Abstract
Purpose of Review
The goal of this review is to summarize recent findings related to modifications in osteocyte lacunar and canalicular morphology due to physiological and pathological conditions. In addition, this review aims to outline how these modifications may influence the local mechanical environment of osteocytes and their mechanosensitivity.
Recent Findings
Reduction in lacunar density with age and increasing lacunar size with lactation are confirmed in multiple studies in human and murine bone. There is also evidence of a reduction in canalicular density, length, and branching, as well as increasing sphericity and smaller lacunae with aging and disease. However, while some studies have found modifications in lacunar density, size, shape, and orientation, as well as canalicular density, length, and size due to specific physiological and pathological conditions, others have not observed any differences. Recent finite element models provide insights into how observed modifications in the lacunar-canalicular network (lacunar and canalicular density) and lacunar-canalicular morphology (lacunar area/volume, shape, and orientation as well as canalicular diameter and length) may influence the fluid flow and local strains around the lacunar-canalicular network and modify the local mechanical environment of osteocytes.
Summary
Modifications in the lacunar-canalicular network morphology may lead to significant changes in the strains received by osteocytes and may influence bone’s response to mechanical stimulation as osteocytes are the primary mechanosensing bone cells. Further experimental and computational studies will continue to improve our understanding of the relationship between lacunar-canalicular network morphology and osteocyte mechanosensitivity.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Mori S, Harruff R, Ambrosius W, Burr DB. Trabecular bone volume and microdamage accumulation in the femoral heads of women with and without femoral neck fractures. Bone. 1997;21(6):521–6. https://doi.org/10.1016/S8756-3282(97)00200-7.
Vashishth D, Verborgt O, Divine G, Schaffler MB, Fyhrie DP. Decline in osteocyte lacunar density in human cortical bone is associated with accumulation of microcracks with age. Bone. 2000;26(4):375–80. https://doi.org/10.1016/S8756-3282(00)00236-2.
Ashique AM, Hart LS, Thomas CDL, Clement JG, Pivonka P, Carter Y, et al. Lacunar-canalicular network in femoral cortical bone is reduced in aged women and is predominantly due to a loss of canalicular porosity. Bone Rep. 2017;7:9–16. https://doi.org/10.1016/j.bonr.2017.06.002.
Busse B, Djonic D, Milovanovic P, Hahn M, Puschel K, Ritchie RO, et al. Decrease in the osteocyte lacunar density accompanied by hypermineralized lacunar occlusion reveals failure and delay of remodeling in aged human bone. Aging Cell. 2010;9(6):1065–75. https://doi.org/10.1111/j.1474-9726.2010.00633.x.
Hunter RL, Agnew AM. Intraskeletal variation in human cortical osteocyte lacunar density: implications for bone quality assessment. Bone Reports. 2016;5:252–61. https://doi.org/10.1016/j.bonr.2016.09.002.
Rolvien T, Schmidt FN, Milovanovic P, Jahn K, Riedel C, Butscheidt S, et al. Early bone tissue aging in human auditory ossicles is accompanied by excessive hypermineralization, osteocyte death and micropetrosis. Sci Rep. 2018;8(1):1920. https://doi.org/10.1038/s41598-018-19803-2.
Torres-Lagares D, Tulasne J-F, Pouget C, Llorens A, Saffar J-L, Lesclous P. Structure and remodelling of the human parietal bone: an age and gender histomorphometric study. J Cranio-Maxillofac Surg. 2010;38(5):325–30. https://doi.org/10.1016/j.jcms.2009.07.012.
Bach-Gansmo FL, Brüel A, Jensen MV, Ebbesen EN, Birkedal H, Thomsen JS. Osteocyte lacunar properties and cortical microstructure in human iliac crest as a function of age and sex. Bone. 2016;91:11–9. https://doi.org/10.1016/j.bone.2016.07.003.
Lai X, Price C, Modla S, Thompson WR, Caplan J, Kirn-Safran CB, et al. The dependences of osteocyte network on bone compartment, age, and disease. Bone Res. 2015;3(1):1–11. https://doi.org/10.1038/boneres.2015.9.
