Abstract
Purpose of Review
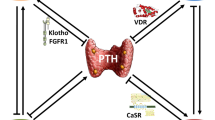
Chronic kidney disease mineral and bone disease (CKD-MBD) is a common complication of kidney disease and is strongly influenced by diet. The purpose of this manuscript is to review recent advances in the role of diet in CKD-MBD over the last 5 years.
Recent Findings
Many of the recent studies examining the role of diet in CKD-MBD have focused on the adverse effects of high phosphorus consumption on bone health and metabolism. In general, the studies have shown that high phosphorus consumption worsens markers of bone and mineral metabolism but that eating a diet with a calcium to phosphorus ratio closer to 1:1 can attenuate some of these effects. Recent studies also showed that dietary counseling is efficacious for improving markers of CKD-MBD.
Summary
High consumption of phosphorus aggravates CKD-MBD. Dietary counseling may ameliorate these effects, for example, by consuming diets with higher calcium to phosphorus ratios.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Moe S, Drüeke T, Cunningham J, Goodman W, Martin K, Olgaard K, Ott S, Sprague S, Lameire N, Eknoyan G, Kidney Disease: Improving Global Outcomes (KDIGO), et al. Definition, evaluation, and classification of renal osteodystrophy: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney International. 2006;69(11):1945–53. https://doi.org/10.1038/sj.ki.5000414.
Gutiérrez OM. Fibroblast growth factor 23 and disordered vitamin D metabolism in chronic kidney disease: updating the "trade-off" hypothesis. Clin J Am Soc Nephrol. 2010;5(9):1710–6. https://doi.org/10.2215/cjn.02640310.
Alem AM, Sherrard DJ, Gillen DL, Weiss NS, Beresford SA, Heckbert SR, Wong C, Stehman-Breen C. Increased risk of hip fracture among patients with end-stage renal disease. Kidney Int. 2000;58(1):396–9. https://doi.org/10.1046/j.1523-1755.2000.00178.x.
Kim SM, Long J, Montez-Rath M, Leonard M, Chertow GM. Hip fracture in patients with non-dialysis-requiring chronic kidney disease. J Bone Miner Res. 2016;31(10):1803–9. https://doi.org/10.1002/jbmr.2862.
Barsotti G, Cupisti A, Morelli E, Meola M, Cozza V, Barsotti M, Giovannetti S. Secondary hyperparathyroidism in severe chronic renal failure is corrected by very-low dietary phosphate intake and calcium carbonate supplementation. Nephron. 1998;79(2):137–41.
Combe C, Aparicio M. Phosphorus and protein restriction and parathyroid function in chronic renal failure. Kidney Int. 1994;46(5):1381–6.
Combe C, Morel D, de Precigout V, Blanchetier V, Bouchet JL, Potaux L, et al. Long-term control of hyperparathyroidism in advanced renal failure by low-phosphorus low-protein diet supplemented with calcium (without changes in plasma calcitriol). Nephron. 1995;70(3):287–95.
Gonzalez-Parra E, Gonzalez-Casaus ML, Galan A, Martinez-Calero A, Navas V, Rodriguez M, Ortiz A. Lanthanum carbonate reduces FGF23 in chronic kidney disease stage 3 patients. Nephrol Dial Transplant. 2011;26(8):2567–71. https://doi.org/10.1093/ndt/gfr144.
Kaye M. The effects in the rat of varying intakes of dietary calcium, phosphorus, and hydrogen ion on hyperparathyroidism due to chronic renal failure. J Clin Invest. 1974;53(1):256–69.
Lafage MH, Combe C, Fournier A, Aparicio M. Ketodiet, physiological calcium intake and native vitamin D improve renal osteodystrophy. Kidney Int. 1992;42(5):1217–25.
Oliveira RB, Cancela AL, Graciolli FG, Dos Reis LM, Draibe SA, Cuppari L, et al. Early control of PTH and FGF23 in normophosphatemic CKD patients: a new target in CKD-MBD therapy? Clin J Am Soc Nephrol. 2010;5(2):286–91. https://doi.org/10.2215/CJN.05420709.
