Abstract
Purpose of the Review
Osteocytes are cells embedded within the bone matrix, but their function and specific patterns of gene expression remain only partially defined; this is beginning to change with recent studies using transcriptomics. This unbiased approach can generate large amounts of data and is now being used to identify novel genes and signalling pathways within osteocytes both at baseline conditions and in response to stimuli. This review outlines the methods used to isolate cell populations containing osteocytes, and key recent transcriptomic studies that used osteocyte-containing preparations from bone tissue.
Recent Findings
Three common methods are used to prepare samples to examine osteocyte gene expression: digestion followed by sorting, laser capture microscopy, and the isolation of cortical bone shafts. All these methods present challenges in interpreting the data generated. Genes previously not known to be expressed by osteocytes have been identified and variations in osteocyte gene expression have been reported with age, sex, anatomical location, mechanical loading, and defects in bone strength.
Summary
A substantial proportion of newly identified transcripts in osteocytes remain functionally undefined but several have been cross-referenced with functional data. Future work and improved methods (e.g. scRNAseq) likely provide useful resources for the study of osteocytes and important new information on the identity and functions of this unique cell type within the skeleton.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Schaffler MB, Cheung WY, Majeska R, Kennedy O. Osteocytes: master orchestrators of bone. Calcif Tissue Int. 2014;94(1):5–24. https://doi.org/10.1007/s00223-013-9790-y.
Dallas SL, Prideaux M, Bonewald LF. The osteocyte: an endocrine cell ... and more. Endocr Rev. 2013;34(5):658–90. https://doi.org/10.1210/er.2012-1026.
Robling AG, Bonewald LF. The osteocyte: new insights. Annu Rev Physiol. 2020;82:485–506. https://doi.org/10.1146/annurev-physiol-021119-034332.
Palumbo C, Palazzini S, Marotti G. Morphological study of intercellular junctions during osteocyte differentiation. Bone. 1990;11(6):401–6. https://doi.org/10.1016/8756-3282(90)90134-K.
Bonewald LF. Generation and function of osteocyte dendritic processes. J Musculoskelet Neuronal Interact. 2005;5(4):321–4.
Buenzli PR, Sims NA. Quantifying the osteocyte network in the human skeleton. Bone. 2015;75:144–50. https://doi.org/10.1016/j.bone.2015.02.016.
Tresguerres FGF, Torres J, López-Quiles J, Hernández G, Vega JA, Tresguerres IF. The osteocyte: a multifunctional cell within the bone. Ann Anat - Anatomischer Anzeiger. 2020;227:151422. https://doi.org/10.1016/j.aanat.2019.151422.
Creecy A, Damrath JG, Wallace JM. Control of bone matrix properties by osteocytes. Front Endocrinol. 2021;11(1061) https://doi.org/10.3389/fendo.2020.578477.
Feng JQ, Ward LM, Liu S, Lu Y, Xie Y, Yuan B, Yu X, Rauch F, Davis SI, Zhang S, Rios H, Drezner MK, Quarles LD, Bonewald LF, White KE. Loss of DMP1 causes rickets and osteomalacia and identifies a role for osteocytes in mineral metabolism. Nat Genet. 2006;38(11):1310–5. https://doi.org/10.1038/ng1905.
Bonewald LF, Wacker MJ. FGF23 production by osteocytes. Pediatr Nephrol. 2013;28(4):563–8. https://doi.org/10.1007/s00467-012-2309-3.
Paic F, Igwe JC, Nori R, Kronenberg MS, Franceschetti T, Harrington P, Kuo L, Shin DG, Rowe DW, Harris SE, Kalajzic I. Identification of differentially expressed genes between osteoblasts and osteocytes. Bone. 2009;45(4):682–92. https://doi.org/10.1016/j.bone.2009.06.010.
Pellegata NS, Dieguez-Lucena JL, Joensuu T, Lau S, Montgomery KT, Krahe R, Kivelä T, Kucherlapati R, Forsius H, de la Chapelle A. Mutations in KERA, encoding keratocan, cause cornea plana. Nat Genet. 2000;25(1):91–5. https://doi.org/10.1038/75664.
Igwe JC, Gao Q, Kizivat T, Kao WW, Kalajzic I. Keratocan is expressed by osteoblasts and can modulate osteogenic differentiation. Connect Tissue Res. 2011;52(5):401–7. https://doi.org/10.3109/03008207.2010.546536.
