Abstract
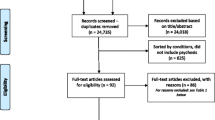
The immediate postpartum period is a time of acute vulnerability to mental illness, which presents unique challenges for the psychiatric consultant. Because the postpartum hospital stay is typically brief, the consultant must have a working knowledge of postpartum physiology and the myriad forms of mental illness that may emerge in this vulnerable time, in order to quickly make a diagnosis and formulate a treatment plan. This review aims to characterize the most common reasons for postpartum consultation, review postpartum physiology and psychiatric conditions, and propose an evidence-based, practical approach to treatment. A literature search using the terms “postpartum,” “obstetric,” “consultation,” and “psychiatry” yielded six studies that identified reasons for psychiatric consultation to the obstetrics and gynecology services. These studies informed the structure of the article such that we review the most common reasons for consultation and how to approach each issue. The most common reason for consultation is past psychiatric history, often in the absence of current symptoms. For each clinical situation, including depression, adverse birth events, and psychosis, we present a differential diagnosis, as well as risk factors, clinical signs, and recommended treatment.
Similar content being viewed by others
References
Hutner L, Sacks A, Segal C. Characteristics of the population of patients on an obstetrics-gynecology consultation-liaison service. Paris, France: Marce Society; 2012.
Dunsis A, Smith GC. Consultation-liaison psychiatry in an obstetric service. Aust N Z J Psychiatry. 1996;30(1):63–73.
Judd F, Stafford L, Handrinos D, Laios L, Breadon C, Cornthwaite L, et al. Consultation-liaison psychiatry in a maternity hospital. Australas Psychiatry. 2010;18(2):120–4.
Sloan EP, Kirsh S. Characteristics of obstetrical inpatients referred to a consultation-liaison psychiatry service in a tertiary-level university hospital. Arch Womens Ment Health. 2008;11(5–6):327–33.
Tsai SJ, Lee YC, Yang CH, Sim CB. Psychiatric consultations in obstetric inpatients. J Obstet Gynaecol Res. 1996;22(6):603–7.
Rigatelli M, Galeazzi GM, Palmieri G. Consultation-liaison psychiatry in obstetrics and gynecology. J Psychosom Obstet Gynaecol. 2002;23(3):165–72.
Lin HL, Chou HH, Liu CY, Hsu SC, Hsiao MC, Juang YY. The role of consulting psychiatrists for obstetric and gynecologic inpatients. Chang Gung Med J. 2011;34(1):57–64.
Mourikis I, Kouzoupis AV, Antoniou M, Spyropoulou A, Leonardou A, Vogiatzi M, et al. Consultation-liaison psychiatry service in obstetrics and gynecology, in Athens, Greece. Eur Neuropsychopharmacol. 2009;19:S697.
Benjet C, Azar ST, Kuersten-Hogan R. Evaluating the parental fitness of psychiatrically diagnosed individuals: advocating a functional-contextual analysis of parenting. J Fam Psychol. 2003;17(2):238–51.
Rutherford SJ, Keeley P. Assessing parenting capacity: are mental health nurses prepared for this role? J Psychiatr Ment Health Nurs. 2009;16(4):363–7.
Nair S, Morrison MF. The evaluation of maternal competency. Psychosomatics. 2000;41(6):523–30.
Oyserman D, Mowbray CT, Meares PA, Firminger KB. Parenting among mothers with a serious mental illness. Am J Orthopsychiatry. 2000;70(3):296–315.
Brockington I. Motherhood and mental health. Oxford, England: Oxford University Press; 1996.
Beck CT, Reynolds MA, Rutowski P. Maternity blues and postpartum depression. J Obstet Gynecol Neonatal Nurs. 1992;21(4):287–93.
O'Hara MW. Postpartum depression: what we know. J Clin Psychol. 2009;65(12):1258–69.
O'Hara MW, Zekoski EM, Philipps LH, Wright EJ. Controlled prospective study of postpartum mood disorders: comparison of childbearing and nonchildbearing women. J Abnorm Psychol. 1990;99(1):3–15.
Murray L, Cooper P. Effects of postnatal depression on infant development. Arch Dis Child. 1997;77(2):99–101.
