Abstract
Purpose of Review
The purpose of this review is to outline the principles of clinical genetic testing and to provide practical guidance to clinicians in navigating genetic testing for patients with suspected monogenic forms of osteoporosis.
Recent Findings
Heritability assessments and genome-wide association studies have clearly shown the significant contributions of genetic variations to the pathogenesis of osteoporosis. Currently, over 50 monogenic disorders that present primarily with low bone mass and increased risk of fractures have been described. The widespread availability of clinical genetic testing offers a valuable opportunity to correctly diagnose individuals with monogenic forms of osteoporosis, thus instituting appropriate surveillance and treatment.
Summary
Clinical genetic testing may identify the appropriate diagnosis in a subset of patients with low bone mass, multiple or unusual fractures, and severe or early-onset osteoporosis, and thus clinicians should be aware of how to incorporate such testing into their clinical practices.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sarafrazi N, Wambogo EA, Shepherd JA. Osteoporosis or low bone mass in older adults: United States, 2017–2018. NCHS Data Brief. 2021;405:1–8.
Mergler S, et al. Epidemiology of low bone mineral density and fractures in children with severe cerebral palsy: a systematic review. Dev Med Child Neurol. 2009;51(10):773–8.
Presedo A, Dabney KW, Miller F. Fractures in patients with cerebral palsy. J Pediatr Orthop. 2007;27(2):147–53.
Burge R, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22(3):465–75.
Compston JE, McClung MR, Leslie WD. Osteoporosis. Lancet. 2019;393(10169):364–76.
Yengo L, et al. A saturated map of common genetic variants associated with human height. Nature. 2022;610(7933):704–12.
Timpson NJ, et al. Genetic architecture: the shape of the genetic contribution to human traits and disease. Nat Rev Genet. 2018;19(2):110–24.
Trajanoska K, Rivadeneira F. The genetic architecture of osteoporosis and fracture risk. Bone. 2019;126:2–10.
• Chen S, et al. Genetic burden contributing to extremely low or high bone mineral density in a senior male population from the Osteoporotic Fractures in Men Study (MrOS). JBMR Plus. 2020; 4(3): e10335. Interesting study that determined the burden of rare genetic variants in development of osteoporosis-related fractures.
Bjornerem A, et al. Genetic and environmental variances of bone microarchitecture and bone remodeling markers: a twin study. J Bone Miner Res. 2015;30(3):519–27.
Piroska M, et al. Strong genetic effects on bone mineral density in multiple locations with two different techniques: results from a cross-sectional twin study. Medicina (Kaunas). 2021;57(3):248.
• Richards JB, et al. Bone mineral density, osteoporosis, and osteoporotic fractures: a genome-wide association study. Lancet. 2008;371(9623):1505–12. Pivotal osteoporosis GWAS.
• Styrkarsdottir U, et al. Multiple genetic loci for bone mineral density and fractures. N Engl J Med. 2008;358(22):2355–65. Pivotal osteoporosis GWAS.
• Rivadeneira F, et al. Twenty bone-mineral-density loci identified by large-scale meta-analysis of genome-wide association studies. Nat Genet. 2009;41(11):1199–206. Meta-analysis of pivotal osteoporosis GWAS.
Paternoster L, et al. Genetic determinants of trabecular and cortical volumetric bone mineral densities and bone microstructure. PLoS Genet. 2013;9(2): e1003247.
Styrkarsdottir U, et al. New sequence variants associated with bone mineral density. Nat Genet. 2009;41(1):15–7.
Pocock NA, et al. Genetic determinants of bone mass in adults. A twin study. J Clin Invest. 1987;80(3):706–10.
Flicker L, et al. Bone density determinants in elderly women: a twin study. J Bone Miner Res. 1995;10(11):1607–13.
Gueguen R, et al. Segregation analysis and variance components analysis of bone mineral density in healthy families. J Bone Miner Res. 1995;10(12):2017–22.
Krall EA, Dawson-Hughes B. Heritable and life-style determinants of bone mineral density. J Bone Miner Res. 1993;8(1):1–9.
