Abstract
Purpose of Review
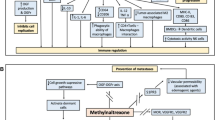
Opioids are still the most effective and widely used treatments for acute and chronic pain in cancer patients. This review focuses on the impact of opioids and mu-opioid receptors (MOR) on tumor progression and providing new ideas for targeting the MOR in cancer treatment.
Recent Findings
Studies estimated that opioids facilitate tumor progression and are related to the worse prognosis in cancer patients. As the primary receptor of opioids, MOR is involved in the regulation of malignant transformation of tumors and participating in proliferation, invasion, metastasis, and angiogenesis.
Summary
MOR may be a new molecular marker of malignant tumors and thus become a new target for cancer therapy, which may be beneficial to the outcomes of cancer patients.



Similar content being viewed by others
Abbreviations
- Cox-2:
-
cyclooxygenase-2
- EGFR:
-
epidermal growth factor receptor
- HIF-1:
-
hypoxia inducible factor-1
- ICAM:
-
intercellular adhesion molecule
- MAPK:
-
mitogen-activated protein kinase
- MMP-9:
-
matrix metalloproteinase 9
- MOR:
-
mu-opioid receptor
- SSTR2:
-
somatostatin receptor 2
- VEGF:
-
vascular endothelial growth factor
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30. https://doi.org/10.3322/caac.21590.
Vineis P, Wild CP. Global cancer patterns: causes and prevention. Lancet. 2014;383:549–57. https://doi.org/10.1016/s0140-6736(13)62224-2.
Fidler MM, Bray F, Soerjomataram I. The global cancer burden and human development: a review. Scand J Public Health. 2018;46:27–36. https://doi.org/10.1177/1403494817715400.
Matzner P, Sandbank E, Neeman E, Zmora O, Gottumukkala V, Ben-Eliyahu S. Harnessing cancer immunotherapy during the unexploited immediate perioperative period. Nat Rev Clin Oncol. 2020;17:313–26. https://doi.org/10.1038/s41571-019-0319-9.
Horowitz M, Neeman E, Sharon E, Ben-Eliyahu S. Exploiting the critical perioperative period to improve long-term cancer outcomes. Nat Rev Clin Oncol. 2015;12:213–26.
Sekandarzad MW, van Zundert AAJ, Lirk PB, Doornebal CW, Hollmann MW. Perioperative anesthesia care and tumor progression. Anesth Analg. 2017;124:1697–708. https://doi.org/10.1213/ane.0000000000001652.
Cox BM. A concise review of concepts in opioid pharmacology up to the discovery of endogenous opioids. Mol Pharmacol. 2020;98:392–400. https://doi.org/10.1124/mol.120.119420.
Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;100:57–70. https://doi.org/10.1016/s0092-8674(00)81683-9.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–74. https://doi.org/10.1016/j.cell.2011.02.013.
Kontomanolis EN, Koutras A, Syllaios A, Schizas D, Mastoraki A, Garmpis N, et al. Role of oncogenes and tumor-suppressor genes in carcinogenesis: a review. Anticancer Res. 2020;40:6009–15. https://doi.org/10.21873/anticanres.14622.
Foulds L. Tumor progression. Cancer Res. 1957;17:355–6.
Margraf A, Ludwig N, Zarbock A, Rossaint J. Systemic inflammatory response syndrome after surgery: mechanisms and protection. Anesth Analg. 2020;131:1693–707. https://doi.org/10.1213/ane.0000000000005175.
Stein C. Opioid Receptors. Annu Rev Med. 2016;67:433–51. https://doi.org/10.1146/annurev-med-062613-093100.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012.
Siuda ER, Carr R 3rd, Rominger DH, Violin JD. Biased mu-opioid receptor ligands: a promising new generation of pain therapeutics. Curr Opin Pharmacol. 2017;32:77–84. https://doi.org/10.1016/j.coph.2016.11.007.