Whiffen VE, Gotlib IH. Infants of postpartum depressed mothers: temperament and cognitive status. J Abnorm Psychol. 1989;98(3):274–9.
Wrate RM, Rooney AC, Thomas PF, Cox JL. Postnatal depression and child development. A three-year follow-up study. Br J Psychiatry. 1985;146:622–7.
Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012–24.
Kim DR, Sockol LE, Sammel MD, Kelly C, Moseley M, Epperson CN. Elevated risk of adverse obstetric outcomes in pregnant women with depression. Arch Womens Ment Health. 2013;16(6):475–82.
Kim JH, Choi SS, Ha K. A closer look at depression in mothers who kill their children: is it unipolar or bipolar depression? J Clin Psychiatry. 2008;69(10):1625–31.
American Psychiatric Association. Depressive disorders. In: Diagnostic and Statistical Manual of Mental Disorders. 5th ed.; 2013. pp. 186–7
American Psychiatric Association. Depressive disorders. In: Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition, Text Revision ed.; 2000. pp. 422–3.
Bloch M, Schmidt PJ, Danaceau M, Murphy J, Nieman L, Rubinow DR. Effects of gonadal steroids in women with a history of postpartum depression. Am J Psychiatry. 2000;157(6):924–30.
Forty L, Jones L, Macgregor S, Caesar S, Cooper C, Hough A, et al. Familiality of postpartum depression in unipolar disorder: results of a family study. Am J Psychiatry. 2006;163(9):1549–53.
Murphy-Eberenz K, Zandi PP, March D, Crowe RR, Scheftner WA, Alexander M, et al. Is perinatal depression familial? J Affect Disord. 2006;90(1):49–55.
El-Ibiary SY, Hamilton SP, Abel R, Erdman CA, Robertson PA, Finley PR. A pilot study evaluating genetic and environmental factors for postpartum depression. Innov Clin Neurosci. 2013;10(9–10):15–22.
Costas J, Gratacos M, Escaramis G, Martin-Santos R, de Diego Y, Baca-Garcia E, et al. Association study of 44 candidate genes with depressive and anxiety symptoms in post-partum women. J Psychiatr Res. 2010;44(11):717–24.
Doornbos B, Dijck-Brouwer DA, Kema IP, Tanke MA, van Goor SA, Muskiet FA, et al. The development of peripartum depressive symptoms is associated with gene polymorphisms of MAOA, 5-HTT and COMT. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33(7):1250–4.
Guintivano J, Arad M, Gould TD, Payne JL, Kaminsky ZA. Antenatal prediction of postpartum depression with blood DNA methylation biomarkers. Mol Psychiatry. 2014;19(5):560–7.
Schiller CE, Meltzer-Brody S, Rubinow DR. The role of reproductive hormones in postpartum depression. CNS Spectr. 2014;29:1–12.
Payne JL, Palmer JT, Joffe H. A reproductive subtype of depression: conceptualizing models and moving toward etiology. Harv Rev Psychiatry. 2009;17(2):72–86.
Brett M, Baxendale S. Motherhood and memory: a review. Psychoneuroendocrinology. 2001;26(4):339–62.
Hendrick V, Altshuler LL, Suri R. Hormonal changes in the postpartum and implications for postpartum depression. Psychosomatics. 1998;39(2):93–101.
Osterlund MK. Underlying mechanisms mediating the antidepressant effects of estrogens. Biochim Biophys Acta. 2010;1800(10):1136–44.
Rubinow DR, Schmidt PJ, Roca CA. Estrogen-serotonin interactions: implications for affective regulation. Biol Psychiatry. 1998;44(9):839–50.
Chevillard C, Barden N, Saavedra JM. Estradiol treatment decreases type A and increases type B monoamine oxidase in specific brain stem areas and cerebellum of ovariectomized rats. Brain Res. 1981;222(1):177–81.
Ma ZQ, Bondiolotti GP, Olasmaa M, Violani E, Patrone C, Picotti GB, et al. Estrogen modulation of catecholamine synthesis and monoamine oxidase A activity in the human neuroblastoma cell line SK-ER3. J Steroid Biochem Mol Biol. 1993;47(1–6):207–11.