Igwe JC, Jiang X, Paic F, Ma L, Adams DJ, Baldock PA, Pilbeam CC, Kalajzic I. Neuropeptide Y is expressed by osteocytes and can inhibit osteoblastic activity. J Cell Biochem. 2009;108(3):621–30. https://doi.org/10.1002/jcb.22294.
Matic I, Matthews BG, Kizivat T, Igwe JC, Marijanovic I, Ruohonen ST, Savontaus E, Adams DJ, Kalajzic I. Bone-specific overexpression of NPY modulates osteogenesis. J Musculoskelet Neuronal Interact. 2012;12(4):209–18.
Wee NKY, Vrhovac Madunic I, Ivanisevic T, Sinder BP, Kalajzic I. Divergent effects of peripheral and global neuropeptide Y deletion. J Musculoskelet Neuronal Interact. 2020;20(4):579–90.
Chia LY, Walsh NC, Martin TJ, Sims NA. Isolation and gene expression of haematopoietic-cell-free preparations of highly purified murine osteocytes. Bone. 2015;72:34–42. https://doi.org/10.1016/j.bone.2014.11.005.
Ochiai-Shino H, Kato H, Sawada T, Onodera S, Saito A, Takato T, Shibahara T, Muramatsu T, Azuma T. A novel strategy for enrichment and isolation of osteoprogenitor cells from induced pluripotent stem cells based on surface marker combination. PLoS One. 2014;9(6):e99534. https://doi.org/10.1371/journal.pone.0099534.
Zimmerman SM, Dimori M, Heard-Lipsmeyer ME, Morello R. The osteocyte transcriptome is extensively dysregulated in mouse models of osteogenesis imperfecta. JBMR Plus. 2019;3(7):e10171. https://doi.org/10.1002/jbm4.10171.
Greenblatt MB, Ono N, Ayturk UM, Debnath S, Lalani S. The unmixing problem: a guide to applying single-cell RNA sequencing to bone. J Bone Miner Res. 2019;34(7):1207–19. https://doi.org/10.1002/jbmr.3802. This paper provides an overview and practical considerations for performing single-cell sequencing analysis in bone
Machado L. Esteves de Lima J, Fabre O, Proux C, Legendre R, Szegedi A et al. <em>In situ</em> fixation redefines quiescence and early activation of skeletal muscle stem cells. Cell Rep. 2017;21(7):1982–93. https://doi.org/10.1016/j.celrep.2017.10.080.
Ayturk UM, Jacobsen CM, Christodoulou DC, Gorham J, Seidman JG, Seidman CE, Robling AG, Warman ML. An RNA-seq protocol to identify mRNA expression changes in mouse diaphyseal bone: applications in mice with bone property altering Lrp5 mutations. J Bone Miner Res. 2013;28(10):2081–93. https://doi.org/10.1002/jbmr.1946.
O’Flanagan CH, Campbell KR, Zhang AW, Kabeer F, Lim JLP, Biele J, et al. Dissociation of solid tumor tissues with cold active protease for single-cell RNA-seq minimizes conserved collagenase-associated stress responses. Genome Biol. 2019;20(1):210. https://doi.org/10.1186/s13059-019-1830-0. This paper demonstrates the impact of collagenase digestion on the transcriptome in single-cell RNA sequencing studies
Stern AR, Stern MM, Van Dyke ME, Jähn K, Prideaux M, Bonewald LF. Isolation and culture of primary osteocytes from the long bones of skeletally mature and aged mice. Biotechniques. 2012;52(6):361–73. https://doi.org/10.2144/0000113876.
Nioi P, Taylor S, Hu R, Pacheco E, He YD, Hamadeh H, Paszty C, Pyrah I, Ominsky MS, Boyce RW. Transcriptional profiling of laser capture microdissected subpopulations of the osteoblast lineage provides insight into the early response to sclerostin antibody in rats. J Bone Miner Res. 2015;30(8):1457–67. https://doi.org/10.1002/jbmr.2482.
Harris TL, Silva MJ. Gene expression of intracortical bone demonstrates loading-induced increases in Wnt1 and Ngf and inhibition of bone remodeling processes. Bone. 2021;150:116019. https://doi.org/10.1016/j.bone.2021.116019.