Dietis N, Rowbotham DJ, Lambert DG. Opioid receptor subtypes: fact or artifact? Br J Anaesth. 2011;107:8–18. https://doi.org/10.1093/bja/aer115.
Trescot AM, Datta S, Lee M, Hansen H. Opioid pharmacology. Pain Phys. 2008;11:S133–53.
Kiguchi Y, Aono Y, Watanabe Y, Yamamoto-Nemoto S, Shimizu K, Shimizu T, et al. In vivo neurochemical evidence that delta1-, delta2- and mu2-opioid receptors, but not mu1-opioid receptors, inhibit acetylcholine efflux in the nucleus accumbens of freely moving rats. Eur J Pharmacol. 2016;789:402–10. https://doi.org/10.1016/j.ejphar.2016.07.028.
Lu H, Zhang H, Weng ML, Zhang J, Jiang N, Cata JP, et al. Morphine promotes tumorigenesis and cetuximab resistance via EGFR signaling activation in human colorectal cancer. J Cell Physiol. 2020. https://doi.org/10.1002/jcp.30161In this study, results indicated that EGFR inhibition by cetuximab strongly reversed the protumoral effects of morphine in vitro and in vivo. Collectively, we provide evidence that morphine-EGFR signaling might be a promising therapeutic target for CRC patients, especially for cetuximab-resistant CRC patients.
Chen DT, Pan JH, Chen YH, Xing W, Yan Y, Yuan YF, et al. The mu-opioid receptor is a molecular marker for poor prognosis in hepatocellular carcinoma and represents a potential therapeutic target. Br J Anaesth. 2019;122:e157–e67. https://doi.org/10.1016/j.bja.2018.09.030.
Friesen C, Hormann I, Roscher M, Fichtner I, Alt A, Hilger R, et al. Opioid receptor activation triggering downregulation of cAMP improves effectiveness of anti-cancer drugs in treatment of glioblastoma. Cell Cycle. 2014;13:1560–70.
Reed B, Butelman ER, Kreek MJ. Kappa opioid receptor antagonists as potential therapeutics for mood and substance use disorders. Handb Exp Pharmacol. 2020. https://doi.org/10.1007/164_2020_401.
Dripps IJ, Chen R, Shafer AM, Livingston KE, Disney A, Husbands SM, et al. Pharmacological properties of δ-opioid receptor-mediated behaviors: agonist efficacy and receptor reserve. J Pharmacol Exp Ther. 2020;374:319–30.
Gupta A, Gullapalli S, Pan H, Ramos-Ortolaza DL, Hayward MD, Low MJ, et al. Regulation of opioid receptors by their endogenous opioid peptides. Cell Mol Neurobiol. 2021;41:1103–18. https://doi.org/10.1007/s10571-020-01015-w.
Kiguchi N, Ding H, Kishioka S, Ko MC. Nociceptin/orphanin FQ peptide receptor-related ligands as novel analgesics. Curr Top Med Chem. 2020;20:2878–88.
Thompson AA, Liu W, Chun E, Katritch V, Wu H, Vardy E, et al. Structure of the nociceptin/orphanin FQ receptor in complex with a peptide mimetic. Nature. 2012;485:395–9.
Zhang H, Sun M, Zhou D, Gorur A, Sun Z, Zeng W, et al. Increased mu-opioid receptor expression is associated with reduced disease-free and overall survival in laryngeal squamous cell carcinoma. Br J Anaesth. 2020;125:722–9. https://doi.org/10.1016/j.bja.2020.07.051This study enrolled LSCC patients depending on MOR expression high or low. This study indicated that increased mu-opioid receptor expression is associated with reduced disease-free survival and overall survival in LSCC patients.
Scopsi L, Balslev E, Brunner N, Poulsen HS, Andersen J, Rank F, et al. Immunoreactive opioid peptides in human breast cancer. Am J Pathol. 1989;134:473–9.
