Abstract
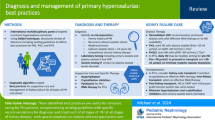
Purpose of Review
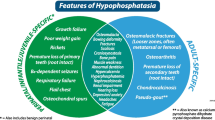
X-linked hypophosphatemia and tumor-induced osteomalacia are diseases characterized by hypophosphatemia with impaired proximal tubular phosphate reabsorption. Complete resection of responsible tumors is the first-line therapy for patients with tumor-induced osteomalacia. In contrast, phosphate and active vitamin D have been used for patients with X-linked hypophosphatemia and inoperable ones with tumor-induced osteomalacia. The purpose of this review is to summarize the pathogenesis of these diseases and discuss about the new treatment.
Recent Findings
Excessive FGF23 production has been shown to underline several kinds of hypophosphatemic rickets/osteomalacia including X-linked hypophosphatemia and tumor-induced osteomalacia. Burosumab, an anti-FGF23 monoclonal antibody, was approved for clinical use, while the indications of burosumab are different depending on countries.
Summary
The inhibition of excessive FGF23 activity has been approved as a new therapy for several kinds of hypophosphatemic diseases. Further studies are necessary to clarify the long-term effects and safety of burosumab.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kinoshita Y, Fukumoto S. X-linked hypophosphatemia and FGF23-related hypophosphatemic diseases: prospect for new treatment. Endocr Rev. 2018;39(3):274–91. https://doi.org/10.1210/er.2017-00220.
Levine BS, Kleeman CR, Felsenfeld AJ. The journey from vitamin D-resistant rickets to the regulation of renal phosphate transport. Clin J Am Soc Nephrol. 2009;4(11):1866–77. https://doi.org/10.2215/cjn.03000509.
ADHR Consortium Autosomal dominant hypophosphataemic rickets is associated with mutations in FGF23. Nat Genet. 2000;26(3):345–8. https://doi.org/10.1038/81664.
Yamashita T, Yoshioka M, Itoh N. Identification of a novel fibroblast growth factor, FGF-23, preferentially expressed in the ventrolateral thalamic nucleus of the brain. Biochem Biophys Res Commun. 2000;277(2):494–8. https://doi.org/10.1006/bbrc.2000.3696.
Shimada T, Mizutani S, Muto T, Yoneya T, Hino R, Takeda S, Takeuchi Y, Fujita T, Fukumoto S, Yamashita T. Cloning and characterization of FGF23 as a causative factor of tumor-induced osteomalacia. Proc Natl Acad Sci U S A. 2001;98(11):6500–5. https://doi.org/10.1073/pnas.101545198.
Shimada T, Muto T, Urakawa I, Yoneya T, Yamazaki Y, Okawa K, Takeuchi Y, Fujita T, Fukumoto S, Yamashita T. Mutant FGF-23 responsible for autosomal dominant hypophosphatemic rickets is resistant to proteolytic cleavage and causes hypophosphatemia in vivo. Endocrinology. 2002;143(8):3179–82.https://doi.org/10.1210/endo.143.8.8795
Sitara D, Razzaque MS, Hesse M, Yoganathan S, Taguchi T, Erben RG, J+APw-ppner H, Lanske B. Homozygous ablation of fibroblast growth factor-23 results in hyperphosphatemia and impaired skeletogenesis, and reverses hypophosphatemia in Phex-deficient mice. Matrix Biol. 2004;23(7):421–32. https://doi.org/10.1016/j.matbio.2004.09.007.
Urakawa I, Yamazaki Y, Shimada T, Iijima K, Hasegawa H, Okawa K, Fujita T, Fukumoto S, Yamashita T. Klotho converts canonical FGF receptor into a specific receptor for FGF23. Nature. 2006;444(7120):770–4. https://doi.org/10.1038/nature05315.
