Abstract
Purpose of Review
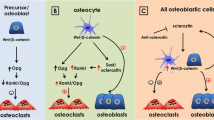
Diabetes mellitus is a prevalent chronic disease affecting millions of people in the world. Bone fragility is a complication found in diabetic patients. Although osteoblasts and osteoclasts are directly affected by diabetes, herein we focus on how the diabetic state—based on hyperglycemia and accumulation of advanced glycation end products among other features—impairs osteocyte functions exerting deleterious effects on bone.
Recent Findings
In the last years, several studies described that diabetic conditions cause morphological modifications on lacunar-canalicular system, alterations on osteocyte mechanoreceptors and intracellular pathways and on osteocyte communication with other cells through the secretion of proteins such as sclerostin or RANKL.
Summary
This article gives an overview of events occurring in diabetic osteocytes. In particular, mechanical responses seem to be seriously affected in these conditions, suggesting that mechanical sensibility could be a target for future research in the field.
Similar content being viewed by others
References
Ferrari S, IOF Bone and Diabetes Working Group, Napoli N, Chandran M, Pierroz DD, Abrahamsen B, et al. Mechanisms of diabetes mellitus-induced bone fragility. Nat Rev Endocrinol. 2017;13:208–19.
Dobnig H, Hofbauer LC, Brueck CC, Singh SK. Osteoporosis in patients with diabetes mellitus. J Bone Miner Res. 2007;22:1317–28.
Cunha JS, Ferreira VM, Maquigussa E, Naves MA, Boim MA. Effects of high glucose and high insulin concentrations on osteoblast function in vitro. Cell Tissue Res. 2014;358(1):249–56. https://doi.org/10.1007/s00441-014-1913-x.
Botolin LR, McCabe S. Chronic hyperglycemia modulates osteoblast gene expression through osmotic and non-osmotic pathways. J Cell Biochem. 2006;99:411–24.
Yu L, An Y, Zhang H, Wang C, Jiao F, Xu H, et al. Activation of ROS/MAPKs/NF-κB/NLRP3 and inhibition of efferocytosis in osteoclast-mediated diabetic osteoporosis. FASEB J. 2019;33(11):12515–27.
Plotkin L, Bellido T. Osteocytic signalling pathways as therapeutic targets for bone fragility. Nat Rev Endocrinol. 2016;12(10):593–605.
Bonewald LF. The amazing osteocyte. J Bone Miner Res. 2011;26(2):229–38.
Sun T, et al. Effects of mechanical vibration on cell morphology, proliferation, apoptosis, and cytokine expression/secretion in osteocyte-like MLO-Y4 cells exposed to high glucose. Cell Biol Int. 2019;128(1):128:112056. https://doi.org/10.1002/cbin.11221.
Wang L, Lai X, Price C, Modla S, Thompson WR, Caplan J, et al. The dependences of osteocyte network on bone compartment, age, and disease. Bone Res. 2015;3:15009.
Chappard D, Mabilleau G, Perrot R, Flatt PR, Irwin N. High fat-fed diabetic mice present with profound alterations of the osteocyte network. Bone. 2006;90:99–106.
Jing D, Liu X, Li W, Cai J, Yan Z, Shao X, et al. Spatiotemporal characterization of microdamage accumulation and its targeted remodeling mechanisms in diabetic fatigued bone. FASEB J. 2020;34(2):2579–94.
Xin W, Rhodes DR, Ingold C, Chinnaiyan AM, Rubin MA. Dysregulation of the annexin family protein family is associated with prostate cancer progression. Am J Pathol. 2003;162(1):255–61. https://doi.org/10.1016/S0002-9440(10)63816-3.
Maycas M, Esbrit P, Gortázar ARAR. Molecular mechanisms in bone mechanotransduction. Histol Histopathol. 2017;32(8):751–60.