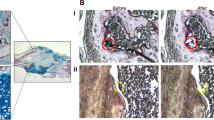
Vrahnas C, Blank M, Dite TA, Tatarczuch L, Ansari N, Crimeen-Irwin B, Nguyen H, Forwood MR, Hu Y, Ikegame M, Bambery KR, Petibois C, Mackie EJ, Tobin MJ, Smyth GK, Oakhill JS, Martin TJ, Sims NA. Increased autophagy in EphrinB2-deficient osteocytes is associated with elevated secondary mineralization and brittle bone. Nat Commun. 2019;10(1):3436. https://doi.org/10.1038/s41467-019-11373-9.
Youlten SE, Kemp JP, Logan JG, Ghirardello EJ, Sergio CM, Dack MRG, Guilfoyle SE, Leitch VD, Butterfield NC, Komla-Ebri D, Chai RC, Corr AP, Smith JT, Mohanty ST, Morris JA, McDonald MM, Quinn JMW, McGlade AR, Bartonicek N, et al. Osteocyte transcriptome mapping identifies a molecular landscape controlling skeletal homeostasis and susceptibility to skeletal disease. Nat Commun. 2021;12(1):2444. https://doi.org/10.1038/s41467-021-22517-1. This study examines how skeletal sites, age, and sex influence transcript expression in cortical bone osteocytes under physiological conditions.
Root SH, Wee NKY, Novak S, Rosen CJ, Baron R, Matthews BG, Kalajzic I. Perivascular osteoprogenitors are associated with transcortical channels of long bones. Stem Cells. 2020;38(6):769–81. https://doi.org/10.1002/stem.3159.
Grüneboom A, Hawwari I, Weidner D, Culemann S, Müller S, Henneberg S, Brenzel A, Merz S, Bornemann L, Zec K, Wuelling M, Kling L, Hasenberg M, Voortmann S, Lang S, Baum W, Ohs A, Kraff O, Quick HH, et al. A network of trans-cortical capillaries as mainstay for blood circulation in long bones. Nat Metab. 2019;1(2):236–50. https://doi.org/10.1038/s42255-018-0016-5.
Kelly NH, Schimenti JC, Ross FP, van der Meulen MCH. Transcriptional profiling of cortical versus cancellous bone from mechanically-loaded murine tibiae reveals differential gene expression. Bone. 2016;86:22–9. https://doi.org/10.1016/j.bone.2016.02.007.
Al-Barghouthi BM, Mesner LD, Calabrese GM, Brooks D, Tommasini SM, Bouxsein ML, et al. Systems genetics in diversity outbred mice inform BMD GWAS and identify determinants of bone strength. Nat Commun. 2021;12(1):3408. https://doi.org/10.1038/s41467-021-23649-0. This study examines the transcriptomes of 196 cortical bone samples isolated from Diversity Outbred mice. Analysis of this data using a unique Bayesian network approach combined with human GWAS studies identified novel genes that may regulate bone mass
Taylor S, Ominsky MS, Hu R, Pacheco E, He YD, Brown DL, Aguirre JI, Wronski TJ, Buntich S, Afshari CA, Pyrah I, Nioi P, Boyce RW. Time-dependent cellular and transcriptional changes in the osteoblast lineage associated with sclerostin antibody treatment in ovariectomized rats. Bone. 2016;84:148–59. https://doi.org/10.1016/j.bone.2015.12.013.
Achiou Z, Toumi H, Touvier J, Boudenot A, Uzbekov R, Ominsky MS, Pallu S, Lespessailles E. Sclerostin antibody and interval treadmill training effects in a rodent model of glucocorticoid-induced osteopenia. Bone. 2015;81:691–701. https://doi.org/10.1016/j.bone.2015.09.010.
Mosey H, Nunez JA, Goring A, Clarkin CE, Staines KA, Lee PD, et al. Sost deficiency does not alter bone’s lacunar or vascular porosity in mice. Front Mater. 2017;4:27. https://doi.org/10.3389/fmats.2017.00027.
Yamamoto T, Hasegawa T, Sasaki M, Hongo H, Tabata C, Liu Z, Li M, Amizuka N. Structure and formation of the twisted plywood pattern of collagen fibrils in rat lamellar bone. J Electron Microsc. 2012;61(2):113–21. https://doi.org/10.1093/jmicro/dfs033.
