents. J Pers Disord. 2017;31(6):827–43. https://doi.org/10.1521/pedi_2017_31_289 In this study, the transgenerational effect of childhood adversity and parental BPD traits on the development of BPD was analyzed. This is one of the few studies on this subject including a relevant amount of fathers in the analysis.
Macfie J, Kurdziel G, Mahan RM, Kors S. A Mother's borderline personality disorder and her sensitivity, autonomy support, hostility, fearful/disoriented behavior, and role reversal with her young child. J Personal Disord. 2017;31(6):721–37. https://doi.org/10.1521/pedi_2017_31_275.
• Frankel-Waldheter M, Macfie J, Strimpfel JM, Watkins CD. Effect of maternal autonomy and relatedness and borderline personality disorder on adolescent symptomatology. Personal Disord. 2015;6(2):152–60. https://doi.org/10.1037/per0000109 In this observational paradigm study the authors could show that mothers with BPD impede the development of autonomy and relatedness in their offspring, this being linked to increased BPD pathology in adolescents’ and possibly presenting BPD characteristic interpersonal and emotional deficits that are inter-generationally transmitted.
Kluczniok D, Boedeker K, Hindi Attar C, Jaite C, Bierbaum AL, Fuehrer D, et al. Emotional availability in mothers with borderline personality disorder and mothers with remitted major depression is differently associated with psychopathology among school-aged children. J Affect Disord. 2018;231:63–73. https://doi.org/10.1016/j.jad.2018.02.001.
Easterbrooks MA, Biringen Z. The emotional availability scales: methodological refinements of the construct and clinical implications related to gender and at-risk interactions. Infant Ment Health J. 2005;26(4):291–4. https://doi.org/10.1002/imhj.20053.
Trupe RD, Macfie J, Skadberg RM, Kurdziel G. Patterns of emotional availability between mothers and young children: associations with risk factors for borderline personality disorder. Infant Child Dev. 2018;27(1). https://doi.org/10.1002/icd.2046.
•• Marcoux AA, Bernier A, Seguin JR, Boike Armerding J, Lyons-Ruth K. How do mothers with borderline personality disorder mentalize when interacting with their infants? Personal Ment Health. 2017;11(1):14–22. https://doi.org/10.1002/pmh.1362 In this interesting study, the authors could show that mothers with BPD have greater difficulties analyzing and interpreting their children’s emotions and intentions in comparison to healthy control mothers.
•• Apter G, Devouche E, Garez V, Valente M, Genet MC, Gratier M, et al. The still-face: a greater challenge for infants of mothers with borderline personality disorder. J Pers Disord. 2017;31(2):156–69. https://doi.org/10.1521/pedi_2016_30_243 Using a well-validated observational paradigm, the authors could identify characteristics of the dyadic relationship between mothers with BPD and their offspring. Maternal as well as offspring behavior was analyzed.
Weinberg MK, Tronick EZ. Beyond the face: an empirical study of infant affective configurations of facial, vocal, gestural, and regulatory behaviors. Child Dev. 1994;65(5):1503–15.
Whalen DJ, Kiel EJ, Tull MT, Latzman RD, Gratz KL. Maternal borderline personality disorder symptoms and convergence between observed and reported infant negative emotional expressions. Personal Disord. 2015;6(3):229–38. https://doi.org/10.1037/per0000116.
Gratz KL, Kiel EJ, Latzman RD, Elkin TD, Moore SA, Tull MT. Emotion: empirical contribution. Maternal borderline personality pathology and infant emotion regulation: examining the influence of maternal emotion-related difficulties and infant attachment. J Personal Disord. 2014;28(1):52–69. https://doi.org/10.1521/pedi.2014.28.1.52.
• Mahan RM, Kors SB, Simmons ML, Macfie J. Maternal psychological control, maternal borderline personality disorder, and adolescent borderline features. Personal Disord. 2018;9(4):297–304. https://doi.org/10.1037/per0000269 This observational paradigm study could demonstrate a mediating effect of maternal affective instability on offspring affective instability, hinting at the intergenerational transmission of this BPD characteristic trait.
Yelland C, Girke T, Tottman C, Williams AS. Clinical characteristics and mental health outcomes for women admitted to an Australian mother-baby unit: a focus on borderline personality disorder and emotional dysregulation? Australas Psychiatry. 2015;23(6):683–7. https://doi.org/10.1177/1039856215590251.
McCarthy KL, Lewis KL, Bourke ME, Grenyer BF. A new intervention for people with borderline personality disorder who are also parents: a pilot study of clinician acceptability. Borderline Personal Disord Emot Dysregul. 2016;3(1):10. https://doi.org/10.1186/s40479-016-0044-2.
•• Sved Williams A, Yelland C, Hollamby S, Wigley M, Aylward P. A new therapeutic group to help women with borderline personality disorder and their infants. J Psychiatr Pract. 2018;24(5):331–340. https://doi.org/10.1097/PRA.0000000000000330. In this study, a comprehensive therapeutic program specifically aimed at mothers with BPD and their children was developed and maternal outcomes extensively assessed on various self-report scales.
Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev. 2011;14(1):1–27. https://doi.org/10.1007/s10567-010-0080-1.
Hoffman C, Dunn DM, Njoroge WFM. Impact of postpartum mental illness upon infant development. Curr Psychiatry Rep. 2017;19(12):100. https://doi.org/10.1007/s11920-017-0857-8.
Bodeker K, Fuchs A, Fuhrer D, Kluczniok D, Dittrich K, Reichl C, et al. Impact of maternal early life maltreatment and maternal history of depression on child psychopathology: mediating role of maternal sensitivity? Child Psychiatry Hum Dev. 2018. https://doi.org/10.1007/s10578-018-0839-z.
Funding
The study was supported by the grant UBICA-II from the German Federal Ministry of Education and Research to SC.H. (BMBF 01KR1803B). The German Federal Ministry of Education and Research had no influence on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Julian G. Florange and Sabine C. Herpertz declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Personality Disorders
Rights and permissions
About this article
Cite this article
Florange, J.G., Herpertz, S.C. Parenting in Patients with Borderline Personality Disorder, Sequelae for the Offspring and Approaches to Treatment and Prevention. Curr Psychiatry Rep 21, 9 (2019). https://doi.org/10.1007/s11920-019-0996-1
Published:
DOI: https://doi.org/10.1007/s11920-019-0996-1