Ma ZQ, Violani E, Villa F, Picotti GB, Maggi A. Estrogenic control of monoamine oxidase A activity in human neuroblastoma cells expressing physiological concentrations of estrogen receptor. Eur J Pharmacol. 1995;284(1–2):171–6.
Sacher J, Wilson AA, Houle S, Rusjan P, Hassan S, Bloomfield PM, et al. Elevated brain monoamine oxidase A binding in the early postpartum period. Arch Gen Psychiatry. 2010;67(5):468–74.
Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry. 2013;70(5):490–8.
Harris B, Johns S, Fung H, Thomas R, Walker R, Read G, et al. The hormonal environment of post-natal depression. Br J Psychiatry. 1989;154:660–7.
Harris B. Biological and hormonal aspects of postpartum depressed mood. Br J Psychiatry. 1994;164(3):288–92.
Yim IS, Glynn LM, Dunkel-Schetter C, Hobel CJ, Chicz-DeMet A, Sandman CA. Risk of postpartum depressive symptoms with elevated corticotropin-releasing hormone in human pregnancy. Arch Gen Psychiatry. 2009;66(2):162–9.
Rich-Edwards JW, Mohllajee AP, Kleinman K, Hacker MR, Majzoub J, Wright RJ, et al. Elevated midpregnancy corticotropin-releasing hormone is associated with prenatal, but not postpartum, maternal depression. J Clin Endocrinol Metab. 2008;93(5):1946–51.
Meltzer-Brody S, Stuebe A, Dole N, Savitz D, Rubinow D, Thorp J. Elevated corticotropin releasing hormone (CRH) during pregnancy and risk of postpartum depression (PPD). J Clin Endocrinol Metab. 2011;96(1):E40–7.
Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26(4):289–95.
Glynn LM, Davis EP, Sandman CA. New insights into the role of perinatal HPA-axis dysregulation in postpartum depression. Neuropeptides. 2013;47(6):363–70.
Bloch M, Rotenberg N, Koren D, Klein E. Risk factors associated with the development of postpartum mood disorders. J Affect Disord. 2005;88(1):9–18.
Bloch M, Rotenberg N, Koren D, Klein E. Risk factors for early postpartum depressive symptoms. Gen Hosp Psychiatry. 2006;28(1):3–8.
Jardri R, Pelta J, Maron M, Thomas P, Delion P, Codaccioni X, et al. Predictive validation study of the edinburgh postnatal depression scale in the first week after delivery and risk analysis for postnatal depression. J Affect Disord. 2006;93(1–3):169–76.
Buttner MM, Mott SL, Pearlstein T, Stuart S, Zlotnick C, O'Hara MW. Examination of premenstrual symptoms as a risk factor for depression in postpartum women. Arch Womens Ment Health. 2013;16(3):219–25.
Di Florio A, Jones L, Forty L, Gordon-Smith K, Blackmore ER, Heron J, et al. Mood disorders and parity—a clue to the aetiology of the postpartum trigger. J Affect Disord. 2014;152–154:334–9.
Ludermir AB, Lewis G, Valongueiro SA, de Araujo TV, Araya R. Violence against women by their intimate partner during pregnancy and postnatal depression: a prospective cohort study. Lancet. 2010;376(9744):903–10.
Nelson DB, Freeman MP, Johnson NL, McIntire DD, Leveno KJ. A prospective study of postpartum depression in 17 648 parturients. J Matern Fetal Neonatal Med. 2013;26(12):1155–61.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150:782–6.
Evins GG, Theofrastous JP, Galvin SL. Postpartum depression: a comparison of screening and routine clinical evaluation. Am J Obstet Gynecol. 2000;182(5):1080–2.
Petrozzi A, Gagliardi L. Anxious and depressive components of Edinburgh postnatal depression scale in maternal postpartum psychological problems. J Perinat Med. 2013;41(4):343–8.
Wisner KL, Perel JM, Peindl KS, Hanusa BH, Piontek CM, Findling RL. Prevention of postpartum depression: a pilot randomized clinical trial. Am J Psychiatry. 2004;161(7):1290–2.
