Abstract
Purpose of Review
For patients with early stage non-small-cell lung cancer (NSCLC), thermal ablation (TA) has become in the least two decades an option of treatment used worldwide for patients with comorbidities who are not surgical candidates. Here, we review data published with different TA techniques: radiofrequency ablation (RFA), microwave ablation (MWA) and cryoablation. This paper reviews also the comparison that has been made between TA and stereotactic radiotherapy (SBRT).
Recent Findings
A majority of retrospective studies, the absence of comparative studies, and the variety of techniques make difficult to get evident data. Nevertheless, these stand-alone techniques have demonstrated local efficacy for tumors less than 3 cm and good tolerance on fragile patients. Many recent reviews and database analyses show that outcomes after TA (mainly RFA and MWA) are comparable to SBRT in terms of survival rates.
Summary
For patients who are unfit for surgery, TA has demonstrated interesting results for safety, benefits in overall survival, and acceptable local control.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Meza R, Meernik C, Jeon J, et al. Lung cancer incidence trends by gender, race and histology in the United States, 1973–2010. PLoS ONE 2015;10(3):e0121323.
Rami-Porta R, Tsuboi M. Sublobar resection for lung cancer. Eur Respir J. 2009;33(2):426–35.
Klapper JA, Hittinger SA, Denlinger CE. Alternatives to lobectomy for high-risk patients with early-stage non-small cell lung cancer. Ann Thorac Surg. 2017;103(4):1330–9.
• Wang L, Anraku M, Sato M, Nitadori JI, Nagayama K, Kitano K, et al. Impact of the 8th edition of the UICC-TNM classification on clinical stage 0-IA lung adenocarcinoma: does the new classification predict postoperative prognosis more precisely than the previous one? Ann Thorac Cardiovasc Surg. 2018;24(5):223–9 This team has retrospectively reviewed the data of clinical stage IA (7th edition) lung adenocarcinoma patients who underwent surgery from 2001 to 2012, and reclassified them by the 8th edition. The 8th edition of the UICC-TNM classification predicts postoperative prognosis more precisely than the 7th one in clinical stage 0-IA lung adenocarcinoma.
Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM, Beasley MB, et al. The 2015 World Health Organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol. 2015;10(9):1243–60.
Zheng M. Classification and pathology of lung cancer. Surg Oncol Clin N Am. 2016;25(3):447–68.
Tsutsumida H, Nomoto M, Goto M, Kitajima S, Kubota I, Hirotsu Y, et al. A micropapillary pattern is predictive of a poor prognosis in lung adenocarcinoma, and reduced surfactant apoprotein A expression in the micropapillary pattern is an excellent indicator of a poor prognosis. Mod Pathol. 2007;20(6):638–47.
• Masai K, Sakurai H, Sukeda A, Suzuki S, Asakura K, Nakagawa K, et al. Prognostic impact of margin distance and tumor spread through air spaces in limited resection for primary lung cancer. J Thorac Oncol. 2017;12(12):1788–97 This series shows that the presence of STAS and tumor margins less than 1 cm are significant risk factors for local recurrence after limited resections.
• Bains S, Eguchi T, Warth A, Yeh YC, Nitadori JI, Woo KM, et al. Procedure-specific risk prediction for recurrence in patients undergoing lobectomy or sublobar resection for small (≤2 cm) lung adenocarcinoma: an international cohort analysis. J Thorac Oncol. 2019;14(1):72–86 This analysis found that micropapillary pattern, solid pattern, lymphovascular invasion, and necrosis were involved in the risk prediction following lobectomy, and micropapillary pattern, spread through air spaces, lymphovascular invasion, and necrosis following sublobar resection.
• Kim SK, Kim TJ, Chung MJ, Kim TS, Lee KS, Zo JI, et al. Lung adenocarcinoma: CT features associated with spread through air spaces. Radiology. 2018;289(3):831–40 From this article we learnt that spread through air spaces (STAS) beyond the edge of the main tumor is a risk factor for local recurrence after a local treatment. CT images may help identify the presence of STAS and may influence treatment decisions regarding the adequate extent of surgery or local ablative therapies.