• Heveran CM, Rauff A, King KB, Carpenter RD, Ferguson VL. A new open-source tool for measuring 3D osteocyte lacunar geometries from confocal laser scanning microscopy reveals age-related changes to lacunar size and shape in cortical mouse bone. Bone. 2018;110:115–27. https://doi.org/10.1016/j.bone.2018.01.018. This study developed a new tool to assess 3D osteocyte lacunar morphology using confocal laser scanning microscopy images and presented the limitations of 2D measurements on the same images that did not capture age-related changes in lacunar morphology that were observed in 3D assessments.
Tiede-Lewis LM, Xie Y, Hulbert MA, Campos R, Dallas MR, Dusevich V, et al. Degeneration of the osteocyte network in the C57BL/6 mouse model of aging. Aging (Albany NY). 2017;9(10):2190–208. https://doi.org/10.18632/aging.101308.
• Milovanovic P, Zimmermann EA, Riedel C, vom Scheidt A, Herzog L, Krause M, et al. Multi-level characterization of human femoral cortices and their underlying osteocyte network reveal trends in quality of young, aged, osteoporotic and antiresorptive-treated bone. Biomaterials. 2015;45:46–55. https://doi.org/10.1016/j.biomaterials.2014.12.024. This study is one of the very few studies that presented comparative data on osteocyte lacunar density in a human cohort that includes young, old, bisphosphonate-treated, and osteoporotic groups.
Hemmatian H, Laurent MR, Bakker AD, Vanderschueren D, Klein-Nulend J, van Lenthe GH. Age-related changes in female mouse cortical bone microporosity. Bone. 2018;113:1–8. https://doi.org/10.1016/j.bone.2018.05.003.
Jahn-Rickert K, Wolfel EM, Jobke B, Riedel C, Hellmich M, Werner M, et al. Elevated bone hardness under denosumab treatment, with persisting lower osteocyte viability during discontinuation. Front Endocrinol (Lausanne). 2020;11:250. https://doi.org/10.3389/fendo.2020.00250.
Qiu S, Rao DS, Palnitkar S, Parfitt AM. Reduced iliac cancellous osteocyte density in patients with osteoporotic vertebral fracture. J Bone Miner Res. 2003;18(9):1657–63. https://doi.org/10.1359/jbmr.2003.18.9.1657.
Mullender MG, Tan SD, Vico L, Alexandre C, Klein-Nulend J. Differences in osteocyte density and bone histomorphometry between men and women and between healthy and osteoporotic subjects. Calcif Tissue Int. 2005;77(5):291–6. https://doi.org/10.1007/s00223-005-0043-6.
Milovanovic P, Rakocevic Z, Djonic D, Zivkovic V, Hahn M, Nikolic S, et al. Nano-structural, compositional and micro-architectural signs of cortical bone fragility at the superolateral femoral neck in elderly hip fracture patients vs healthy aged controls. Experiment Gerontol. 2014;55:19–28. https://doi.org/10.1016/j.exger.2014.03.001.
Carpentier VT, Wong J, Yeap Y, Gan C, Sutton-Smith P, Badiei A, et al. Increased proportion of hypermineralized osteocyte lacunae in osteoporotic and osteoarthritic human trabecular bone: implications for bone remodeling. Bone. 2012;50(3):688–94. https://doi.org/10.1016/j.bone.2011.11.021.
Misof BM, Blouin S, Andrade VF, Roschger P, Borba VZ, Hartmann MA, et al. No evidence of mineralization abnormalities in iliac bone of premenopausal women with type 2 diabetes mellitus. J Musculoskelet Neuronal Interact. 2022;22(3):305 (https://www.ismni.org/jmni/pdf/89/jmni_22_305.pdf).
Busse B, Bale HA, Zimmermann EA, Panganiban B, Barth HD, Carriero A, et al. Vitamin D deficiency induces early signs of aging in human bone, increasing the risk of fracture. Sci Translat Med. 2013;5(193):193ra88-ra88. https://doi.org/10.1126/scitranslmed.3006286.