Lennon FE, Mirzapoiazova T, Mambetsariev B, Poroyko VA, Salgia R, Moss J, et al. The Mu opioid receptor promotes opioid and growth factor-induced proliferation, migration and Epithelial Mesenchymal Transition (EMT) in human lung cancer. PLoS One. 2014;9:e91577.
Li Y, Li G, Tao T, Kang X, Liu C, Zhang X, et al. The μ-opioid receptor (MOR) promotes tumor initiation in hepatocellular carcinoma. Cancer Lett. 2019;453:1–9. https://doi.org/10.1016/j.canlet.2019.03.038In this study, results establish that MOR can be a novel and reliable HCSC marker and a potential therapeutic target against HCC via MOR-NFAT signaling.
Cieślińska A, Sienkiewicz-Szłapka E, Kostyra E, Fiedorowicz E, Snarska J, Wroński K, et al. μ-Opioid receptor gene (OPRM1) polymorphism in patients with breast cancer. Tumour Biol. 2015;36:4655–60.
Oh CS, Lee SH, Yoo YB, Yang JH, Kim SH. Mu-opioid receptor polymorphisms and breast cancer in a Korean female adult population: a retrospective study. J Breast Cancer. 2016;19:206–9.
Bortsov AV, Millikan RC, Belfer I, Boortz-Marx RL, Arora H, McLean SA. μ-Opioid receptor gene A118G polymorphism predicts survival in patients with breast cancer. Anesthesiology. 2012;116:896–902.
Lee YJ, Oh CS, Choi JM, Park S, Kim SH. mu-opioid receptor polymorphisms and breast cancer recurrence in adult Korean women undergoing breast cancer surgery: a retrospective study. Int J Med Sci. 2020;17:2941–6.
Wang S, Li Y, Liu XD, Zhao CX, Yang KQ. Polymorphism of A118G in μ-opioid receptor gene is associated with risk of esophageal squamous cell carcinoma in a Chinese population. Int J Clin Oncol. 2013;18:666–9. https://doi.org/10.1007/s10147-012-0441-5.
Xu X, Mao B, Wu L, Liu L, Rui J, Chen G. A118G Polymorphism in μ-opioid receptor gene and interactions with smoking and drinking on risk of oesophageal squamous cell carcinoma. J Clin Lab Anal. 2017;31:e22018.
Wu Q, Chen X, Wang J, Sun P, Weng M, Chen W, et al. Nalmefene attenuates malignant potential in colorectal cancer cell via inhibition of opioid receptor. Acta Biochim Biophys Sin Shanghai. 2018;50:156–63. https://doi.org/10.1093/abbs/gmx131.
Jorand R, Biswas S, Wakefield DL, Tobin SJ, Golfetto O, Hilton K, et al. Molecular signatures of mu opioid receptor and somatostatin receptor 2 in pancreatic cancer. Mol Biol Cell. 2016;27:3659–72.
Lu J, Liu Z, Zhao L, Tian H, Liu X, Yuan C. In vivo and in vitro inhibition of human liver cancer progress by downregulation of the μ-opioid receptor and relevant mechanisms. Oncol Rep. 2013;30:1731–8. https://doi.org/10.3892/or.2013.2640.
Xie N, Matigian N, Vithanage T, Gregory K, Nassar ZD, Cabot PJ, et al. Effect of perioperative opioids on cancer-relevant circulating parameters: Mu opioid receptor and Toll-like receptor 4 activation potential, and proteolytic profile. Clin Cancer Res. 2018;24:2319–27. https://doi.org/10.1158/1078-0432.Ccr-18-0172.
Lec PM, Lenis AT, Golla V, Brisbane W, Shuch B, Garraway IP, et al. The role of opioids and their receptors in urological malignancy: a review. J Urol. 2020;204:1150–9. https://doi.org/10.1097/ju.0000000000001156.