Plotkin LI. Connexin 43 hemichannels and intracellular signaling in bone cells. Front Physiol. 2014;5:131. https://doi.org/10.3389/fphys.2014.00131.
Xu H, Liu R, Ning D, Zhang J, Yang R, Riquelme MA, et al. Biological responses of osteocytic connexin 43 hemichannels to simulated microgravity. J Orthop Res. 2017;35(6):1195–202. https://doi.org/10.1002/jor.23224.
Genetos DC, Kephart CJ, Zhang Y, Yellowley CE, Donahue HJ. Oscillating fluid flow activation of gap junction hemichannels induces ATP release from MLO-Y4 osteocytes. J Cell Physiol. 2007;212(1):207–14. https://doi.org/10.1002/jcp.21021.
Xu H, Gu S, Riquelme MA, Burra S, Callaway D, Cheng H, et al. Connexin 43 channels are essential for normal bone structure and osteocyte viability. J Bone Miner Res. 2015;30(3):550–62. https://doi.org/10.1002/jbmr.2374.
Yang L, Zhou G, Li M, Li Y, Yang L, Fu Q, et al. High glucose downregulates connexin 43 expression and its gap junction and hemichannel function in osteocyte-like mlo-y4 cells through activation of the p38mapk/erk signal pathway. Diabetes, Metab Syndr Obes Targets Ther. 2020;13:545–57. https://doi.org/10.2147/DMSO.S239892.
Agrawal A, Gartland A. P2x7 receptors: role in bone cell formation and function. J Mol Endocrinol. 2015;54(2):R75–88. https://doi.org/10.1530/JME-14-0226.
Orriss IR, Burnstock G, Arnett TR. Purinergic signalling and bone remodelling. Curr Opin Pharmacol. 2010;10(3):322–30. https://doi.org/10.1016/j.coph.2010.01.003.
Jørgensen NR. The purinergic P2X7 ion channel receptor—a ‘repair’ receptor in bone. Curr Opin Immunol. 2018;52:32–8. https://doi.org/10.1016/j.coi.2018.03.016.
Seref-Ferlengez Z, Maung S, Schaffler MB, Spray DC, Suadicani SO, Thi MM. P2X7R-Panx1 complex impairs bone mechanosignaling under high glucose levels associated with type-1 diabetes. PLoS One. 2016;11:5. https://doi.org/10.1371/journal.pone.0155107.
Chachisvilis M, Zhang YL, Frangos JA. Mechanical stimulus alters conformation of type 1 parathyroid hormone receptor in bone cells. Am J Phys Cell Phys. 2009;296(6):C1391–9.
Maycas M, Ardura JA, de Castro LF, Bravo B, Gortázar AR, Esbrit P. Role of the parathyroid hormone type 1 receptor (PTH1R) as a mechanosensor in osteocyte survival. J Bone Miner Res. Jul. 2015;30(7):1231–44. https://doi.org/10.1002/jbmr.2439.
Ben-awadh AN, Delgado-Calle J, Tu X, Kuhlenschmidt K, Allen MR, Plotkin LI, et al. Parathyroid hormone receptor signaling induces bone resorption in the adult skeleton by directly regulating the RANKL gene in osteocytes. Endocrinology. 2014;155(8):2797–809. https://doi.org/10.1210/en.2014-1046.
Wein MN. Parathyroid hormone signaling in osteocytes. JBMR Plus. 2018;2(1):22–30. https://doi.org/10.1002/jbm4.10021.
Lozano D, de Castro LF, Dapía S, Andrade-Zapata I, Manzarbeitia F́, Alvarez-Arroyo MV, et al. Role of parathyroid hormone-related protein in the decreased osteoblast function in diabetes-related osteopenia. Endocrinology. 2009;150(5):2027–35. https://doi.org/10.1210/en.2008-1108.