Rolvien T, Krause M, Jeschke A, Yorgan T, Püschel K, Schinke T, et al. Vitamin D regulates osteocyte survival and perilacunar remodeling in human and murine bone. Bone. 2017;103:78–87. https://doi.org/10.1016/j.bone.2017.06.022.
Akhter MP, Kimmel D, Lappe JM, Recker RR. Effect of macroanatomic bone type and estrogen loss on osteocyte lacunar properties in healthy adult women. Calcif Tissue Int. 2017;100(6):619–30. https://doi.org/10.1007/s00223-017-0247-6.
Heveran CM, Schurman CA, Acevedo C, Livingston EW, Howe D, Schaible EG, et al. Chronic kidney disease and aging differentially diminish bone material and microarchitecture in C57Bl/6 mice. Bone. 2019;127:91–103. https://doi.org/10.1016/j.bone.2019.04.019.
Zhang D, Miranda M, Li X, Han J, Sun Y, Rojas N, et al. Retention of osteocytic micromorphology by sclerostin antibody in a concurrent ovariectomy and functional disuse model. Ann N Y Acad Sci. 2019;1442(1):91–103. https://doi.org/10.1111/nyas.13991.
Britz HM, Carter Y, Jokihaara J, Leppanen OV, Jarvinen TL, Belev G, et al. Prolonged unloading in growing rats reduces cortical osteocyte lacunar density and volume in the distal tibia. Bone. 2012;51(5):913–9. https://doi.org/10.1016/j.bone.2012.08.112.
Hemmatian H, Jalali R, Semeins CM, Hogervorst J, van Lenthe GH, Klein-Nulend J, et al. Mechanical loading differentially affects osteocytes in fibulae from lactating mice compared to osteocytes in virgin mice: possible role for lacuna size. Calcif Tissue Int. 2018;103(6):675–85. https://doi.org/10.1007/s00223-018-0463-8.
Sang W, Li Y, Guignon J, Liu XS, Ural A. Structural role of osteocyte lacunae on mechanical properties of bone matrix: a cohesive finite element study. J Mech Behav Biomed Mater. 2022;125:104943. https://doi.org/10.1016/j.jmbbm.2021.104943.
Sharma D, Ciani C, Marin PA, Levy JD, Doty SB, Fritton SP. Alterations in the osteocyte lacunar-canalicular microenvironment due to estrogen deficiency. Bone. 2012;51(3):488–97. https://doi.org/10.1016/j.bone.2012.05.014.
Allison H, O’Sullivan LM, McNamara LM. Temporal changes in cortical microporosity during estrogen deficiency associated with perilacunar resorption and osteocyte apoptosis: a pilot study. Bone Rep. 2022;16:101590. https://doi.org/10.1016/j.bonr.2022.101590.
• Carter Y, Thomas CDL, Clement JG, Cooper DML. Femoral osteocyte lacunar density, volume and morphology in women across the lifespan. J Struct Biol. 2013;183(3):519–26. https://doi.org/10.1016/j.jsb.2013.07.004. This study presents comprehensive data on major lacunar properties measured in human bone including lacunar density, volume, and shape as a function of age using three-dimensional measurement techniques.
Dole NS, Yee CS, Mazur CM, Acevedo C, Alliston T. TGFβ regulation of perilacunar/canalicular remodeling is sexually dimorphic. J Bone Miner Res. 2020;35(8):1549–61. https://doi.org/10.1002/jbmr.4023.
Kaya S, Basta-Pljakic J, Seref-Ferlengez Z, Majeska RJ, Cardoso L, Bromage TG, et al. Lactation-induced changes in the volume of osteocyte lacunar-canalicular space alter mechanical properties in cortical bone tissue. J Bone Miner Res. 2017;32(4):688–97. https://doi.org/10.1002/jbmr.3090.