Karasik D, et al. Heritability and genetic correlations for bone microarchitecture: the Framingham Study Families. J Bone Miner Res. 2017;32(1):106–14.
Kemp JP, et al. Phenotypic dissection of bone mineral density reveals skeletal site specificity and facilitates the identification of novel loci in the genetic regulation of bone mass attainment. PLoS Genet. 2014;10(6): e1004423.
Patel RM, et al. A cross-sectional multicenter study of osteogenesis imperfecta in North America - results from the linked clinical research centers. Clin Genet. 2015;87(2):133–40.
Trajanoska K, et al. Assessment of the genetic and clinical determinants of fracture risk: genome wide association and mendelian randomisation study. BMJ. 2018;362: k3225.
Nethander M, et al. Assessment of the genetic and clinical determinants of hip fracture risk: genome-wide association and Mendelian randomization study. Cell Rep Med. 2022;3(10): 100776.
Alonso N, et al. Identification of a novel locus on chromosome 2q13, which predisposes to clinical vertebral fractures independently of bone density. Ann Rheum Dis. 2018;77(3):378–85.
Styrkarsdottir U, et al. GWAS of bone size yields twelve loci that also affect height, BMD, osteoarthritis or fractures. Nat Commun. 2019;10(1):2054.
•• Zhu X, Bai W, Zheng H. Twelve years of GWAS discoveries for osteoporosis and related traits: advances, challenges and applications. Bone Res. 2021;9(1):23. This is a comprehensive review of the history of osteoporosis-related GWAS.
Kim SK. Identification of 613 new loci associated with heel bone mineral density and a polygenic risk score for bone mineral density, osteoporosis and fracture. PLoS ONE. 2018;13(7): e0200785.
Kemp JP, et al. Identification of 153 new loci associated with heel bone mineral density and functional involvement of GPC6 in osteoporosis. Nat Genet. 2017;49(10):1468–75.
Morris JA, et al. An atlas of genetic influences on osteoporosis in humans and mice. Nat Genet. 2019;51(2):258–66.
Medina-Gomez C, et al. Life-course genome-wide association study meta-analysis of total body BMD and assessment of age-specific effects. Am J Hum Genet. 2018;102(1):88–102.
He D, et al. Exome-wide screening identifies novel rare risk variants for bone mineral density. Osteoporos Int. 2023;34(5):965–75.
• Lu T, et al. Individuals with common diseases but with a low polygenic risk score could be prioritized for rare variant screening. Genet Med. 2021;23(3): 508–15. This study shows that patients who have osteoporosis but a low burden of common variants by PRS may benefit from further clinical genetic evaluation.
Backman JD, et al. Exome sequencing and analysis of 454,787 UK Biobank participants. Nature. 2021;599(7886):628–34.
Yalaev B, et al. Using a polygenic score to predict the risk of developing primary osteoporosis. Int J Mol Sci. 2022;23(17):10021.
• Lu T, et al. Improved prediction of fracture risk leveraging a genome-wide polygenic risk score. Genome Med. 2021;13(1): 16. This study demonstrated the utility and limitations of incorporating individual polygenic risk scores into the current clinic osteoporosis fracture risk algorithm (FRAX Score).
Wu Q, Jung J. Genome-wide polygenic risk score for major osteoporotic fractures in postmenopausal women using associated single nucleotide polymorphisms. J Transl Med. 2023;21(1):127.
Forgetta V, et al. Development of a polygenic risk score to improve screening for fracture risk: a genetic risk prediction study. PLoS Med. 2020;17(7): e1003152.
Nguyen TV, Eisman JA. Post-GWAS polygenic risk score: utility and challenges. JBMR Plus. 2020;4(11): e10411.
Xiao X, Wu Q. Ethnic disparities in fracture risk assessment using polygenic scores. Osteoporos Int. 2023;34(5):943–53.
Polygenic Risk Score Task Force of the International Common Disease, A. Responsible use of polygenic risk scores in the clinic: potential benefits, risks and gaps. Nat Med. 2021;27(11):1876–84.
Krakow D, Rimoin DL. The skeletal dysplasias. Genet Med. 2010;12(6):327–41.