Maycas M, McAndrews KA, Sato AY, Pellegrini GG, Brown DM, Allen MR, et al. PTHrP-derived peptides restore bone mass and strength in diabetic mice: additive effect of mechanical loading. J Bone Miner Res. Mar. 2017;32(3):486–97. https://doi.org/10.1002/jbmr.3007.
Esbrit P, Lozano D, Fernández-de-Castro L, Portal-Núñez S, López-Herradón A, Dapía S, et al. The C-terminal fragment of parathyroid hormone-related peptide promotes bone formation in diabetic mice with low-turnover osteopaenia. Br J Pharmacol. 2011;162(6):1424–38.
Esbrit P, García-Martín A, Acitores A, Maycas M, Villanueva-Peñacarrillo ML. Src kinases mediate VEGFR2 transactivation by the osteostatin domain of PTHrP to modulate osteoblastic function. J Cell Biochem. 2013;114(6):1404–13.
de Castro LF, Maycas M, Bravo B, Esbrit P, Gortazar A. VEGF receptor 2 (VEGFR2) activation is essential for osteocyte survival induced by mechanotransduction. J Cell Physiol. 2015;230(2):278–85. https://doi.org/10.1002/jcp.24734.
Schwartz M, Coon BG, Baeyens N, Han J, Budatha M, Ross TD, et al. Intramembrane binding of VE-cadherin to VEGFR2 and VEGFR3 assembles the endothelial mechanosensory complex. J Cell Biol. 2015;208(7):975–86.
Parajuli A, Liu C, Li W, Gu X, Lai X, Pei S, et al. Bone’s responses to mechanical loading are impaired in type 1 diabetes. Bone. 2015;81:152–60. https://doi.org/10.1016/j.bone.2015.07.012.
Bellido T, Aguirre JI, Plotkin LI, Stewart SA, Weinstein RS, Parfitt AM, et al. Osteocyte apoptosis is induced by weightlessness in mice and precedes osteoclast recruitment and bone loss. J Bone Miner Res. 2006;21(4):605–15.
Zhou Y, Zhang C, Wei W, Chi M, Wan Y, Li X, et al. FOXO1 mediates advanced glycation end products induced mouse osteocyte-like MLO-Y4 cell apoptosis and dysfunctions. J Diabetes Res. 2019;2019:6757428.
Maycas M, Portolés MT, Matesanz MC, Buendía I, Linares J, Feito MJ, et al. High glucose alters the secretome of mechanically stimulated osteocyte-like cells affecting osteoclast precursor recruitment and differentiation. J Cell Physiol. 2017;232(12):3611–21. https://doi.org/10.1002/jcp.25829.
Sánchez-de-Diego C, et al. Glucose restriction promotes osteocyte specification by activating a PGC-1α-dependent transcriptional program. iScience. 2019;15:79–94. https://doi.org/10.1016/j.isci.2019.04.015.
Riddle RC, Clemens TL. Bone cell bioenergetics and skeletal energy homeostasis. Physiol Rev. 2017;97(2):667–98. https://doi.org/10.1152/physrev.00022.2016.
Lira VA, Benton CR, Yan Z, Bonen A. PGC-1α regulation by exercise training and its influences on muscle function and insulin sensitivity. Am J Physiol Endocrinol Metab. 2010;299(2):E145–61. https://doi.org/10.1152/ajpendo.00755.2009.
Yang Y, Graves DT, Alshabab A, Albiero ML, Mattos M, Corrêa JD, et al. Osteocytes play an important role in experimental periodontitis in healthy and diabetic mice through expression of RANKL. J Clin Periodontol. 2018;45(3):285–92.
Karalazou P, et al. OPG/RANK/RANKL signaling axis in patients with type i diabetes: associations with parathormone and vitamin D. Ital J Pediatr. 2019;45(1):161.
Abe I, et al. Effect of denosumab, a human monoclonal antibody of receptor activator of nuclear factor kappa-B ligand (RANKL), upon glycemic and metabolic parameters: effect of denosumab on glycemic parameters. Med. 2019;98(47):e18067.