Jähn K, Kelkar S, Zhao H, Xie Y, Tiede-Lewis LM, Dusevich V, et al. Osteocytes acidify their microenvironment in response to PTHrP in vitro and in lactating mice in vivo. J Bone Miner Res. 2017;32(8):1761–72. https://doi.org/10.1002/jbmr.3167.
Qing H, Ardeshirpour L, Divieti Pajevic P, Dusevich V, Jähn K, Kato S, et al. Demonstration of osteocytic perilacunar/canalicular remodeling in mice during lactation. J Bone Miner Res. 2012;27(5):1018–29. https://doi.org/10.1002/jbmr.1567.
Li Y, de Bakker CM, Lai X, Zhao H, Parajuli A, Tseng W-J, et al. Maternal bone adaptation to mechanical loading during pregnancy, lactation, and post-weaning recovery. Bone. 2021;151:116031. https://doi.org/10.1016/j.bone.2021.116031.
van Hove RP, Nolte PA, Vatsa A, Semeins CM, Salmon PL, Smit TH, et al. Osteocyte morphology in human tibiae of different bone pathologies with different bone mineral density–is there a role for mechanosensing? Bone. 2009;45(2):321–9. https://doi.org/10.1016/j.bone.2009.04.238.
Tokarz D, Martins JS, Petit ET, Lin CP, Demay MB, Liu ES. Hormonal regulation of osteocyte perilacunar and canalicular remodeling in the Hyp mouse model of X-linked hypophosphatemia. J Bone Miner Res. 2018;33(3):499–509. https://doi.org/10.1002/jbmr.3327.
Dole NS, Mazur CM, Acevedo C, Lopez JP, Monteiro DA, Fowler TW, et al. Osteocyte-intrinsic TGF-β signaling regulates bone quality through perilacunar/canalicular remodeling. Cell Rep. 2017;21(9):2585–96. https://doi.org/10.1016/j.celrep.2017.10.115.
Hemmatian H, Conrad S, Furesi G, Mletzko K, Krug J, Faila AV, et al. Reorganization of the osteocyte lacuno-canalicular network characteristics in tumor sites of an immunocompetent murine model of osteotropic cancers. Bone. 2021;152:116074. https://doi.org/10.1016/j.bone.2021.116074.
Ma Y-L, Dai R-C, Sheng Z-F, Jin Y, Zhang Y-H, Fang L-N, et al. Quantitative associations between osteocyte density and biomechanics, microcrack and microstructure in OVX rats vertebral trabeculae. J Biomech. 2008;41(6):1324–32. https://doi.org/10.1016/j.jbiomech.2008.01.017.
Zimmermann EA, Schaible E, Gludovatz B, Schmidt FN, Riedel C, Krause M, et al. Intrinsic mechanical behavior of femoral cortical bone in young, osteoporotic and bisphosphonate-treated individuals in low-and high energy fracture conditions. Sci Rep. 2016;6:21072.
Lowe DA, Lepori-Bui N, Fomin PV, Sloofman LG, Zhou X, Farach-Carson MC, et al. Deficiency in perlecan/HSPG2 during bone development enhances osteogenesis and decreases quality of adult bone in mice. Calcif Tissue Int. 2014;95(1):29–38. https://doi.org/10.1007/s00223-014-9859-2.
Zeng QQ, Jee WSS, Bigornia AE, King JG, D’Souza SM, Li XJ, et al. Time responses of cancellous and cortical bones to sciatic neurectomy in growing female rats. Bone. 1996;19(1):13–21. https://doi.org/10.1016/8756-3282(96)00112-3.
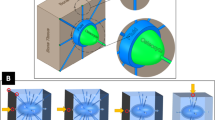
Sang W, Ural A. Evaluating the role of canalicular morphology and perilacunar region properties on local mechanical environment of lacunar-canalicular network using finite element modeling. J Biomech Eng 2023;145(6):061006. https://doi.org/10.1115/1.4056655.