•• Unger S, et al. Nosology of genetic skeletal disorders: 2023 revision. Am J Med Genet A. 2023;191(5):1164–1209. This is the most up-to-date classification system of genetic skeletal disorders and can be used for development of differential diagnosis or curation of genetic testing panels.
• Oheim R, et al. Genetic diagnostics in routine osteological assessment of adult low bone mass disorders. J Clin Endocrinol Metab. 2022;107(7):e3048-e3057. Interesting study that highlights the diagnostic yield of genetic testing in osteoporosis and provides a framework for which patients were most likely to have a causative variant.
Rouleau C, et al. Diagnostic yield of bone fragility gene panel sequencing in children and young adults referred for idiopathic primary osteoporosis at a single regional reference centre. Bone Rep. 2022;16: 101176.
Marom R, Rabenhorst BM, Morello R. Osteogenesis imperfecta: an update on clinical features and therapies. Eur J Endocrinol. 2020;183(4):R95–106.
Bains JS, et al. A Multicenter Observational cohort study to evaluate the effects of bisphosphonate exposure on bone mineral density and other health outcomes in osteogenesis imperfecta. JBMR Plus. 2019;3(5): e10118.
Machol K, et al. Hearing loss in individuals with osteogenesis imperfecta in North America: results from a multicenter study. Am J Med Genet A. 2020;182(4):697–704.
Najirad M, et al. Malocclusion traits and oral health-related quality of life in children with osteogenesis imperfecta: a cross-sectional study. J Am Dent Assoc. 2020;151(7):480-490 e2.
Rodriguez Celin M, et al. A multicenter study to evaluate pain characteristics in osteogenesis imperfecta. Am J Med Genet A. 2023;191(1):160–72.
Tam A, et al. A multicenter study to evaluate pulmonary function in osteogenesis imperfecta. Clin Genet. 2018;94(6):502–11.
Taqi D, et al. Osteogenesis imperfecta tooth level phenotype analysis: cross-sectional study. Bone. 2021;147: 115917.
Steiner RD, Adsit J, Basel D, et al. COL1A1/2-related osteogenesis imperfecta. In: Pagon RA, et al., editors. GeneReviews(R). Seattle: University of Washington, Seattle University of Washington; 1993. (All rights reserved.: Seattle (WA).).
Sillence DO, Senn A, Danks DM. Genetic heterogeneity in osteogenesis imperfecta. J Med Genet. 1979;16(2):101–16.
Zhytnik L, et al. Inter- and intrafamilial phenotypic variability in individuals with collagen-related osteogenesis imperfecta. Clin Transl Sci. 2020;13(5):960–71.
Whyte MP. Hypophosphatasia - aetiology, nosology, pathogenesis, diagnosis and treatment. Nat Rev Endocrinol. 2016;12(4):233–46.
Desborough R, et al. Clinical and biochemical characteristics of adults with hypophosphatasia attending a metabolic bone clinic. Bone. 2021;144: 115795.
Hepp N, et al. Biochemical and clinical manifestations in adults with hypophosphatasia: a national cross-sectional study. Osteoporos Int. 2022;33(12):2595–605.
Baron R, Kneissel M. WNT signaling in bone homeostasis and disease: from human mutations to treatments. Nat Med. 2013;19(2):179–92.
Joeng KS, et al. Osteocyte-specific WNT1 regulates osteoblast function during bone homeostasis. J Clin Invest. 2017;127(7):2678–88.
Joeng KS, et al. The swaying mouse as a model of osteogenesis imperfecta caused by WNT1 mutations. Hum Mol Genet. 2014;23(15):4035–42.
Laine CM, et al. WNT1 mutations in early-onset osteoporosis and osteogenesis imperfecta. N Engl J Med. 2013;368(19):1809–16.
Lawson LY, et al. Loading-induced bone formation is mediated by Wnt1 induction in osteoblast-lineage cells. FASEB J. 2022;36(9): e22502.
Fahiminiya S, et al. Mutations in WNT1 are a cause of osteogenesis imperfecta. J Med Genet. 2013;50(5):345–8.