Dennis CL, Dowswell T. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst Rev. 2013;CD001134.
Howell EA, Balbierz A, Wang J, Parides M, Zlotnick C, Leventhal H. Reducing postpartum depressive symptoms among black and Latina mothers: a randomized controlled trial. Obstet Gynecol. 2012;119(5):942–9.
Kim DR, Epperson CN, Weiss AR, Wisner KL. Pharmacotherapy of postpartum depression: an update. Expert Opin Pharmacother. 2014;15(9):1223–34.
Moses-Kolko EL, Berga SL, Kalro B, Sit DK, Wisner KL. Transdermal estradiol for postpartum depression: a promising treatment option. Clin Obstet Gynecol. 2009;52(3):516–29.
Davanzo R, Copertino M, De Cunto A, Minen F, Amaddeo A. Antidepressant drugs and breastfeeding: a review of the literature. Breastfeed Med. 2011;6(2):89–98.
Lanza di Scalea T, Wisner KL. Antidepressant medication use during breastfeeding. Clin Obstet Gynecol. 2009;52(3):483–97.
Forrest GC, Standish E, Baum JD. Support after perinatal death: a study of support and counselling after perinatal bereavement. Br Med J (Clin Res Ed). 1982;285(6353):1475–9.
Hughes P, Turton P, Hopper E, McGauley GA, Fonagy P. Disorganised attachment behaviour among infants born subsequent to stillbirth. J Child Psychol Psychiatry. 2001;42(6):791–801.
Gold KJ, Boggs ME, Muzik M, Sen A. Anxiety disorders and obsessive compulsive disorder 9 months after perinatal loss. Gen Hosp Psychiatry. 2014.
Gold KJ, Johnson TR. Mothers at risk: maternal mental health outcomes after perinatal death. Obstet Gynecol. 2014;123(1):6S.
Engelhard IM, van den Hout MA, Arntz A. Posttraumatic stress disorder after pregnancy loss. Gen Hosp Psychiatry. 2001;23(2):62–6.
Christiansen DM, Elklit A, Olff M. Parents bereaved by infant death: PTSD symptoms up to 18 years after the loss. Gen Hosp Psychiatry. 2013;35(6):605–11.
Cacciatore J, Radestad I, Frederik Froen J. Effects of contact with stillborn babies on maternal anxiety and depression. Birth. 2008;35(4):313–20.
Erlandsson K, Warland J, Cacciatore J, Radestad I. Seeing and holding a stillborn baby: mothers’ feelings in relation to how their babies were presented to them after birth—findings from an online questionnaire. Midwifery. 2013;29(3):246–50.
Hughes P, Turton P, Hopper E, Evans CD. Assessment of guidelines for good practice in psychosocial care of mothers after stillbirth: a cohort study. Lancet. 2002;360(9327):114–8.
Gold KJ, Dalton VK, Schwenk TL. Hospital care for parents after perinatal death. Obstet Gynecol. 2007;109(5):1156–66.
Hughes P, Riches S. Psychological aspects of perinatal loss. Curr Opin Obstet Gynecol. 2003;15(2):107–11.
Cunningham KA. Holding a stillborn baby: does the existing evidence help us provide guidance? Med J Aust. 2012;196(9):558–60.
Koopmans L, Wilson T, Cacciatore J, Flenady V. Support for mothers, fathers and families after perinatal death. Cochrane Database Syst Rev. 2013;6:CD000452.
Kersting A, Dolemeyer R, Steinig J, Walter F, Kroker K, Baust K, et al. Brief internet-based intervention reduces posttraumatic stress and prolonged grief in parents after the loss of a child during pregnancy: a randomized controlled trial. Psychother Psychosom. 2013;82(6):372–81.
Gold KJ, Kuznia AL, Hayward RA. How physicians cope with stillbirth or neonatal death: a national survey of obstetricians. Obstet Gynecol. 2008;112(1):29–34.
Farrow VA, Goldenberg RL, Fretts R, Schulkin J. Psychological impact of stillbirths on obstetricians. J Matern Fetal Neonatal Med. 2013;26(8):748–52.