Zhang YF, Xu QX, Liao LD, Xu XE, Wu JY, Wu ZY, et al. Association of mu-opioid receptor expression with lymph node metastasis in esophageal squamous cell carcinoma. Dis Esophagus. 2015;28:196–203. https://doi.org/10.1111/dote.12165.
Hsiao PN, Chang MC, Cheng WF, Chen CA, Lin HW, Hsieh CY, et al. Morphine induces apoptosis of human endothelial cells through nitric oxide and reactive oxygen species pathways. Toxicology. 2009;256:83–91. https://doi.org/10.1016/j.tox.2008.11.015.
Ziche M, Morbidelli L. Nitric oxide and angiogenesis. J Neuro-Oncol. 2000;50:139–48. https://doi.org/10.1023/a:1006431309841.
Gupta K, Kshirsagar S, Chang L, Schwartz R, Law PY, Yee D, et al. Morphine stimulates angiogenesis by activating proangiogenic and survival-promoting signaling and promotes breast tumor growth. Cancer Res. 2002;62:4491–8.
Schito L. Hypoxia-dependent angiogenesis and lymphangiogenesis in cancer. Adv Exp Med Biol. 2019;1136:71–85. https://doi.org/10.1007/978-3-030-12734-3_5.
Singleton PA, Lingen MW, Fekete MJ, Garcia JG, Moss J. Methylnaltrexone inhibits opiate and VEGF-induced angiogenesis: role of receptor transactivation. Microvasc Res. 2006;72:3–11. https://doi.org/10.1016/j.mvr.2006.04.004.
Radisavljevic Z, Avraham H, Avraham S. Vascular endothelial growth factor up-regulates ICAM-1 expression via the phosphatidylinositol 3 OH-kinase/AKT/Nitric oxide pathway and modulates migration of brain microvascular endothelial cells. J Biol Chem. 2000;275:20770–4. https://doi.org/10.1074/jbc.M002448200.
Liu Z, Cheng S, Fu G, Ji F, Wang C, Cao M. Postoperative administration of ketorolac averts morphine-induced angiogenesis and metastasis in triple-negative breast cancer. Life Sci. 2020;251:117604. https://doi.org/10.1016/j.lfs.2020.117604.
Nguyen J, Luk K, Vang D, Soto W, Vincent L, Robiner S, et al. Morphine stimulates cancer progression and mast cell activation and impairs survival in transgenic mice with breast cancer. Br J Anaesth. 2014;113(Suppl 1):i4–13.
Koodie L, Yuan H, Pumper JA, Yu H, Charboneau R, Ramkrishnan S, et al. Morphine inhibits migration of tumor-infiltrating leukocytes and suppresses angiogenesis associated with tumor growth in mice. Am J Pathol. 2014;184:1073–84.
Yamamizu K, Hamada Y, Narita M. κ Opioid receptor ligands regulate angiogenesis in development and in tumours. Br J Pharmacol. 2015;172:268–76.
Cata JP, Keerty V, Keerty D, Feng L, Norman PH, Gottumukkala V, et al. A retrospective analysis of the effect of intraoperative opioid dose on cancer recurrence after non-small cell lung cancer resection. Cancer Med. 2014;3:900–8.
Pavlovskiĭ LN. Vydaiushchiĭsia nemetskiĭ vrach i issledovatel' Paul' Erlikh i ego rol' v razvitii immunologii i khimioterapii (k 150-letiiu so dnia rozhdeniia) [Famous German physician and researcher Paul Ehrlich and his role in the development of immunology and chemotherapy (to his 150-year birthday anniversary)]. Lik Sprava. 2004;(8):938. Russian.
Burnet FM. Immunological aspects of malignant disease. Lancet. 1967;1:1171–4. https://doi.org/10.1016/s0140-6736(67)92837-1.
Shavit Y, Terman GW, Lewis JW, Zane CJ, Gale RP, Liebeskind JC. Effects of footshock stress and morphine on natural killer lymphocytes in rats: studies of tolerance and cross-tolerance. Brain Res. 1986;372:382–5. https://doi.org/10.1016/0006-8993(86)91149-2.