• Sang W, Ural A. Quantifying how altered lacunar morphology and perilacunar tissue properties influence local mechanical environment of osteocyte lacunae using finite element modeling. J Mech Behav Biomed Mater. 2022;135:105433. https://doi.org/10.1016/j.jmbbm.2022.105433. This study developed a 3D FE modeling approach that incorporated varying lacunar morphology and provided detailed information about how the local mechanical environment changes with modifications in lacunar morphology.
Vashishth D, Gibson GJ, Fyhrie DP. Sexual dimorphism and age dependence of osteocyte lacunar density for human vertebral cancellous bone. Anat Rec A Discov Mol Cell Evol Biol. 2005;282A(2):157–62. https://doi.org/10.1002/ar.a.20146.
Hemmatian H, Bakker AD, Klein-Nulend J, van Lenthe GH. Alterations in osteocyte lacunar morphology affect local bone tissue strains. J Mech Behav Biomed Mater. 2021;123:104730. https://doi.org/10.1016/j.jmbbm.2021.104730.
Kola SK, Begonia MT, Tiede-Lewis LM, Laughrey LE, Dallas SL, Johnson ML, et al. Osteocyte lacunar strain determination using multiscale finite element analysis. Bone Reports. 2020;12: 100277.
• Lai X, Chung R, Li Y, Liu XS, Wang L. Lactation alters fluid flow and solute transport in maternal skeleton: a multiscale modeling study on the effects of microstructural changes and loading frequency. Bone. 2021;151:116033. https://doi.org/10.1016/j.bone.2021.116033. This study developed a model that evaluated the influence of morphological changes in the LCN due to lactation and loading frequency on load-induced fluid flow in LCN.
VanHouten JN, Wysolmerski JJ. Low estrogen and high parathyroid hormone-related peptide levels contribute to accelerated bone resorption and bone loss in lactating mice. Endocrinology. 2003;144(12):5521–9. https://doi.org/10.1210/en.2003-0892.
Bacabac RG, Mizuno D, Schmidt CF, MacKintosh FC, Van Loon JJ, Klein-Nulend J, et al. Round versus flat: bone cell morphology, elasticity, and mechanosensing. J Biomech. 2008;41(7):1590–8. https://doi.org/10.1016/j.jbiomech.2008.01.031.
Lewis KJ, Cabahug-Zuckerman P, Boorman-Padgett JF, Basta-Pljakic J, Louie J, Stephen S, et al. Estrogen depletion on In vivo osteocyte calcium signaling responses to mechanical loading. Bone. 2021;152:116072. https://doi.org/10.1016/j.bone.2021.116072.
Wu V, van Oers RFM, Schulten E, Helder MN, Bacabac RG, Klein-Nulend J. Osteocyte morphology and orientation in relation to strain in the jaw bone. Int J Oral Sci. 2018;10(1):2. https://doi.org/10.1038/s41368-017-0007-5.
Carter Y, Suchorab JL, Thomas CDL, Clement JG, Cooper DM. Normal variation in cortical osteocyte lacunar parameters in healthy young males. J Anat. 2014;225(3):328–36. https://doi.org/10.1111/joa.12213.
Marotti G. Osteocyte orientation in human lamellar bone and its relevance to the morphometry of periosteocytic lacunae. Metab Bone Dis Relat Res. 1979;1(4):325–33. https://doi.org/10.1016/0221-8747(79)90027-4.
van Oers RF, Wang H, Bacabac RG. Osteocyte shape and mechanical loading. Curr Osteoporos Rep. 2015;13(2):61–6. https://doi.org/10.1007/s11914-015-0256-1.
Gauthier R, Langer M, Follet H, Olivier C, Gouttenoire P-J, Helfen L, et al. 3D micro structural analysis of human cortical bone in paired femoral diaphysis, femoral neck and radial diaphysis. J Struct Biol. 2018;204(2):182–90. https://doi.org/10.1016/j.jsb.2018.08.006.
Carter Y, Thomas CDL, Clement JG, Peele AG, Hannah K, Cooper DML. Variation in osteocyte lacunar morphology and density in the human femur — a synchrotron radiation micro-CT study. Bone. 2013;52(1):126–32. https://doi.org/10.1016/j.bone.2012.09.010.