Swanson LM, Flynn H, Adams-Mundy JD, Armitage R, Arnedt JT. An open pilot of cognitive-behavioral therapy for insomnia in women with postpartum depression. Behav Sleep Med. 2013;11(4):297–307.
Hudak R, Wisner KL. Diagnosis and treatment of postpartum obsessions and compulsions that involve infant harm. Am J Psychiatry. 2012;169(4):360–3.
Abramowitz JS, Meltzer-Brody S, Leserman J, Killenberg S, Rinaldi K, Mahaffey BL, et al. Obsessional thoughts and compulsive behaviors in a sample of women with postpartum mood symptoms. Arch Womens Ment Health. 2010;13(6):523–30.
Miller ES, Chu C, Gollan J, Gossett DR. Obsessive-compulsive symptoms during the postpartum period. A prospective cohort. J Reprod Med. 2013;58(3-4):115–22.
Grekin R, O'Hara MW. Prevalence and risk factors of postpartum posttraumatic stress disorder: a meta-analysis. Clin Psychol Rev. 2014;34(5):389–401.
Beck CT, Gable RK, Sakala C, Declercq ER. Posttraumatic stress disorder in new mothers: results from a two-stage U.S. national survey. Birth. 2011;38(3):216–27.
Gotkine M, Ben-Hur T, Vincent A, Vaknin-Dembinsky A. Limbic encephalitis presenting as a post-partum psychiatric condition. J Neurol Sci. 2011;308(1–2):152–4.
Munk-Olsen T, Laursen TM, Mendelson T, Pedersen CB, Mors O, Mortensen PB. Risks and predictors of readmission for a mental disorder during the postpartum period. Arch Gen Psychiatry. 2009;66(2):189–95.
Valdimarsdottir U, Hultman CM, Harlow B, Cnattingius S, Sparen P. Psychotic illness in first-time mothers with no previous psychiatric hospitalizations: a population-based study. PLoS Med. 2009;6(2):e13.
Jones I, Craddock N. Familiality of the puerperal trigger in bipolar disorder: results of a family study. Am J Psychiatry. 2001;158(6):913–7.
Sit D, Rothschild AJ, Wisner KL. A review of postpartum psychosis. J Womens Health (Larchmt). 2006;15(4):352–68.
Blackmore ER, Jones I, Doshi M, Haque S, Holder R, Brockington I, et al. Obstetric variables associated with bipolar affective puerperal psychosis. Br J Psychiatry. 2006;188:32–6.
Bergink V, Lambregtse-van den Berg MP, Koorengevel KM, Kupka R, Kushner SA. First-onset psychosis occurring in the postpartum period: a prospective cohort study. J Clin Psychiatry. 2011;72(11):1531–7.
Bergink V, Bouvy PF, Vervoort JS, Koorengevel KM, Steegers EA, Kushner SA. Prevention of postpartum psychosis and mania in women at high risk. Am J Psychiatry. 2012;169(6):609–15.
Kendell RE, Chalmers JC, Platz C. Epidemiology of puerperal psychoses. Br J Psychiatry. 1987;150:662–73.
Altshuler LL, Hendrick V, Cohen LS. Course of mood and anxiety disorders during pregnancy and the postpartum period. J Clin Psychiatry. 1998;59 Suppl 2:29–33.
Blackmore ER, Rubinow DR, O’Connor TG, Liu X, Tang W, Craddock N, et al. Reproductive outcomes and risk of subsequent illness in women diagnosed with postpartum psychosis. Bipolar Disord. 2013;15(4):394–404.
Bergink V, Burgerhout KM, Weigelt K, Pop VJ, de Wit H, Drexhage RC, et al. Immune system dysregulation in first-onset postpartum psychosis. Biol Psychiatry. 2013;73(10):1000–7.
Weigelt K, Bergink V, Burgerhout KM, Pescatori M, Wijkhuijs A, Drexhage HA. Down-regulation of inflammation-protective microRNAs 146a and 212 in monocytes of patients with postpartum psychosis. Brain Behav Immun. 2013;29:147–55.