Ahmed M, Liu Z, Afzal KS, Weeks D, Lobo SM, Kruskal JB, et al. Radiofrequency ablation: effect of surrounding tissue composition on coagulation necrosis in a canine tumor model. Radiology. 2004;230:761–7.
Sidoff L, Dupuy DE. Clinical experiences with microwave thermal ablation of lung malignancies. Int J Hyperth. 2017;33(1):25–33.
• Brace CL, Hinshaw JL, Laeseke PF, Sampson LA, Lee FT Jr. Pulmonary thermal ablation: comparison of radiofrequency and microwave devices by using gross pathologic and CT findings in a swine model. Radiology. 2009;251:705–11 In this article, microwave ablation with a 17-gauge high-power triaxial antenna creates larger and more circular zones of ablation than does a similarly sized RF applicator in a preclinical animal model.
de Baere T, Tselikas L, Woodrum D, Abtin F, Littrup P, Deschamps F, et al. Evaluating cryoablation of metastatic lung tumors in patients--safety and efficacy: the ECLIPSE trial--interim analysis at 1 year. J Thorac Oncol. 2015;10(10):1468–74.
Iguchi T, Hiraki T, Gobara H, Fujiwara H, Matsui Y, Soh J, et al. Percutaneous radiofrequency ablation of lung cancer presenting as ground-glass opacity. Cardiovasc Intervent Radiol. 2015;38(2):409–15.
Yang X, Ye X, Lin Z, Jin Y, Zhang K, Dong Y, et al. Computed tomography-guided percutaneous microwave ablation for treatment of peripheral ground-glass opacity-lung adenocarcinoma: a pilot study. J Cancer Res Ther. 2018;14(4):764–71.
Dupuy DE, Mayo-Smith WW, Abbott GF, DiPetrillo T. Clinical applications of radio-frequency tumor ablation in the thorax. Radiographics. 2002;22:S259–S69.
Dupuy DE. Image-guided thermal ablation of lung malignancies. Radiology. 2011;260:633–55.
Ambrogi MC, Fontanini G, Cioni R, Faviana P, Fanucchi O, Mussi A. Biologic effects of radiofrequency thermal ablation on non-small cell lung cancer: results of a pilot study. J Thorac Cardiovasc Surg. 2006;131(5):1002–6.
• Giraud P, Antoine M, Larrouy A, et al. Evaluation of microscopic tumor extension in non-small-cell lung cancer for three-dimensional conformal radiotherapy planning. Int J Radiat Oncol Biol Phys. 2000;48:1015–24 This article concluded that microscopic extension was different between adenocarcinoma (ADC) and squamous cell carcinoma (SCC). To cover 95% of the microscopic extension the clinical target volume must be increased to 8 mm and 6 mm for ADC and SCC respectively.
Beland MD, Wasser EJ, Mayo-Smith WW, Dupuy DE. Primary non-small cell lung cancer: review of frequency, location, and time of recurrence after radiofrequency ablation. Radiology. 2010;254(1):301–7.
de Baere T, Palussiere J, Auperin A, et al. Mid-term local efficacy and survival after radiofrequency ablation of lung tumors with a minimum follow-up of 1 year: prospective evaluation. Radiology. 2006;240:587–96.
• Gillams AR, Lees WR. Radiofrequency ablation of lung metastases: factors influencing success. Eur Radiol. 2008;18:672–7 This article concluded that peripheral tumors less than 3.5 cm with no large vessel contact are the optimal tumors for RFA.
Nelson DB, Tam AL, Mitchell KG, Rice DC, Mehran RJ, Sepesi B, et al. Local recurrence after microwave ablation of lung malignancies: a systematic review. Ann Thorac Surg. 2019;107(6):1876–83.
Callstrom MR, Woodrum DA, Nichols FC, Palussiere J, Buy X, Suh RD, et al. Multicenter study of metastatic lung tumors targeted by interventional cryoablation evaluation (SOLSTICE). J Thorac Oncol. 2020;15(7):1200–9.
Dupuy DE, Fernando HC, Hillman S, Ng T, Tan AD, Sharma A, et al. Radiofrequency ablation of stage IA non-small cell lung cancer in medically inoperable patients: results from the American College of Surgeons Oncology Group Z4033 (Alliance) trial. Cancer. 2015;121(19):3491–8.