Shimada T, Hasegawa H, Yamazaki Y, Muto T, Hino R, Takeuchi Y, Fujita T, Nakahara K, Fukumoto S, Yamashita T. FGF-23 is a potent regulator of vitamin D metabolism and phosphate homeostasis. J Bone Miner Res. 2004;19(3):429–35. https://doi.org/10.1359/jbmr.0301264.
Jonsson KB, Zahradnik R, Larsson T, White KE, Sugimoto T, Imanishi Y, Yamamoto T, Hampson G, Koshiyama H, Ljunggren Ö, Oba K, Yang IM, Miyauchi A, Econs MJ, Lavigne J, Jüppner H. Fibroblast growth factor 23 in oncogenic osteomalacia and X-linked hypophosphatemia. N Engl J Med. 2003;348(17):1656–63. https://doi.org/10.1056/NEJMoa020881.
Yamazaki Y, Okazaki R, Shibata M, Hasegawa Y, Satoh K, Tajima T, Takeuchi Y, Fujita T, Nakahara K, Yamashita T, Fukumoto S. Increased circulatory level of biologically active full-length FGF-23 in patients with hypophosphatemic rickets/osteomalacia. J Clin Endocrinol Metab. 2002;87(11):4957–60. https://doi.org/10.1210/jc.2002-021105.
Endo I, Fukumoto S, Ozono K, Namba N, Tanaka H, Inoue D, Minagawa M, Sugimoto T, Yamauchi M, Michigami T, Matsumoto T. Clinical usefulness of measurement of fibroblast growth factor 23 (FGF23) in hypophosphatemic patients: proposal of diagnostic criteria using FGF23 measurement. Bone. 2008;42(6):1235–9. https://doi.org/10.1016/j.bone.2008.02.014.
Imel EA, Hui SL, Econs MJ. FGF23 concentrations vary with disease status in autosomal dominant hypophosphatemic rickets. J Bone Miner Res. 2007;22(4):520–6. https://doi.org/10.1359/jbmr.070107.
Endo I, Fukumoto S, Ozono K, Namba N, Inoue D, Okazaki R, Yamauchi M, Sugimoto T, Minagawa M, Michigami T, Nagai M, Matsumoto T. Nationwide survey of fibroblast growth factor 23 (FGF23)-related hypophosphatemic diseases in Japan: prevalence, biochemical data and treatment. Endocr J. 2015;62(9):811–6. https://doi.org/10.1507/endocrj.EJ15-0275.
The HYP Consortium. A gene (PEX) with homologies to endopeptidases is mutated in patients with X-linked hypophosphatemic rickets. Nat Genet. 1995;11(2):130–6. https://doi.org/10.1038/ng1095-130.
Beck L, Soumounou Y, Martel J, Krishnamurthy G, Gauthier C, Goodyer CG, Tenenhouse HS. Pex/PEX tissue distribution and evidence for a deletion in the 3' region of the Pex gene in X-linked hypophosphatemic mice. J Clin Invest. 1997;99(6):1200–9. https://doi.org/10.1172/jci119276.
Yuan B, Takaiwa M, Clemens TL, Feng JQ, Kumar R, Rowe PS, Xie Y, Drezner MK. Aberrant Phex function in osteoblasts and osteocytes alone underlies murine X-linked hypophosphatemia. J Clin Invest. 2008;118(2):722–34. https://doi.org/10.1172/jci32702.
Fukumoto S. FGF23-related hypophosphatemic rickets/osteomalacia: diagnosis and new treatment. J Mol Endocrinol. 2021;66(2):R57–r65. https://doi.org/10.1530/jme-20-0089.
Folpe AL, Fanburg-Smith JC, Billings SD, Bisceglia M, Bertoni F, Cho JY, Econs MJ, Inwards CY, Jan de Beur SM, Mentzel T, Montgomery E, Michal M, Miettinen M, Mills SE, Reith JD, O'Connell JX, Rosenberg AE, Rubin BP, Sweet DE, et al. Most osteomalacia-associated mesenchymal tumors are a single histopathologic entity: an analysis of 32 cases and a comprehensive review of the literature. Am J Surg Pathol. 2004;28(1):1–30. https://doi.org/10.1097/00000478-200401000-00001
Lee JC, Jeng YM, Su SY, Wu CT, Tsai KS, Lee CH, Lin CY, Carter JM, Huang JW, Chen SH, Shih SR, Mariño-Enríquez A, Chen CC, Folpe AL, Chang YL, Liang CW. Identification of a novel FN1-FGFR1 genetic fusion as a frequent event in phosphaturic mesenchymal tumour. J Pathol. 2015;235(4):539–45. https://doi.org/10.1002/path.4465.