Bergink V, Gibney SM, Drexhage HA. Autoimmunity, inflammation, and psychosis: a search for peripheral markers. Biol Psychiatry. 2014;75(4):324–31.
Viguera AC, Emmerich AD, Cohen LS. Case records of the Massachusetts General Hospital. Case 24-2008. A 35-year-old woman with postpartum confusion, agitation, and delusions. N Engl J Med. 2008;359(5):509–15.
Wisner KL, Peindl K, Hanusa BH. Symptomatology of affective and psychotic illnesses related to childbearing. J Affect Disord. 1994;30(2):77–87.
Rhode A, Marneros A. Postpartum psychoses: onset and long-term course. jPsychopharmacology. 1993;26(3–4):203–9.
Oates M. Suicide: the leading cause of maternal death. Br J Psychiatry. 2003;183:279–81.
Porter T, Gavin H. Infanticide and neonaticide: a review of 40 years of research literature on incidence and causes. Trauma Violence Abuse. 2010;11(3):99–112.
Rahman T, Grellner KA, Harry B, Beck N, Lauriello J. Infanticide in a case of folie a deux. Am J Psychiatry. 2013;170(10):1110–2.
Nonacs R, Cohen LS. Postpartum mood disorders: diagnosis and treatment guidelines. J Clin Psychiatry. 1998;59 Suppl 2:34–40.
Chandra PS, Bhargavaraman RP, Raghunandan VN, Shaligram D. Delusions related to infant and their association with mother–infant interactions in postpartum psychotic disorders. Arch Womens Ment Health. 2006;9(5):285–8.
Stewart DE, Klompenhouwer JL, Kendell RE, van Hulst AM. Prophylactic lithium in puerperal psychosis. The experience of three centres. Br J Psychiatry. 1991;158:393–7.
Austin MP. Puerperal affective psychosis: is there a case for lithium prophylaxis? Br J Psychiatry. 1992;161:692–4.
Wisner KL, Hanusa BH, Peindl KS, Perel JM. Prevention of postpartum episodes in women with bipolar disorder. Biol Psychiatry. 2004;56(8):592–6.
Sharma V, Smith A, Mazmanian D. Olanzapine in the prevention of postpartum psychosis and mood episodes in bipolar disorder. Bipolar Disord. 2006;8(4):400–4.
Essali A, Alabed S, Guul A, Essali N. Preventive interventions for postnatal psychosis. Cochrane Database Syst Rev. 2013;6:CD009991.
Sharma V. Pharmacotherapy of postpartum psychosis. Expert Opin Pharmacother. 2003;4(10):1651–8.
Engqvist I, Nilsson K. Involving the family in the care and treatment of women with postpartum psychosis: Swedish psychiatrists’ experiences. Psychiatry J. 2013;2013:897084.
Marsh W, Viguera A. Bipolar disorder through pregnancy and postpartum. Psychiatr Ann. 2012;42(5):184–9.
Viguera AC, Newport DJ, Ritchie J, Stowe Z, Whitfield T, Mogielnicki J, et al. Lithium in breast milk and nursing infants: clinical implications. Am J Psychiatry. 2007;164(2):342–5.
Yonkers KA, Wisner KL, Stowe Z, Leibenluft E, Cohen L, Miller L, et al. Management of bipolar disorder during pregnancy and the postpartum period. Am J Psychiatry. 2004;161(4):608–20.
Gardiner SJ, Kristensen JH, Begg EJ, Hackett LP, Wilson DA, Ilett KF, et al. Transfer of olanzapine into breast milk, calculation of infant drug dose, and effect on breast-fed infants. Am J Psychiatry. 2003;160(8):1428–31.
Brockington IF. Cerebral vascular disease as a cause of postpartum psychosis. Arch Womens Ment Health. 2007;10(4):177–8.
Brockington IF. Eclamptic psychosis. Arch Womens Ment Health. 2007;10(2):87–8.
Bergink V, Kushner SA, Pop V, Kuijpens H, Lambregtse-van den Berg MP, Drexhage RC, et al. Prevalence of autoimmune thyroid dysfunction in postpartum psychosis. Br J Psychiatry. 2011;198(4):264–8.