Bryant HU, Bernton EW, Holaday JW. Morphine pellet-induced immunomodulation in mice: temporal relationships. J Pharmacol Exp Ther. 1988;245:913–20.
Vaghari BA, Ahmed OI, Wu CL. Regional anesthesia-analgesia: relationship to cancer recurrence and infection. Anesthesiol Clin. 2014;32:841–51. https://doi.org/10.1016/j.anclin.2014.08.004.
Shavit Y, Depaulis A, Martin FC, Terman GW, Pechnick RN, Zane CJ, et al. Involvement of brain opiate receptors in the immune-suppressive effect of morphine. Proc Natl Acad Sci U S A. 1986;83:7114–7.
Weber RJ, Pert A. The periaqueductal gray matter mediates opiate-induced immunosuppression. Science. 1989;245:188–90. https://doi.org/10.1126/science.2749256.
Maher DP, Walia D, Heller NM. Suppression of human natural killer cells by different classes of opioids. Anesth Analg. 2019;128:1013–21.
Yeager MP, Colacchio TA. Effect of morphine on growth of metastatic colon cancer in vivo. Arch Surg. 1991;126:454–6. https://doi.org/10.1001/archsurg.1991.01410280056007.
Gavériaux-Ruff C, Matthes HW, Peluso J, Kieffer BL. Abolition of morphine-immunosuppression in mice lacking the mu-opioid receptor gene. Proc Natl Acad Sci U S A. 1998;95:6326–30.
Boland JW, Pockley AG. Influence of opioids on immune function in patients with cancer pain: from bench to bedside. Br J Pharmacol. 2018;175:2726–36.
Thomas PT, Bhargava HN, House RV. Immunomodulatory effects of in vitro exposure to morphine and its metabolites. Pharmacology. 1995;50:51–62. https://doi.org/10.1159/000139266.
Vihinen P, Kähäri VM. Matrix metalloproteinases in cancer: prognostic markers and therapeutic targets. Int J Cancer. 2002;99:157–66. https://doi.org/10.1002/ijc.10329.
Houshyar H, Cooper ZD, Woods JH. Paradoxical effects of chronic morphine treatment on the temperature and pituitary-adrenal responses to acute restraint stress: a chronic stress paradigm. J Neuroendocrinol. 2001;13:862–74. https://doi.org/10.1046/j.1365-2826.2001.00713.x.
Zhang QJ, Luan JC, Wang YM, Song NH, Xia JD. Mu-opioid receptors in the paraventricular nucleus regulate ejaculatory behaviors via the sympathetic nerve system in male rats. Zhonghua Nan Ke Xue. 2020;26:867–74.
Fang H, Declerck YA. Targeting the tumor microenvironment: from understanding pathways to effective clinical trials. Cancer Res. 2013;73:4965–77.
Vincent L, Vang D, Nguyen J, Gupta M, Luk K, Ericson ME, et al. Mast cell activation contributes to sickle cell pathobiology and pain in mice. Blood. 2013;122:1853–62.
Das Roy L, Curry JM, Sahraei M, Besmer DM, Kidiyoor A, Gruber HE, et al. Arthritis augments breast cancer metastasis: role of mast cells and SCF/c-Kit signaling. Breast Cancer Res. 2013;15:R32.
Gach K, Szemraj J, Wyrębska A, Janecka A. The influence of opioids on matrix metalloproteinase-2 and -9 secretion and mRNA levels in MCF-7 breast cancer cell line. Mol Biol Rep. 2011;38:1231–6. https://doi.org/10.1007/s11033-010-0222-z.
Visse R, Nagase H. Matrix metalloproteinases and tissue inhibitors of metalloproteinases: structure, function, and biochemistry. Circ Res. 2003;92:827–39. https://doi.org/10.1161/01.Res.0000070112.80711.3d.