Alhamdi S, et al. Heterozygous WNT1 variant causing a variable bone phenotype. Am J Med Genet A. 2018;176(11):2419–24.
Makitie RE, et al. Skeletal characteristics of WNT1 osteoporosis in children and young adults. J Bone Miner Res. 2016;31(9):1734–42.
Palomo T, et al. Skeletal characteristics associated with homozygous and heterozygous WNT1 mutations. Bone. 2014;67:63–70.
Cui Y, et al. Lrp5 functions in bone to regulate bone mass. Nat Med. 2011;17(6):684–91.
Ai M, et al. Clinical and molecular findings in osteoporosis-pseudoglioma syndrome. Am J Hum Genet. 2005;77(5):741–53.
Boyden LM, et al. High bone density due to a mutation in LDL-receptor-related protein 5. N Engl J Med. 2002;346(20):1513–21.
Jiao X, et al. Autosomal recessive familial exudative vitreoretinopathy is associated with mutations in LRP5. Am J Hum Genet. 2004;75(5):878–84.
Narumi S, et al. Various types of LRP5 mutations in four patients with osteoporosis-pseudoglioma syndrome: identification of a 7.2-kb microdeletion using oligonucleotide tiling microarray. Am J Med Genet A. 2010;152A(1):133–40.
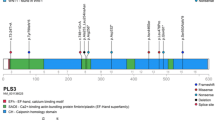
van Dijk FS, et al. PLS3 mutations in X-linked osteoporosis with fractures. N Engl J Med. 2013;369(16):1529–36.
George-Abraham JK, et al. Fractures in children with neurofibromatosis type 1 from two NF clinics. Am J Med Genet A. 2013;161A(5):921–6.
Ireland A, et al. Development of tibia & fibula bone deficits in children with neurofibromatosis type I - a longitudinal case-control comparison. Bone. 2022;154: 116183.
Heerva E, et al. A controlled register-based study of 460 neurofibromatosis 1 patients: increased fracture risk in children and adults over 41 years of age. J Bone Miner Res. 2012;27(11):2333–7.
Charoenngam N, et al. Bone fragility in hereditary connective tissue disorders: a systematic review and meta-analysis. Endocr Pract. 2023;29:589–600.
Haine E, et al. Muscle and bone impairment in children with Marfan syndrome: correlation with age and FBN1 genotype. J Bone Miner Res. 2015;30(8):1369–76.
Coussens M, et al. Bone parameters in hypermobile Ehlers-Danlos syndrome and hypermobility spectrum disorder: a comparative cross-sectional study. Bone. 2023;166: 116583.
Banica T, et al. Higher fracture prevalence and smaller bone size in patients with hEDS/HSD-a prospective cohort study. Osteoporos Int. 2020;31(5):849–56.
Basalom S, Rauch F. Bone disease in patients with Ehlers-Danlos syndromes. Curr Osteoporos Rep. 2020;18(2):95–102.
Gao G, Smith DI. Clinical massively parallel sequencing. Clin Chem. 2020;66(1):77–88.
Schuler BA, Nelson ET, Koziura M, Cogan JD, Hamid R, Phillips JA, 3rd. Lessons learned: next-generation sequencing applied to undiagnosed genetic diseases. J Clin Invest. 2022;132(7). https://doi.org/10.1172/JCI154942.
Bennett RL, French KS, Resta RG, Doyle DL. Standardized human pedigree nomenclature: update and assessment of the recommendations of the National Society of Genetic Counselors. J Genet Couns. 2008;17(5):424–33. https://doi.org/10.1007/s10897-008-9169-9.
Nurchis MC, et al. Whole genome sequencing diagnostic yield for paediatric patients with suspected genetic disorders: systematic review, meta-analysis, and GRADE assessment. Arch Public Health. 2023;81(1):93.
Belkadi A, et al. Whole-genome sequencing is more powerful than whole-exome sequencing for detecting exome variants. Proc Natl Acad Sci U S A. 2015;112(17):5473–8.
Retterer K, et al. Clinical application of whole-exome sequencing across clinical indications. Genet Med. 2016;18(7):696–704.