Cheung W-Y, Simmons CA, You L. Osteocyte apoptosis regulates osteoclast precursor adhesion via osteocytic IL-6 secretion and endothelial ICAM-1 expression. Bone. 2012;50:104–10.
Starzyk J, Wędrychowicz A, Sztefko K. Sclerostin and its significance for children and adolescents with type 1 diabetes mellitus (T1D). Bone. 2019;120:387–92.
Muñoz-Torres M, García-Martín A, Rozas-Moreno P, Reyes-García R, Morales-Santana S, García-Fontana B, et al. Circulating levels of sclerostin are increased in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab. 2012;97(1):234–41.
Gennari L, et al. Circulating sclerostin levels and bone turnover in type 1 and type 2 diabetes. J Clin Endocrinol Metab. 2012;97:3744–50.
Bonewald L, Pacicca DM, Brown T, Watkins D, Kover K, Yan Y, et al. Elevated glucose acts directly on osteocytes to increase sclerostin expression in diabetes. Sci Rep. 2019;9(1):17353.
Cipriani C, et al. The interplay between bone and glucose metabolism. Front Endocrinol (Lausanne). 2020;11:122.
Hesse M, Fröhlich LF, Zeitz U, Lanske B, Erben RG. Ablation of vitamin D signaling rescues bone, mineral, and glucose homeostasis in Fgf-23 deficient mice. Matrix Biol. 2007;26(2):75–84.
Farlay D, LAG A, Gineyts E, Akhter MP, Recker RR, Boivin G. Nonenzymatic glycation and degree of mineralization are higher in bone from fractured patients with type 1 diabetes mellitus. J Bone Miner Res. 2016;31:190–5.
Severcan F, Bozkurt O, Bilgin MD, Evis Z, Pleshko N. Early alterations in bone characteristics of type I diabetic rat femur: a Fourier transform infrared (FT-IR) imaging study. Appl Spectrosc. 2016;70:2005–15.
McNamara L, Parle E, Tio S, Behre A, Carey JJ, Murphy CG, et al. Bone mineral is more heterogeneously distributed in the femoral heads of osteoporotic and diabetic patients: a pilot study. JBMR Plus. 2019;4(2):e10253.
Sims N, Vrahnas C, Blank M, Dite TA, Tatarczuch L, Ansari N, et al. Increased autophagy in EphrinB2-deficient osteocytes is associated with elevated secondary mineralization and brittle bone. Nat Commun. 2019;10(1):3436.
Liu E, Wu M, Ai W, Chen L, Zhao S. Bradykinin receptors and EphB2/EphrinB2 pathway in response to high glucose-induced osteoblast dysfunction and hyperglycemia-induced bone deterioration in mice. Int J Mol Med. 2016;37(3):565–74.
Duer M, Davies E, Müller KH, Wong WC, Pickard CJ, Reid DG, et al. Citrate bridges between mineral platelets in bone. Proc Natl Acad Sci U S A. 2014;111(14):E1354–63.
Villaseñor A, Aedo-Martín D, Obeso D, Erjavec I, Rodríguez-Coira J, Buendía I, et al. Metabolomics reveals citric acid secretion in mechanically-stimulated osteocytes is inhibited by high glucose. Sci Rep. 2019;9(1):2295. https://doi.org/10.1038/s41598-018-38154-6.
Funding
This study was supported by Ministerio de Ciencia, Innovación y Universidades (SAF2016-80286).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Arancha Gortazar and Juan Ardura declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Osteocytes
Rights and permissions
About this article
Cite this article
Gortázar, A.R., Ardura, J.A. Osteocytes and Diabetes: Altered Function of Diabetic Osteocytes. Curr Osteoporos Rep 18, 796–802 (2020). https://doi.org/10.1007/s11914-020-00641-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-020-00641-z