Khabbazi S, Hassanshahi M, Hassanshahi A, Peymanfar Y, Su YW, Xian CJ. Opioids and matrix metalloproteinases: the influence of morphine on MMP-9 production and cancer progression. Naunyn Schmiedeberg's Arch Pharmacol. 2019;392:123–33. https://doi.org/10.1007/s00210-019-01613-6.
Xie N, Khabbazi S, Nassar ZD, Gregory K, Vithanage T, Anand-Apte B, et al. Morphine alters the circulating proteolytic profile in mice: functional consequences on cellular migration and invasion. FASEB J. 2017;31:5208–16.
Afsharimani B, Baran J, Watanabe S, Lindner D, Cabot PJ, Parat MO. Morphine and breast tumor metastasis: the role of matrix-degrading enzymes. Clin Exp Metastasis. 2014;31:149–58. https://doi.org/10.1007/s10585-013-9616-3.
Khabbazi S, Goumon Y, Parat MO. Morphine modulates interleukin-4- or breast cancer cell-induced pro-metastatic activation of macrophages. Sci Rep. 2015;5:11389.
Pacifico F, Leonardi A. NF-kappaB in solid tumors. Biochem Pharmacol. 2006;72:1142–52. https://doi.org/10.1016/j.bcp.2006.07.032.
O’Sullivan S, Medina C, Ledwidge M, Radomski MW, Gilmer JF. Nitric oxide-matrix metaloproteinase-9 interactions: biological and pharmacological significance--NO and MMP-9 interactions. Biochim Biophys Acta. 1843;2014:603–17. https://doi.org/10.1016/j.bbamcr.2013.12.006.
Charbaji N, Rosenthal P, Schäfer-Korting M, Küchler S. Cytoprotective effects of opioids on irradiated oral epithelial cells. Wound Repair Regen. 2013;21:883–9. https://doi.org/10.1111/wrr.12115.
Börner C, Höllt V, Kraus J. Mechanisms of the inhibition of nuclear factor-κB by morphine in neuronal cells. Mol Pharmacol. 2012;81:587–97. https://doi.org/10.1124/mol.111.076620.
Law PY, Loh HH, Wei LN. Insights into the receptor transcription and signaling: implications in opioid tolerance and dependence. Neuropharmacology. 2004;47(Suppl 1):300–11. https://doi.org/10.1016/j.neuropharm.2004.07.013.
Zylla D, Gourley BL, Vang D, Jackson S, Boatman S, Lindgren B, et al. Opioid requirement, opioid receptor expression, and clinical outcomes in patients with advanced prostate cancer. Cancer. 2013;119:4103–10.
Steele GL, Dudek AZ, Gilmore GE, Richter SA, Olson DA, Eklund JP, et al. Impact of pain, opioids, and the Mu-opioid receptor on progression and survival in patients with newly diagnosed stage IV pancreatic cancer. Am J Clin Oncol. 2020;43:591–7. https://doi.org/10.1097/coc.0000000000000714.
Forget P, Tombal B, Scholtès JL, Nzimbala J, Meulders C, Legrand C, et al. Do intraoperative analgesics influence oncological outcomes after radical prostatectomy for prostate cancer? Eur J Anaesthesiol. 2011;28:830–5. https://doi.org/10.1097/EJA.0b013e32834b7d9a.
Akbari M, Naghibzadeh-Tahami A, Khanjani N, Baneshi MR, Kamali E, Hesampour M, et al. Opium as a risk factor for bladder cancer: a population-based case-control study in Iran. Arch Iran Med. 2015;18:567–71.
Hasegawa T, Oguri T, Osawa T, Sawa T, Osaga S, Okuyama T, et al. Opioid dose and survival of patients with incurable nonsmall cell lung cancer: a prospective cohort study. J Palliat Med. 2018;21:1436–41. https://doi.org/10.1089/jpm.2018.0044.