Sims NA, White CP, Sunn KL, Thomas GP, Drummond ML, Morrison NA, Eisman JA, Gardiner EM. Human and murine osteocalcin gene expression: conserved tissue restricted expression and divergent responses to 1,25-dihydroxyvitamin D3 in vivo. Mol Endocrinol. 1997;11(11):1695–708. https://doi.org/10.1210/mend.11.11.0008.
Kartsogiannis V, Zhou H, Horwood NJ, Thomas RJ, Hards DK, Quinn JM, et al. Localization of RANKL (receptor activator of NF kappa B ligand) mRNA and protein in skeletal and extraskeletal tissues. Bone. 1999;25(5):525–34. https://doi.org/10.1016/s8756-3282(99)00214-8.
Kartsogiannis V, Udagawa N, Ng KW, Martin TJ, Moseley JM, Zhou H. Localization of parathyroid hormone-related protein in osteoclasts by in situ hybridization and immunohistochemistry. Bone. 1998;22(3):189–94. https://doi.org/10.1016/s8756-3282(97)00278-0.
van Bezooijen RL, Roelen BAJ, Visser A, van der Wee-Pals L, de Wilt E, Karperien M, Hamersma H, Papapoulos SE, ten Dijke P, Löwik CWGM. Sclerostin is an osteocyte-expressed negative regulator of bone formation, but not a classical BMP antagonist. J Exp Med. 2004;199(6):805–14. https://doi.org/10.1084/jem.20031454.
Isojima T, Sims NA. Cortical bone development, maintenance and porosity: genetic alterations in humans and mice influencing chondrocytes, osteoclasts, osteoblasts and osteocytes. Cell Mol Life Sci. 2021;78:5755–73. https://doi.org/10.1007/s00018-021-03884-w.
Qing H, Ardeshirpour L, Pajevic PD, Dusevich V, Jähn K, Kato S, et al. Demonstration of osteocytic perilacunar/canalicular remodeling in mice during lactation. J Bone Miner Res. 2012;27(5):1018–29. https://doi.org/10.1002/jbmr.1567.
Wang N, Niger C, Li N, Richards GO, Skerry TM. Cross-Species RNA-Seq Study Comparing Transcriptomes of Enriched Osteocyte Populations in the Tibia and Skull. Front Endocrinol. 2020;11(693) https://doi.org/10.3389/fendo.2020.581002. This cross-species study compares the transcriptomic signature of tibia and calvaria isolated from rat, mouse and macaque. They identified 32 differentially expressed genes between calvaria and tibia that were present across the 3 species
Rux DR, Wellik DM. Hox genes in the adult skeleton: novel functions beyond embryonic development. Dev Dyn. 2017;246(4):310–7. https://doi.org/10.1002/dvdy.24482.
Himeno-Ando A, Izumi Y, Yamaguchi A, Iimura T. Structural differences in the osteocyte network between the calvaria and long bone revealed by three-dimensional fluorescence morphometry, possibly reflecting distinct mechano-adaptations and sensitivities. Biochem Biophys Res Commun. 2012;417(2):765–70. https://doi.org/10.1016/j.bbrc.2011.12.031.
Agarwal P, Wylie JN, Galceran J, Arkhitko O, Li C, Deng C, Grosschedl R, Bruneau BG. Tbx5 is essential for forelimb bud initiation following patterning of the limb field in the mouse embryo. Development. 2003;130(3):623–33. https://doi.org/10.1242/dev.00191.
DeLaurier A, Schweitzer R, Logan M. Pitx1 determines the morphology of muscle, tendon, and bones of the hindlimb. Dev Biol. 2006;299(1):22–34. https://doi.org/10.1016/j.ydbio.2006.06.055.
Mallo M, Wellik DM, Deschamps J. Hox genes and regional patterning of the vertebrate body plan. Dev Biol. 2010;344(1):7–15. https://doi.org/10.1016/j.ydbio.2010.04.024.