Slatopolsky E, Caglar S, Gradowska L, Canterbury J, Reiss E, Bricker NS. On the prevention of secondary hyperparathyroidism in experimental chronic renal disease using "proportional reduction" of dietary phosphorus intake. Kidney Int. 1972;2(3):147–51.
Khairallah P, Nickolas TL. Management of osteoporosis in CKD. Clin J Am Soc Nephrol. 2018;13(6):962–9. https://doi.org/10.2215/cjn.11031017.
Uribarri J. Phosphorus homeostasis in normal health and in chronic kidney disease patients with special emphasis on dietary phosphorus intake. Semin Dial. 2007;20(4):295–301.
Gutiérrez OM. The connection between dietary phosphorus, cardiovascular disease, and mortality: where we stand and what we need to know. Adv Nutr. 2013;4(6):723–9. https://doi.org/10.3945/an.113.004812.
Watanabe A, Koizumi T, Horikawa T, Sano Y, Uki H, Miyajima K, Kemuriyama N, Anzai R, Iwata H, Anzai T, Nakagawa K, Nakae D. Impact of altered dietary calcium-phosphorus ratio caused by high-phosphorus diets in a rat chronic kidney disease (CKD) model created by partial ligation of the renal arteries. J Toxicol Pathol. 2020;33(2):77–86. https://doi.org/10.1293/tox.2019-0086.
Ugrica M, Bettoni C, Bourgeois S, Daryadel A, Pastor-Arroyo EM, Gehring N, Hernando N, Wagner CA, Rubio-Aliaga I. A chronic high phosphate intake in mice is detrimental for bone health without major renal alterations. Nephrol Dial Transplant. 2021;36:1183–91. https://doi.org/10.1093/ndt/gfab015.
Sax L. The institute of medicine's "dietary reference intake" for phosphorus: a critical perspective. J Am Coll Nutr. 2001;20(4):271–8. https://doi.org/10.1080/07315724.2001.10719047.
Gutiérrez OM, Porter AK, Viggeswarapu M, Roberts JL, Beck GR Jr. Effects of phosphorus and calcium to phosphorus consumption ratio on mineral metabolism and cardiometabolic health. J Nutr Biochem. 2020;80:108374. https://doi.org/10.1016/j.jnutbio.2020.108374.
• Gutiérrez OM, Luzuriaga-McPherson A, Lin Y, Gilbert LC, Ha SW, Beck GR Jr. Impact of phosphorus-based food additives on bone and mineral metabolism. J Clin Endocrinol Metab. 2015;100(11):4264–71. https://doi.org/10.1210/jc.2015-2279This study provided evidence for the importance of the calcium:phosphorus ratio in the manifestations of CKD-MBD.
Wang L, Tang R, Zhang Y, Liu Z, Chen S, Song K, Guo Y, Zhang L, Wang X, Wang X, Liu H, Zhang X, Liu BC. A rat model with multivalve calcification induced by subtotal nephrectomy and high-phosphorus diet. Kidney Dis (Basel). 2020;6(5):346–54. https://doi.org/10.1159/000506013.
Aniteli TM, de Siqueira FR, Dos Reis LM, Dominguez WV, de Oliveira EMC, Castelucci P, et al. Effect of variations in dietary Pi intake on intestinal Pi transporters (NaPi-IIb, PiT-1, and PiT-2) and phosphate-regulating factors (PTH, FGF-23, and MEPE). Pflugers Arch. 2018;470(4):623–32. https://doi.org/10.1007/s00424-018-2111-6.
• Yamada S, Leaf EM, Chia JJ, Cox TC, Speer MY, Giachelli CM. PiT-2, a type III sodium-dependent phosphate transporter, protects against vascular calcification in mice with chronic kidney disease fed a high-phosphate diet. Kidney Int. 2018;94(4):716–27. https://doi.org/10.1016/j.kint.2018.05.015This study looked at differing calcium:phosphorus ratios on both circulating markers of CKD-MBD and bone histological manifestations.
Byrne FN, Gillman BA, Kiely M, Palmer B, Shiely F, Kearney PM, Earlie J, Bowles MB, Keohane FM, Connolly PP, Wade S, Rennick TA, Moore BL, Smith ON, Sands CM, Slevin O, McCarthy DC, Brennan KM, Mellett H, et al. Pilot randomized controlled trial of a standard versus a modified low-phosphorus diet in hemodialysis patients. Kidney Int Rep. 2020;5(11):1945–55. https://doi.org/10.1016/j.ekir.2020.08.008.