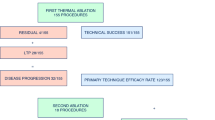
Palussière J, Chomy F, Savina M, Deschamps F, Gaubert JY, Renault A, et al. Radiofrequency ablation of stage IA non-small cell lung cancer in patients ineligible for surgery: results of a prospective multicenter phase II trial. J Cardiothorac Surg. 2018;13(1):91.
Lencioni R, Crocetti L, Cioni R, Suh R, Glenn D, Regge D, et al. Response to radiofrequency ablation of pulmonary tumours: a prospective, intention-to-treat, multicentre clinical trial (the RAPTURE study). Lancet Oncol. 2008;9(7):621–8.
Simon CJ, Dupuy DE, Dipetrillo TA, et al. Pulmonary radiofrequency ablation: long-term safety and efficacy in 153 patients. Radiology. 2007;243:268–75.
Palussiere J, Lagarde P, Auperin A, et al. Percutaneous lung thermal ablation of non-surgical clinical N0 non-small cell lung cancer: results of eight years’ experience in 87 patients from two centers. Cardiovasc Intervent Radiol. 2015;38:160–6.
• Yang X, Ye X, Huang G, et al. Repeated percutaneous microwave ablation for local recurrence of inoperable stage I non small cell lung cancer. J Can Res Ther. 2017;13:683–8 This article showed that local recurrence was higher in tumors > 3.5 cm than that of in tumors ≤3.5 cm. For patients with local recurrence, to repeat, MWA achieved similar OS and PFS as patients without local recurrence. No additional complications were reported in the repeat MWA compared to the original MWA.
McDevitt JL, Mouli SK, Nemcek AA, et al. Percutaneous cryoablation for the treatment of primary and metastatic lung tumors: identification of risk factors for recurrence and major complications. J Vasc Interv Radiol. 2016;27(09):1371–9.
Kodama H, Yamakado K, Takaki H, Kashima M, Uraki J, Nakatsuka A, et al. Lung radiofrequency ablation for the treatment of unresectable recurrent non-small-cell lung cancer after surgical intervention. Cardiovasc Intervent Radiol. 2012;35:563–9.
Hess A, Palussiere J, Goyers JF, et al. Pulmonary radiofrequency ablation in patients with a single lung: feasibility, efficacy, and tolerance. Radiology. 2011;258(2):635–42.
Yang X, Ye X, Zhang L, Geng D, du Z, Yu G, et al. Microwave ablation for lung cancer patients with a single lung: clinical evaluation of 11 cases. Thorac Cancer. 2018;9(5):548–54.
• Brooks ED, Verma V, Senan S. Salvage therapy for locoregional recurrence after stereotactic ablative radiotherapy for early-stage NSCLC. J Thorac Oncol. 2020;15(2):176–89 This article concluded that survival for patients with adequately salvaged local recurrences is similar to that for patients after primary SBRT without recurrence. TA is one of the possible treatments of local recurrence.
• Brooks ED, Sun B, Feng L, Verma V, Zhao L, Gomez DR, et al. Association of long-term outcomes and survival with multidisciplinary salvage treatment for local and regional recurrence after stereotactic ablative radiotherapy for early-stage lung cancer. JAMA Netw Open. 2018;1:e181390 This article showed that life expectancy after salvage treatment for isolated local recurrence was similar to that for patients without recurrence.
• Lam A, Yoshida EJ, Bui K, Fernando D, Nelson K, Abi-Jaoudeh N. A national cancer database analysis of radiofrequency ablation versus stereotactic body radiotherapy in early-stage non–small cell lung cancer. J Vasc Interv Radiol. 2018;29(9):1211–7 From a national cancer database analysis, this article concluded that at high-volume centers, no significant difference in overall survival was seen between patients with early-stage NSCLC treated with RF ablation and SBRT.
Uhlig J, Ludwig JM, Goldberg SB, Chiang A, Blasberg JD, Kim HS. Survival rates after thermal ablation versus stereotactic radiation therapy for stage 1 non-small cell lung cancer: a national cancer database study. Radiology. 2018;289(3):862–70.