Lee JC, Su SY, Changou CA, Yang RS, Tsai KS, Collins MT, Orwoll ES, Lin CY, Chen SH, Shih SR, Lee CH, Oda Y, Billings SD, Li CF, Nielsen GP, Konishi E, Petersson F, Carpenter TO, Sittampalam K, et al. Characterization of FN1-FGFR1 and novel FN1-FGF1 fusion genes in a large series of phosphaturic mesenchymal tumors. Mod Pathol. 2016;29(11):1335–46. https://doi.org/10.1038/modpathol.2016.137.
Kinoshita Y, Takashi Y, Ito N, Ikegawa S, Mano H, Ushiku T, Fukayama M, Nangaku M, Fukumoto S. Ectopic expression of Klotho in fibroblast growth factor 23 (FGF23)-producing tumors that cause tumor-induced rickets/osteomalacia (TIO). Bone Rep. 2019;10:100192. https://doi.org/10.1016/j.bonr.2018.100192.
Takashi Y, Kosako H, Sawatsubashi S, Kinoshita Y, Ito N, Tsoumpra MK, Nangaku M, Abe M, Matsuhisa M, Kato S, Matsumoto T, Fukumoto S. Activation of unliganded FGF receptor by extracellular phosphate potentiates proteolytic protection of FGF23 by its O-glycosylation. Proc Natl Acad Sci U S A. 2019;116(23):11418–27. https://doi.org/10.1073/pnas.1815166116.
Schouten B, Hunt P, Livesey J, Frampton C, Soule S. FGF23 elevation and hypophosphatemia after intravenous iron polymaltose: a prospective study. J Clin Endocrinol Metab. 2009;94(7):2332–7. https://doi.org/10.1210/jc.2008-2396.
Shimizu Y, Tada Y, Yamauchi M, Okamoto T, Suzuki H, Ito N, Fukumoto S, Sugimoto T, Fujita T. Hypophosphatemia induced by intravenous administration of saccharated ferric oxide: another form of FGF23-related hypophosphatemia. Bone. 2009;45(4):814–6. https://doi.org/10.1016/j.bone.2009.06.017.
Wolf M, Koch TA, Bregman DB. Effects of iron deficiency anemia and its treatment on fibroblast growth factor 23 and phosphate homeostasis in women. J Bone Miner Res. 2013;28(8):1793–803. https://doi.org/10.1002/jbmr.1923.
Glorieux FH, Marie PJ, Pettifor JM, Delvin EE. Bone response to phosphate salts, ergocalciferol, and calcitriol in hypophosphatemic vitamin D-resistant rickets. N Engl J Med. 1980;303(18):1023–31. https://doi.org/10.1056/nejm198010303031802.
Sullivan W, Carpenter T, Glorieux F, Travers R, Insogna K. A prospective trial of phosphate and 1,25-dihydroxyvitamin D3 therapy in symptomatic adults with X-linked hypophosphatemic rickets. J Clin Endocrinol Metab. 1992;75(3):879–85. https://doi.org/10.1210/jcem.75.3.1517380.
Carpenter TO, Imel EA, Holm IA, Jan de Beur SM, Insogna KL. A clinician’s guide to X-linked hypophosphatemia. J Bone Miner Res. 2011;26(7):1381–8. https://doi.org/10.1002/jbmr.340.