Sabir AH, et al. Diagnostic yield of rare skeletal dysplasia conditions in the radiogenomics era. BMC Med Genomics. 2021;14(1):148.
• Scocchia A, et al. Diagnostic utility of next-generation sequencing-based panel testing in 543 patients with suspected skeletal dysplasia. Orphanet J Rare Dis. 2021;16(1):412. This study suggests massively paralleled sequencing of approximately 1 in 4 adult patients will return diagnostic results.
GTR: Genetic Testing Registry. Available from: https://www.ncbi.nlm.nih.gov/gtr. Accessed 23 Jan 2024.
Richards S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405–24.
Newey PJ. Approach to the patient with a variant of uncertain significance on genetic testing. Clin Endocrinol (Oxf). 2022;97(4):400–8.
Mighton C, et al. Clinical and psychological outcomes of receiving a variant of uncertain significance from multigene panel testing or genomic sequencing: a systematic review and meta-analysis. Genet Med. 2021;23(1):22–33.
Murdock DR, et al. Transcriptome-directed analysis for Mendelian disease diagnosis overcomes limitations of conventional genomic testing. J Clin Invest. 2021;131(1).
Hirschhorn K, et al. Duty to re-contact. Genet Med. 1999;1(4):171–2.
McInerney-Leo AM, Duncan EL. Massively parallel sequencing for rare genetic disorders: potential and pitfalls. Front Endocrinol (Lausanne). 2020;11: 628946.
Miller DT, et al. ACMG SF v3.2 list for reporting of secondary findings in clinical exome and genome sequencing: a policy statement of the American College of Medical Genetics and Genomics (ACMG). Genet Med. 2023;25:100866.
Kalia SS, et al. Recommendations for reporting of secondary findings in clinical exome and genome sequencing, 2016 update (ACMG SF v2.0): a policy statement of the American College of Medical Genetics and Genomics. Genet Med. 2017;19(2):249–55.
Miller DT, et al. Recommendations for reporting of secondary findings in clinical exome and genome sequencing, 2021 update: a policy statement of the American College of Medical Genetics and Genomics (ACMG). Genet Med. 2021;23(8):1391–8.
Rassie K, et al. Bisphosphonate use and fractures in adults with hypophosphatasia. JBMR Plus. 2019;3(10): e10223.
Lv S, et al. Genetics evaluation of targeted exome sequencing in 223 Chinese probands with genetic skeletal dysplasias. Front Cell Dev Biol. 2021;9: 715042.
Funding
This work was supported in part by the NIH Brittle Bone Disorders Consortium (BBDC) (U54 AR068069). BBDC is a part of the National Center for Advancing Translational Sciences’ (NCATS) Rare Diseases Clinical Research Network (RDCRN), and is funded through a collaboration between NCATS, National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Institute of Dental and Craniofacial Research (NIDCR), National Institute of Mental Health (NIMH), and the Eunice Kennedy Shriver National Institutes of Child Health and Development (NICHD). This work was also supported in part by funding of The Baylor College of Medicine Intellectual and Developmental Disabilities Research Center (P50HD103555) from the Eunice Kennedy Shriver NICHD. This work was funded by the NIH NIDCR (DE031162 and DE031288 to BL), the NHLBI (T32 HL092332 to EB), and the Lawrence Family Bone Disease Program of Texas.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
EB and SCSN declare no competing interests. BL reports non-financial support and other from Baylor Genetics Laboratory, personal fees from Biomarin, other from Acer Therapeutics, other from Sanofi, and other from GQ Bio Therapeutics during the conduct of the study; grants from Sanofi, grants from Kirin Kyowa outside the submitted work.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The mention of trade names, commercial products, or organizations does not imply endorsement by the USA Government.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Busse, E., Lee, B. & Nagamani, S.C.S. Genetic Evaluation for Monogenic Disorders of Low Bone Mass and Increased Bone Fragility: What Clinicians Need to Know. Curr Osteoporos Rep (2024). https://doi.org/10.1007/s11914-024-00870-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s11914-024-00870-6