• Bi N, Shedden K, Zheng X, Kong FS. Comparison of the effectiveness of radiofrequency ablation with stereotactic body radiation therapy in inoperable stage i non-small cell lung cancer: a systemic review and pooled analysis. Int J Radiat Oncol Biol Phys. 2016;95(5):1378–90 This is a comprehensive literature search for published trials from 2001 to 2012. Pooled analyses were performed to obtain overall survival (OS) and local tumor control rates (LCRs) and adverse events. Regression analysis was conducted considering each study’s proportions of stage IA and age. Compared with RFA, SBRT seems to have a higher LCR but similar OS.
Watson R, Tol I, Gunawardana S, et al. Is microwave ablation an alternative to stereotactic ablative body radiotherapy in patients with inoperable early-stage primary lung cancer? Interact Cardiovasc Thorac Surg. 2019;29:539–43.
Vyfhuis MAL, Mohindra P, Simone CB 2nd. stereotactic body radiation therapy versus thermal ablation for early stage non-small cell lung cancer. Radiology. 2019;290(2):574–5.
Iguchi T, Hiraki T, Matsui Y, Mitsuhashi T, Katayama N, Katsui K, et al. Survival outcomes of treatment with radiofrequency ablation, stereotactic body radiotherapy, or sublobar resection for patients with clinical stage I non-small-cell lung cancer: a single-center evaluation. J Vasc Interv Radiol. 2020;31(7):1044–51.
Crabtree T, Puri V, Timmerman R, Fernando H, Bradley J, Decker PA, et al. Treatment of stage I lung cancer in high-risk and inoperable patients: comparison of prospective clinical trials using stereotactic body radiotherapy (RTOG 0236), sublobar resection (ACOSOG Z4032), and radiofrequency ablation (ACOSOG Z4033). J Thorac Cardiovasc Surg. 2013;145(03):692–9.
Kwan SW, Mortell KE, Talenfeld AD, Brunner MC. Thermal ablation matches sublobar resection outcomes in older patients with early-stage non-small cell lung cancer. J Vasc Interv Radiol. 2014;25(1):1–9.
Kwan SW, Mortell KE, Hippe DS, Brunner MC. An economic analysis of sublobar resection versus thermal ablation for earlystage non-small-cell lung cancer. J Vasc Interv Radiol. 2014;25(10):1558–64.
Kashima M, Yamakado K, Takaki H, Kodama H, Yamada T, Uraki J, et al. Complications after 1000 lung radiofrequency ablation sessions in 420 patients: a single center’s experiences. AJR Am J Roentgenol. 2011;197:W576–80.
Jiang B, Mcclure MA, Chen T, et al. Efficacy and safety of thermal ablation of lung malignancies: a network meta-analysis. Ann Thorac Med. 2018;13(4):243–50.
• Lam A, Yoshida EJ, Bui K, Katrivesis J, Fernando D, Nelson K, et al. Patient and facility demographics related outcomes in early-stage non-small cell lung cancer treated with radiofrequency ablation: a national cancer database analysis. J Vasc Interv Radiol. 2018;29(11):1535–41 This article showed from the national cancer database analysis that patients with early-stage NSCLC treated with RF ablation at high-volume centers (top 95th percentile of facilities by number of procedures performed) experienced a significant increase in OS, suggesting regionalization of lung cancer management as a means of improving outcomes.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Jean Palussière has received clinical trial support from the PHRC (national public grant from the French Ministry of Health) and Boston Scientific. Maxime Cazayus, Sophie Cousin, Mathilde Cabart, François Chomy, and Vittorio Catena declare no conflict of interest. Xavier Buy has received compensation from Galil Medical/Boston Scientific for serving as a proctor.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Interventional Oncology
Rights and permissions
About this article
Cite this article
Palussière, J., Cazayus, M., Cousin, S. et al. Is There a Role for Percutaneous Ablation for Early Stage Lung Cancer? What Is the Evidence?. Curr Oncol Rep 23, 81 (2021). https://doi.org/10.1007/s11912-021-01072-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s11912-021-01072-4