Goetz R, Nakada Y, Hu MC, Kurosu H, Wang L, Nakatani T, Shi M, Eliseenkova AV, Razzaque MS, Moe OW, Kuro-o M, Mohammadi M. Isolated C-terminal tail of FGF23 alleviates hypophosphatemia by inhibiting FGF23-FGFR-Klotho complex formation. Proc Natl Acad Sci U S A. 2010;107(1):407–12. https://doi.org/10.1073/pnas.0902006107.
Johnson K, Levine K, Sergi J, Chamoun J, Roach R, Vekich J, Favis M, Horn M, Cao X, Miller B, Snyder W, Aivazian D, Reagan W, Berryman E, Colangelo J, Markiewicz V, Bagi CM, Brown TP, Coyle A, et al. Therapeutic effects of FGF23 c-tail Fc in a murine preclinical model of X-linked hypophosphatemia via the selective modulation of phosphate reabsorption. J Bone Miner Res. 2017;32:2062–73. https://doi.org/10.1002/jbmr.3197.
Wöhrle S, Henninger C, Bonny O, Thuery A, Beluch N, Hynes NE, Guagnano V, Sellers WR, Hofmann F, Kneissel M, Graus Porta D. Pharmacological inhibition of fibroblast growth factor (FGF) receptor signaling ameliorates FGF23-mediated hypophosphatemic rickets. J Bone Miner Res. 2013;28(4):899–911. https://doi.org/10.1002/jbmr.1810.
Zhang MY, Ranch D, Pereira RC, Armbrecht HJ, Portale AA, Perwad F. Chronic inhibition of ERK1/2 signaling improves disordered bone and mineral metabolism in hypophosphatemic (Hyp) mice. Endocrinology. 2012;153(4):1806–16. https://doi.org/10.1210/en.2011-1831.
Aono Y, Yamazaki Y, Yasutake J, Kawata T, Hasegawa H, Urakawa I, Fujita T, Wada M, Yamashita T, Fukumoto S, Shimada T. Therapeutic effects of anti-FGF23 antibodies in hypophosphatemic rickets/osteomalacia. J Bone Miner Res. 2009;24(11):1879–88. https://doi.org/10.1359/jbmr.090509.
Carpenter TO, Imel EA, Ruppe MD, Weber TJ, Klausner MA, Wooddell MM, et al. Randomized trial of the anti-FGF23 antibody KRN23 in X-linked hypophosphatemia. J Clin Invest. 2014;124(4):1587–97. https://doi.org/10.1172/jci72829.
Imel EA, Zhang X, Ruppe MD, Weber TJ, Klausner MA, Ito T, Vergeire M, Humphrey JS, Glorieux FH, Portale AA, Insogna K, Peacock M, Carpenter TO. Prolonged correction of serum phosphorus in adults with X-linked hypophosphatemia using monthly doses of KRN23. J Clin Endocrinol Metab. 2015;100(7):2565–73. https://doi.org/10.1210/jc.2015-1551.
Carpenter TO, Whyte MP, Imel EA, Boot AM, Hogler W, Linglart A, et al. Burosumab therapy in children with X-linked hypophosphatemia. N Engl J Med. 2018;378(21):1987–98. https://doi.org/10.1056/NEJMoa1714641. Phase 2 and 3 clinical trials of burosumab in child patients with XLH. These studies established the safety and efficacy of burosumab in child patients.
Whyte MP, Carpenter TO, Gottesman GS, Mao M, Skrinar A, San Martin J, et al. Efficacy and safety of burosumab in children aged 1-4 years with X-linked hypophosphataemia: a multicentre, open-label, phase 2 trial. Lancet Diabetes Endocrinol. 2019;7(3):189–99. https://doi.org/10.1016/s2213-8587(18)30338-3. Phase 2 and 3 clinical trials of burosumab in child patients with XLH. These studies established the safety and efficacy of burosumab in child patients.