Oh TK, Jeon JH, Lee JM, Kim MS, Kim JH, Lim H, et al. Association of high-dose postoperative opioids with recurrence risk in esophageal squamous cell carcinoma: reinterpreting ERAS protocols for long-term oncologic surgery outcomes. Dis Esophagus. 2017;30:1–8. https://doi.org/10.1093/dote/dox074.
Boudreau DM, Chen L, Yu O, Bowles EJA, Chubak J. Risk of second breast cancer events with chronic opioid use in breast cancer survivors. Pharmacoepidemiol Drug Saf. 2019;28:740–53.
Inoue Y, Iwata T, Okugawa Y, Kawamoto A, Hiro J, Toiyama Y, et al. Prognostic significance of opioid use in the active treatment of advanced colorectal cancer. Mol Clin Oncol. 2013;1:59–64.
Diaz-Cambronero O, Mazzinari G, Cata JP. Perioperative opioids and colorectal cancer recurrence: a systematic review of the literature. Pain Manag. 2018;8:353–61. https://doi.org/10.2217/pmt-2018-0029.
Cronin-Fenton DP, Heide-Jørgensen U, Ahern TP, Lash TL, Christiansen PM, Ejlertsen B, et al. Opioids and breast cancer recurrence: a Danish population-based cohort study. Cancer. 2015;121:3507–14.
Cata JP, Zafereo M, Villarreal J, Unruh BD, Truong A, Truong DT, et al. Intraoperative opioids use for laryngeal squamous cell carcinoma surgery and recurrence: a retrospective study. J Clin Anesth. 2015;27:672–9. https://doi.org/10.1016/j.jclinane.2015.07.012.
Minami S, Fujimoto K, Ogata Y, Yamamoto S, Komuta K. Opioids have no negative effect on the survival time of patients with advanced lung cancer in an acute care hospital. Support Care Cancer. 2015;23:2245–54. https://doi.org/10.1007/s00520-014-2592-6.
Cronin-Fenton D. Opioids and breast cancer recurrence. Curr Opin Support Palliat Care. 2019;13:88–93. https://doi.org/10.1097/spc.0000000000000426.
Owusu-Agyemang P, Hayes-Jordan A, Van Meter A, Williams UU, Zavala AM, Kapoor R, et al. Assessing the survival impact of perioperative opioid consumption in children and adolescents undergoing cytoreductive surgery with hyperthermic intraperitoneal chemotherapy. Paediatr Anaesth. 2017;27:648–56. https://doi.org/10.1111/pan.13146.
Du KN, Feng L, Newhouse A, Mehta J, Lasala J, Mena GE, et al. Effects of intraoperative opioid use on recurrence-free and overall survival in patients with esophageal adenocarcinoma and squamous cell carcinoma. Anesth Analg. 2018;127:210–6. https://doi.org/10.1213/ane.0000000000003428.
Funding
This research was supported by the National Key Research and Development Program of China (NO. 2020YFC2008400); the National Natural Science Foundation of China (NO. 81873948, 81871591); Clinical Research Plan of SHDC (NO. SHDC2020CR4064, SHDC2020CR1005A); Shanghai Shenkang Hospital Development Center Clinical Science and Technology Innovation Project (NO. SHDC12018105); the Key Technology and Development Program of Shanghai (NO. 17411963400); 2019 Fudan University Zhuo-Xue Project (JIF159607); and Shanghai Leading Talent (NO: 2019-112). Shanghai Sailing Program (21YF1406800); Natural Science Foundation of Shanghai (21ZR1413400)
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical collection on Anesthesiology and Critical Care
Rights and permissions
About this article
Cite this article
Zhang, H., Zhou, D., Gu, J. et al. Targeting the mu-Opioid Receptor for Cancer Treatment. Curr Oncol Rep 23, 111 (2021). https://doi.org/10.1007/s11912-021-01107-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s11912-021-01107-w