Baldock PA, Lee NJ, Driessler F, Lin S, Allison S, Stehrer B, Lin EJD, Zhang L, Enriquez RF, Wong IPL, McDonald MM, During M, Pierroz DD, Slack K, Shi YC, Yulyaningsih E, Aljanova A, Little DG, Ferrari SL, et al. Neuropeptide Y knockout mice reveal a central role of NPY in the coordination of bone mass to body weight. PLoS One. 2009;4(12):e8415. https://doi.org/10.1371/journal.pone.0008415.
Wee NKY, Sinder BP, Novak S, Wang X, Stoddard C, Matthews BG, Kalajzic I. Skeletal phenotype of the neuropeptide Y knockout mouse. Neuropeptides. 2019;73:78–88. https://doi.org/10.1016/j.npep.2018.11.009.
Janssen BJ, Malinauskas T, Weir GA, Cader MZ, Siebold C, Jones EY. Neuropilins lock secreted semaphorins onto plexins in a ternary signaling complex. Nat Struct Mol Biol. 2012;19(12):1293–9. https://doi.org/10.1038/nsmb.2416.
Hayashi M, Nakashima T, Taniguchi M, Kodama T, Kumanogoh A, Takayanagi H. Osteoprotection by semaphorin 3A. Nature. 2012;485(7396):69–74. https://doi.org/10.1038/nature11000.
Fukuda T, Takeda S, Xu R, Ochi H, Sunamura S, Sato T, Shibata S, Yoshida Y, Gu Z, Kimura A, Ma C, Xu C, Bando W, Fujita K, Shinomiya K, Hirai T, Asou Y, Enomoto M, Okano H, et al. Sema3A regulates bone-mass accrual through sensory innervations. Nature. 2013;497(7450):490–3. https://doi.org/10.1038/nature12115.
Hayashi M, Nakashima T, Yoshimura N, Okamoto K, Tanaka S, Takayanagi H. Autoregulation of osteocyte Sema3A orchestrates estrogen action and counteracts bone aging. Cell Metab. 2019;29(3):627–37.e5. https://doi.org/10.1016/j.cmet.2018.12.021.
Blank M, Sims NA. Cellular processes by which osteoblasts and osteocytes control bone mineral deposition and maturation revealed by stage-specific EphrinB2 knockdown. Curr Osteoporos Rep. 2019;17(5):270–80. https://doi.org/10.1007/s11914-019-00524-y.
Nguyen M, Wong YC, Ysselstein D, Severino A, Krainc D. Synaptic, mitochondrial, and lysosomal dysfunction in Parkinson’s disease. Trends Neurosci. 2019;42(2):140–9. https://doi.org/10.1016/j.tins.2018.11.001.
Moujalled D, Strasser A, Liddell JR. Molecular mechanisms of cell death in neurological diseases. Cell Death Differ. 2021;28(7):2029–44. https://doi.org/10.1038/s41418-021-00814-y.
Mantila Roosa SM, Liu Y, Turner CH. Gene expression patterns in bone following mechanical loading. J Bone Miner Res. 2011;26(1):100–12. https://doi.org/10.1002/jbmr.193.
Tomlinson RE, Li Z, Li Z, Minichiello L, Riddle RC, Venkatesan A, Clemens TL. NGF-TrkA signaling in sensory nerves is required for skeletal adaptation to mechanical loads in mice. Proc Natl Acad Sci. 2017;114(18):E3632–E41. https://doi.org/10.1073/pnas.1701054114.
Robinson JA, Chatterjee-Kishore M, Yaworsky PJ, Cullen DM, Zhao W, Li C, Kharode Y, Sauter L, Babij P, Brown EL, Hill AA, Akhter MP, Johnson ML, Recker RR, Komm BS, Bex FJ. Wnt/beta-catenin signaling is a normal physiological response to mechanical loading in bone. J Biol Chem. 2006;281(42):31720–8. https://doi.org/10.1074/jbc.M602308200.
Galea GL, Meakin LB, Harris MA, Delisser PJ, Lanyon LE, Harris SE, Price JS. Old age and the associated impairment of bones’ adaptation to loading are associated with transcriptomic changes in cellular metabolism, cell-matrix interactions and the cell cycle. Gene. 2017;599:36–52. https://doi.org/10.1016/j.gene.2016.11.006.