• Lim E, Hyun S, Lee JM, Kim S, Lee MJ, Lee SM, et al. Effects of education on low-phosphate diet and phosphate binder intake to control serum phosphate among maintenance hemodialysis patients: a randomized controlled trial. Kidney Res Clin Pract. 2018;37(1):69–76. https://doi.org/10.23876/j.krcp.2018.37.1.69An important study looking at differing calcium:phosphorus ratios on bone histological disease in CKD.
Moe SM. Rationale to reduce calcium intake in adult patients with chronic kidney disease. Curr Opin Nephrol Hypertens. 2018;27(4):251–7. https://doi.org/10.1097/mnh.0000000000000416.
• Moe SM, Zidehsarai MP, Chambers MA, Jackman LA, Radcliffe JS, Trevino LL, Donahue SE, Asplin JR. Vegetarian compared with meat dietary protein source and phosphorus homeostasis in chronic kidney disease. Clin J Am Soc Nephrol. 2011;6(2):257–64. https://doi.org/10.2215/CJN.05040610This study showed the importance of phosphorus co-transporters in the gut in modulating the effects of diet intake on CKD-MBD.
Shigematsu T, Negi S. Combined therapy with lanthanum carbonate and calcium carbonate for hyperphosphatemia decreases serum FGF-23 level independently of calcium and PTH (COLC Study). Nephrol Dial Transplant. 2012;27(3):1050–4. https://doi.org/10.1093/ndt/gfr388.
•• Slatopolsky E, Caglar S, Pennell JP, Taggart DD, Canterbury JM, Reiss E, Bricker NS. On the pathogenesis of hyperparathyroidism in chronic experimental renal insufficiency in the dog. J Clin Invest. 1971;50(3):492–9 This study provided critical new evidence that low urine phosphorus excretion may be a stronger signal of whole body retention of phosphorus than lower phosphorus intake per se.
Pazianas M, Miller PD. Osteoporosis and chronic kidney disease-mineral and bone disorder (CKD-MBD): back to basics. Am J Kidney Dis. 2021;78:582–9. https://doi.org/10.1053/j.ajkd.2020.12.024.
Hou HT, Wang YN, Shao SZ, Fu S, Huang XP, Wang XH. High calcium diet alleviates 5/6 nephrectomy-induced bone deteriorations of lumbar vertebrae in mice. Exp Ther Med. 2018;15(4):3483–8. https://doi.org/10.3892/etm.2018.5866.
• Stremke ER, McCabe LD, McCabe GP, Martin BR, Moe SM, Weaver CM, et al. Twenty-four-hour urine phosphorus as a biomarker of dietary phosphorus intake and absorption in CKD: a secondary analysis from a controlled diet balance study. Clin J Am Soc Nephrol. 2018;13(7):1002–12. https://doi.org/10.2215/cjn.00390118This study provides a nice meta-analysis of various studies showing a potential beneficial effect of diet counseling on circulating parameters of CKD-MBD in hemodialysis patients.
St-Jules DE, Rozga MR, Handu D, Carrero JJ. Effect of phosphate-specific diet therapy on phosphate levels in adults undergoing maintenance hemodialysis: a systematic review and meta-analysis. Clin J Am Soc Nephrol. 2020;16(1):107–20. https://doi.org/10.2215/cjn.09360620.
Funding
Dr. Gutiérrez was supported by grant K24DK116180 from the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Gutierrez reports receiving grant support and honoraria from Amgen and Akebia; grant support from GSK; honoraria from AstraZeneca, Ardelyx, and Reata; and serving on the Data Monitoring Committee for QED Therapeutics.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Kidney and Bone
Rights and permissions
About this article
Cite this article
Gutiérrez, O.M. Recent Advances in the Role of Diet in Bone and Mineral Disorders in Chronic Kidney Disease. Curr Osteoporos Rep 19, 574–579 (2021). https://doi.org/10.1007/s11914-021-00710-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-021-00710-x