Castro J, Billick S, Kleiman A, Chiechi M, Al-Rashdan M. Confounding psychosis in the postpartum period. Psychiatr Q. 2014;85(1):91–6.
Boulanger E, Pagniez D, Roueff S, Binaut R, Valat AS, Provost N, et al. Sheehan syndrome presenting as early post-partum hyponatraemia. Nephrol Dial Transplant. 1999;14(11):2714–5.
Kovacs K. Sheehan syndrome. Lancet. 2003;361(9356):520–2.
Shoib S, Dar MM, Arif T, Bashir H, Bhat MH, Ahmed J. Sheehan's syndrome presenting as psychosis: a rare clinical presentation. Med J Islam Repub Iran. 2013;27(1):35–7.
Peterson DE. Acute postpartum mental status change and coma caused by previously undiagnosed ornithine transcarbamylase deficiency. Obstet Gynecol. 2003;102(5 Pt 2):1212–5.
Enns GM, O'Brien WE, Kobayashi K, Shinzawa H, Pellegrino JE. Postpartum “psychosis” in mild argininosuccinate synthetase deficiency. Obstet Gynecol. 2005;105(5 Pt 2):1244–6.
Wong LJ, Craigen WJ, O'Brien WE. Postpartum coma and death due to carbamoyl-phosphate synthetase I deficiency. Ann Intern Med. 1994;120(3):216–7.
Cordero DR, Baker J, Dorinzi D, Toffle R. Ornithine transcarbamylase deficiency in pregnancy. J Inherit Metab Dis. 2005;28(2):237–40.
Leonis MA, Balistreri WF. Ch. 76: other inherited metabolic disorders of the liver. In: Feldman M, Friedman LS, Brandt LJ, editors. Sleisinger and Fordtran’s gastrointestinal and liver disease. 9th ed. Saunders Elsevier: Philadelphia, PA, USA; 2010. p. 1271–4.
Brockington IF. The present importance of the organic psychoses of pregnancy, parturition and the puerperium. Arch Womens Ment Health. 2007;10(6):305–6.
Brockington IF. Postpartum psychoses due to other diseases with a specific link to childbirth. Arch Womens Ment Health. 2007;10(5):241–2.
Groves JE. Management of the borderline patient on a medical or surgical ward: the psychiatric consultant's role. Int J Psychiatry Med. 1975;6(3):337–48.
Miller C, Lanham A, Welsh C, Ramanadhan S, Terplan M. Screening, testing, and reporting for drug and alcohol use on labor and delivery: a survey of Maryland birthing hospitals. Soc Work Health Care. 2014;53(7):659–69.
Gopman S. Prenatal and postpartum care of women with substance use disorders. Obstet Gynecol Clin North Am. 2014;41(2):213–28.
Klinger G, Stahl B, Fusar-Poli P, Merlob P. Antipsychotic drugs and breastfeeding. Pediatr Endocrinol Rev. 2013;10(3):308–17.
Stowe ZN. The use of mood stabilizers during breastfeeding. J Clin Psychiatry. 2007;68 Suppl 9:22–8.
Molyneaux E, Howard LM, McGeown HR, Karia AM, Trevillion K. Antidepressant treatment for postnatal depression. Cochrane Database Syst Rev. 2014;9:CD002018.
Yonkers KA, Vigod S, Ross LE. Diagnosis, pathophysiology, and management of mood disorders in pregnant and postpartum women. Obstet Gynecol. 2011;117(4):961–77.
Fortinguerra F, Clavenna A, Bonati M. Psychotropic drug use during breastfeeding: a review of the evidence. Pediatrics. 2009;124(4):e547–56.
Acknowledgments
This manuscript was supported by NIMH grant K23 MH092399 (P.I. DRK).
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Neither Dr. Anderson nor Dr. Kim have any conflicts of interest to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Women's Mental Health
Rights and permissions
About this article
Cite this article
Anderson, E.A., Kim, D.R. Psychiatric Consultation to the Postpartum Mother. Curr Psychiatry Rep 17, 26 (2015). https://doi.org/10.1007/s11920-015-0561-5
Published:
DOI: https://doi.org/10.1007/s11920-015-0561-5