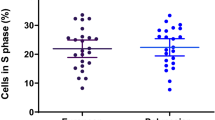
Chermside-Scabbo CJ, Harris TL, Brodt MD, Braenne I, Zhang B, Farber CR, Silva MJ. Old mice have less transcriptional activation but similar periosteal cell proliferation compared to young-adult mice in response to in vivo mechanical loading. J Bone Miner Res. 2020;35(9):1751–64. https://doi.org/10.1002/jbmr.4031.
Balemans W, Patel N, Ebeling M, Van Hul E, Wuyts W, Lacza C, et al. Identification of a 52 kb deletion downstream of the SOST gene in patients with van Buchem disease. J Med Genet. 2002;39(2):91–7. https://doi.org/10.1136/jmg.39.2.91.
Staehling-Hampton K, Proll S, Paeper BW, Zhao L, Charmley P, Brown A, Gardner JC, Galas D, Schatzman RC, Beighton P, Papapoulos S, Hamersma H, Brunkow ME. A 52-kb deletion in the SOST-MEOX1 intergenic region on 17q12-q21 is associated with van Buchem disease in the Dutch population. Am J Med Genet. 2002;110(2):144–52. https://doi.org/10.1002/ajmg.10401.
Brunkow ME, Gardner JC, Van Ness J, Paeper BW, Kovacevich BR, Proll S, et al. Bone dysplasia sclerosteosis results from loss of the SOST gene product, a novel cystine knot-containing protein. Am J Hum Genet. 2001;68(3):577–89. https://doi.org/10.1086/318811.
Balemans W, Ebeling M, Patel N, Van Hul E, Olson P, Dioszegi M, et al. Increased bone density in sclerosteosis is due to the deficiency of a novel secreted protein (SOST). Hum Mol Genet. 2001;10(5):537–43. https://doi.org/10.1093/hmg/10.5.537.
A gene (PEX) with homologies to endopeptidases is mutated in patients with X-linked hypophosphatemic rickets. The HYP Consortium. Nat Genet. 1995;11(2):130–6. https://doi.org/10.1038/ng1095-130.
Keupp K, Beleggia F, Kayserili H, Barnes AM, Steiner M, Semler O, Fischer B, Yigit G, Janda CY, Becker J, Breer S, Altunoglu U, Grünhagen J, Krawitz P, Hecht J, Schinke T, Makareeva E, Lausch E, Cankaya T, et al. Mutations in WNT1 cause different forms of bone fragility. Am J Hum Genet. 2013;92(4):565–74. https://doi.org/10.1016/j.ajhg.2013.02.010.
Pyott SM, Tran TT, Leistritz DF, Pepin MG, Mendelsohn NJ, Temme RT, Fernandez BA, Elsayed SM, Elsobky E, Verma I, Nair S, Turner EH, Smith JD, Jarvik GP, Byers PH. WNT1 mutations in families affected by moderately severe and progressive recessive osteogenesis imperfecta. Am J Hum Genet. 2013;92(4):590–7. https://doi.org/10.1016/j.ajhg.2013.02.009.
Fahiminiya S, Majewski J, Mort J, Moffatt P, Glorieux FH, Rauch F. Mutations in WNT1 are a cause of osteogenesis imperfecta. J Med Genet. 2013;50(5):345–8. https://doi.org/10.1136/jmedgenet-2013-101567.
Jovanovic M, Guterman-Ram G, Marini JC. Osteogenesis imperfecta: mechanisms and signaling pathways connecting classical and rare OI types. Endocr Rev. 2021; https://doi.org/10.1210/endrev/bnab017.
Moffatt P, Boraschi-Diaz I, Marulanda J, Bardai G, Rauch F. Calvaria Bone Transcriptome in mouse models of osteogenesis imperfecta. Int J Mol Sci. 2021;22(10):5290. https://doi.org/10.3390/ijms22105290.
MacLeod RS, Cawley KM, Gubrij I, Nookaew I, Onal M, O'Brien CA. Effective CRISPR interference of an endogenous gene via a single transgene in mice. Sci Rep. 2019;9(1):17312. https://doi.org/10.1038/s41598-019-53611-6.
Elefteriou F, Couasnay G. Advantages and limitations of Cre mouse lines used in skeletal research. Methods Mol Biol. 2021;2230:39–59. https://doi.org/10.1007/978-1-0716-1028-2_3.
Roeder E, Matthews BG, Kalajzic I. Visual reporters for study of the osteoblast lineage. Bone. 2016;92:189–95. https://doi.org/10.1016/j.bone.2016.09.004.