Imel EA, Glorieux FH, Whyte MP, Munns CF, Ward LM, Nilsson O, Simmons JH, Padidela R, Namba N, Cheong HI, Pitukcheewanont P, Sochett E, Högler W, Muroya K, Tanaka H, Gottesman GS, Biggin A, Perwad F, Mao M, et al. Burosumab versus conventional therapy in children with X-linked hypophosphataemia: a randomised, active-controlled, open-label, phase 3 trial. Lancet. 2019;393(10189):2416–27. https://doi.org/10.1016/s0140-6736(19)30654-3. Phase 2 and 3 clinical trials of burosumab in child patients with XLH. These studies established the safety and efficacy of burosumab in child patients.
Insogna KL, Briot K, Imel EA, Kamenicky P, Ruppe MD, Portale AA, et al. A Randomized, double-blind, placebo-controlled, phase 3 trial evaluating the efficacy of burosumab, an anti-FGF23 antibody, in adults with X-linked hypophosphatemia: week 24 primary analysis. J Bone Miner Res. 2018;33(8):1383–93. https://doi.org/10.1002/jbmr.3475. Phase 2 and 3 clinical trials of burosumab in adult patients with XLH and TIO.
Portale AA, Carpenter TO, Brandi ML, Briot K, Cheong HI, Cohen-Solal M, et al. Continued beneficial effects of burosumab in adults with X-linked hypophosphatemia: results from a 24-week treatment continuation period after a 24-week double-blind placebo-controlled period. Calcif Tissue Int. 2019;105(3):271–84. https://doi.org/10.1007/s00223-019-00568-3.
Insogna KL, Rauch F, Kamenicky P, Ito N, Kubota T, Nakamura A, et al. Burosumab improved histomorphometric measures of osteomalacia in adults with X-linked hypophosphatemia: a phase 3, single-arm, international trial. J Bone Miner Res. 2019;34(12):2183–91. https://doi.org/10.1002/jbmr.3843.
Imanishi Y, Ito N, Rhee Y, Takeuchi Y, Shin CS, Takahashi Y, Onuma H, Kojima M, Kanematsu M, Kanda H, Seino Y, Fukumoto S. Interim analysis of a phase 2 open-label trial assessing burosumab efficacy and safety in patients with tumor-induced osteomalacia. J Bone Miner Res. 2021;36(2):262–70. https://doi.org/10.1002/jbmr.4184. Phase 2 and 3 clinical trials of burosumab in adult patients with XLH and TIO.
Jan de Beur SM, Miller PD, Weber TJ, Peacock M, Insogna K, Kumar R, Rauch F, Luca D, Cimms T, Roberts MS, San Martin J, Carpenter TO. Burosumab for the treatment of tumor-induced osteomalacia. J Bone Miner Res. 2021;36(4):627–35. https://doi.org/10.1002/jbmr.4233. Phase 2 and 3 clinical trials of burosumab in adult patients with XLH and TIO.
Amarnani R, Travis S, Javaid MK. Novel use of burosumab in refractory iron-induced FGF23-mediated hypophosphataemic osteomalacia. Rheumatology (Oxford). 2020;59(8):2166–8. https://doi.org/10.1093/rheumatology/kez627.
Gladding A, Szymczuk V, Auble BA, Boyce AM. Burosumab treatment for fibrous dysplasia. Bone. 2021;150:116004. https://doi.org/10.1016/j.bone.2021.116004.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
Funding
This work was supported in part by Grant-in-Aid for Young Scientists 18K15980 (JSPS) (to Y.T.) and Grant-in-Aid for Scientific Research 19H03676 (to S.F.) both from the Japan Society for the Promotion of Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Conflict of Interest
Department of Molecular Endocrinology in Tokushima University is supported by Kyyowa Kirin Co., Ltd.
Consent to Participate and Consent for Publication
All authors read the manuscript and agreed for publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Epidemiology and Pathophysiology
Rights and permissions
About this article
Cite this article
Takashi, Y., Kawanami, D. & Fukumoto, S. FGF23 and Hypophosphatemic Rickets/Osteomalacia. Curr Osteoporos Rep 19, 669–675 (2021). https://doi.org/10.1007/s11914-021-00709-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-021-00709-4