Qiu S, Sudhaker Rao D, Fyhrie DP, Palnitkar S, Parfitt AM. The morphological association between microcracks and osteocyte lacunae in human cortical bone. Bone. 2005;37(1):10–5. https://doi.org/10.1016/j.bone.2005.01.023.
Rolvien T, Vom Scheidt A, Stockhausen KE, Milovanovic P, Djonic D, Hubert J, et al. Inter-site variability of the osteocyte lacunar network in the cortical bone underpins fracture susceptibility of the superolateral femoral neck. Bone. 2018;112:187–93. https://doi.org/10.1016/j.bone.2018.04.018.
von Kroge S, Stürznickel J, Bechler U, Stockhausen KE, Eissele J, Hubert J, et al. Impaired bone quality in the superolateral femoral neck occurs independent of hip geometry and bone mineral density. Acta Biomater. 2022;141:233–43. https://doi.org/10.1016/j.actbio.2022.01.002.
Goff E, Cohen A, Shane E, Recker RR, Kuhn G, Muller R. Large-scale osteocyte lacunar morphological analysis of transiliac bone in normal and osteoporotic premenopausal women. Bone. 2022;160:116424. https://doi.org/10.1016/j.bone.2022.116424.
Milovanovic P, Zimmermann EA, Hahn M, Djonic D, Püschel K, Djuric M, et al. Osteocytic canalicular networks: morphological implications for altered mechanosensitivity. ACS Nano. 2013;7(9):7542–51. https://doi.org/10.1021/nn401360u.
Kobayashi K, Nojiri H, Saita Y, Morikawa D, Ozawa Y, Watanabe K, et al. Mitochondrial superoxide in osteocytes perturbs canalicular networks in the setting of age-related osteoporosis. Sci Rep. 2015;5(1):9148. https://doi.org/10.1038/srep09148.
• Schurman CA, Verbruggen SW, Alliston T. Disrupted osteocyte connectivity and pericellular fluid flow in bone with aging and defective TGF-β signaling. Proc Nat Acad Sci. 2021;118(25):e2023999118. https://doi.org/10.1073/pnas.2023999118. This study presented detailed data on changes in canalicular architecture with age and with defective TGF-β signaling in mice bone as well as computational fluid dynamics simulations that showed the influence of changes in canalicular architecture on fluid flow.
Ciani A, Toumi H, Pallu S, Tsai EHR, Diaz A, Guizar-Sicairos M, et al. Ptychographic X-ray CT characterization of the osteocyte lacuno-canalicular network in a male rat’s glucocorticoid induced osteoporosis model. Bone Reports. 2018;9:122–31. https://doi.org/10.1016/j.bonr.2018.07.005.
Alemi AS, Mazur CM, Fowler TW, Woo JJ, Knott PD, Alliston T. Glucocorticoids cause mandibular bone fragility and suppress osteocyte perilacunar-canalicular remodeling. Bone Rep. 2018;9:145–53. https://doi.org/10.1016/j.bonr.2018.09.004.
Fowler TW, Acevedo C, Mazur CM, Hall-Glenn F, Fields AJ, Bale HA, et al. Glucocorticoid suppression of osteocyte perilacunar remodeling is associated with subchondral bone degeneration in osteonecrosis. Sci Rep. 2017;7(1):1–13. https://doi.org/10.1038/srep44618.
Han Y, Cowin SC, Schaffler MB, Weinbaum S. Mechanotransduction and strain amplification in osteocyte cell processes. Proc Natl Acad Sci. 2004;101(47):16689–94. https://doi.org/10.1073/pnas.0407429101.
Acknowledgements
Wen Sang was supported by Villanova University College of Engineering during this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Wen Sang and Ani Ural declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sang, W., Ural, A. Influence of Osteocyte Lacunar-Canalicular Morphology and Network Architecture on Osteocyte Mechanosensitivity. Curr Osteoporos Rep 21, 401–413 (2023). https://doi.org/10.1007/s11914-023-00792-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-023-00792-9