Dallas SL, Xie Y, Shiflett LA, Ueki Y. Mouse Cre models for the study of bone diseases. Curr Osteoporos Rep. 2018;16(4):466–77. https://doi.org/10.1007/s11914-018-0455-7.
Matic I, Matthews BG, Wang X, Dyment NA, Worthley DL, Rowe DW, Grcevic D, Kalajzic I. Quiescent bone lining cells are a major source of osteoblasts during adulthood. Stem Cells. 2016;34(12):2930–42. https://doi.org/10.1002/stem.2474.
Zhang J, Link DC. Targeting of mesenchymal stromal cells by Cre-recombinase transgenes commonly used to target osteoblast lineage cells. J Bone Miner Res. 2016;31(11):2001–7. https://doi.org/10.1002/jbmr.2877.
Ansari N, Isojima T, Crimeen-Irwin B, Poulton IJ, McGregor NE, Ho PWM, et al. Dmp1Cre-directed knockdown of parathyroid hormone-related protein (PTHrP) in murine decidua is associated with a life-long increase in bone mass, width, and strength in male progeny. J Bone Miner Res. 2021; https://doi.org/10.1002/jbmr.4388.
Ståhl PL, Salmén F, Vickovic S, Lundmark A, Navarro JF, Magnusson J, Giacomello S, Asp M, Westholm JO, Huss M, Mollbrink A, Linnarsson S, Codeluppi S, Borg Å, Pontén F, Costea PI, Sahlén P, Mulder J, Bergmann O, et al. Visualization and analysis of gene expression in tissue sections by spatial transcriptomics. Science. 2016;353(6294):78–82. https://doi.org/10.1126/science.aaf2403.
Debnath S, Yallowitz AR, McCormick J, Lalani S, Zhang T, Xu R, Li N, Liu Y, Yang YS, Eiseman M, Shim JH, Hameed M, Healey JH, Bostrom MP, Landau DA, Greenblatt MB. Discovery of a periosteal stem cell mediating intramembranous bone formation. Nature. 2018;562(7725):133–9. https://doi.org/10.1038/s41586-018-0554-8.
Zhong L, Yao L, Tower RJ, Wei Y, Miao Z, Park J, Shrestha R, Wang L, Yu W, Holdreith N, Huang X, Zhang Y, Tong W, Gong Y, Ahn J, Susztak K, Dyment N, Li M, Long F, et al. Single cell transcriptomics identifies a unique adipose lineage cell population that regulates bone marrow environment. elife. 2020;9 https://doi.org/10.7554/eLife.54695.
Matsushita Y, Nagata M, Kozloff KM, Welch JD, Mizuhashi K, Tokavanich N, Hallett SA, Link DC, Nagasawa T, Ono W, Ono N. A Wnt-mediated transformation of the bone marrow stromal cell identity orchestrates skeletal regeneration. Nat Commun. 2020;11(1):332. https://doi.org/10.1038/s41467-019-14029-w.
Baryawno N, Przybylski D, Kowalczyk MS, Kfoury Y, Severe N, Gustafsson K, et al. A cellular taxonomy of the bone marrow stroma in homeostasis and leukemia. Cell. 2019;177(7):1915–32.e16. https://doi.org/10.1016/j.cell.2019.04.040.
Pathak JL, Bravenboer N, Klein-Nulend J. The osteocyte as the new discovery of therapeutic options in rare bone diseases. Front Endocrinol (Lausanne). 2020;11:405. https://doi.org/10.3389/fendo.2020.00405.
Availability of Data and Material
N/A
Code Availability
N/A
Funding
NKW is supported by an EH Flack Fellowship provided by the Marion and EH Flack Trust and a Rising Star Award provided by St Vincent’s Institute of Medical Research, Melbourne. NAS is supported by an NHMRC (Australia) Senior Research Fellowship. RM is supported by NIH funds from NIGMS (P20 GM125503).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Osteocytes
Rights and permissions
About this article
Cite this article
Wee, N.K., Sims, N.A. & Morello, R. The Osteocyte Transcriptome: Discovering Messages Buried Within Bone. Curr Osteoporos Rep 19, 604–615 (2021). https://doi.org/10.1007/s11914-021-00708-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-021-00708-5