Abstract
Purpose of Review
Chronic myelogenous leukemia (CML) is rare in children, requiring extrapolation from treatment of adults. In this review, we explore similarities and differences between adult and pediatric CML with a focus on therapeutic advances and emerging clinical questions.
Recent Findings
Pediatric CML is effectively treated with long-term targeted therapy using tyrosine kinase inhibitors (TKIs). Newly diagnosed pediatric patients in chronic phase can now be treated with imatinib, dasatinib, or nilotinib without allogeneic hematopoietic stem cell transplantation. While treatment-free remission is possible in adults in chronic phase with optimal response to therapy, data are currently insufficient to support stopping TKI in pediatrics outside of a clinical trial. Knowledge gaps remain regarding long-term and late effects of TKIs in pediatric CML.
Summary
Targeted therapy has markedly improved outcomes for pediatric CML, while raising a number of clinical questions, including the possibility of treatment-free remission and long-term health implications of prolonged TKI exposure at a young age.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
SEER Cancer Stat Facts: Chronic Myeloid Leukemia. National Cancer Institute. Bethesda. Available at: https://seer.cancer.gov/statfacts/html/cmyl.html. Accessed 7/2/2020.
Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M et al. SEER Cancer Statistics Review, 1975-2017. National Cancer Institute Bethesda, MD, https://seercancergov/csr/1975_2017/, based on November 2019 SEER data submission, posted to the SEER web site, April 2020.
Bower H, Björkholm M, Dickman PW, Höglund M, Lambert PC, Andersson TML. Life expectancy of patients with chronic myeloid leukemia approaches the life expectancy of the general population. J Clin Oncol. 2016;34(24):2851–7. https://doi.org/10.1200/JCO.2015.66.2866.
Sasaki K, Strom SS, O’Brien S, Jabbour E, Ravandi F, Konopleva M, et al. Relative survival in patients with chronic-phase chronic myeloid leukaemia in the tyrosine-kinase inhibitor era: analysis of patient data from six prospective clinical trials. Lancet Haematol. 2015;2(5):e186–e93. https://doi.org/10.1016/S2352-3026(15)00048-4.
Knöfler R, Lange BS, Paul F, Tiebel O, Suttorp M. Bleeding signs due to acquired von Willebrand syndrome at diagnosis of chronic myeloid leukaemia in children. Br J Haematol. 2020;188(5):701–6. https://doi.org/10.1111/bjh.16241.
Hijiya N, Schultz KR, Metzler M, Millot F, Suttorp M. Pediatric chronic myeloid leukemia is a unique disease that requires a different approach. Blood. 2016;127(4):392–9. https://doi.org/10.1182/blood-2015-06-648667.
Baccarani M, Castagnetti F, Gugliotta G, Rosti G. A review of the European LeukemiaNet recommendations for the management of CML. Ann Hematol. 2015;94(2):141–7. https://doi.org/10.1007/s00277-015-2322-2.
National Comprehensive Cancer Network. NCCN Guidelines, Chronic Myeloid Leukemia (version 3.2020), 2020. Available at: https://www.nccn.org/professionals/physician_gls/pdf/cml.pdf. Accessed 8/10/2020.
Hochhaus A, Baccarani M, Silver RT, Schiffer C, Apperley JF, Cervantes F, et al. European LeukemiaNet 2020 recommendations for treating chronic myeloid leukemia. Leukemia. 2020;34(4):966–84. https://doi.org/10.1038/s41375-020-0776-2.
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405. https://doi.org/10.1182/blood-2016-03-643544.
• Millot F, Maledon N, Guilhot J, Güneş AM, Kalwak K, Suttorp M. Favourable outcome of de novo advanced phases of childhood chronic myeloid leukaemia. Eur J Cancer. 2019;115:17–23. https://doi.org/10.1016/j.ejca.2019.03.020This report from an international pediatric CML registry presents the largest observational experience of newly diagnosed children and adolescents during the TKI treatment era. Notable findings include the proportion in advanced phase at diagnosis (7.5%) and observation that some patients with de novo advanced phase were effectively treated without HSCT.
Ernst T, Busch M, Rinke J, Ernst J, Haferlach C, Beck JF, et al. Frequent ASXL1 mutations in children and young adults with chronic myeloid leukemia. Leukemia. 2018;32(9):2046–9. https://doi.org/10.1038/s41375-018-0157-2.
Liang DC, Liu HC, Yang CP, Jaing TH, Hung IJ, Yeh TC, et al. Cooperating gene mutations in childhood acute myeloid leukemia with special reference on mutations of ASXL1, TET2, IDH1, IDH2, and DNMT3A. Blood. 2013;121(15):2988–95. https://doi.org/10.1182/blood-2012-06-436782.
Shih AH, Abdel-Wahab O, Patel JP, Levine RL. The role of mutations in epigenetic regulators in myeloid malignancies. Nat Rev Cancer. 2012;12(9):599–612. https://doi.org/10.1038/nrc3343.
Abdel-Wahab O, Dey A. The ASXL-BAP1 axis: new factors in myelopoiesis, cancer and epigenetics. Leukemia. 2013;27(1):10–5. https://doi.org/10.1038/leu.2012.288.
de Cássia Viu Carrara R, Fontes AM, Abraham KJ, Orellana MD, Haddad SK, Palma PVB, et al. Expression differences of genes in the PI3K/AKT, WNT/b-catenin, SHH, NOTCH and MAPK signaling pathways in CD34+ hematopoietic cells obtained from chronic phase patients with chronic myeloid leukemia and from healthy controls. Clin Transl Oncol. 2018;20(4):542–9. https://doi.org/10.1007/s12094-017-1751-x.
Drozdov D, Bonaventure A, Nakata K, Suttorp M, Belot A. Temporal trends in the proportion of “cure” in children, adolescents, and young adults diagnosed with chronic myeloid leukemia in England: a population-based study. Pediatr Blood Cancer. 2018;65(12):e27422. https://doi.org/10.1002/pbc.27422.
Druker BJ. STI571 (Gleevec™) as a paradigm for cancer therapy. Trends Mol Med. 2002;8(4):S14–S8. https://doi.org/10.1016/S1471-4914(02)02305-5.
Cohen MH, Williams G, Johnson JR, Duan J, Gobburu J, Rahman A, et al. Approval summary for imatinib mesylate capsules in the treatment of chronic myelogenous leukemia. Clin Cancer Res. 2002;8(5):935–42.
Athale U, Hijiya N, Patterson BC, Bergsagel J, Andolina JR, Bittencourt H, et al. Management of chronic myeloid leukemia in children and adolescents: recommendations from the Children’s Oncology Group CML working group. Pediatr Blood Cancer. 2019;66(9):e27827. https://doi.org/10.1002/pbc.27827.
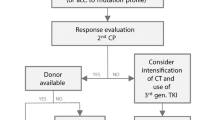
• Hijiya N, Suttorp M. How I treat chronic myeloid leukemia in children and adolescents. Blood. 2019;133(22):2374–84. https://doi.org/10.1182/blood.2018882233This case-based review provides a clinically relevant contemporary perspective on management of challenging clinical scenarios arising in treatment of pediatric CML, including suboptimal response to initial TKI, poor adherence to treatment, side effect arising on therapy, and de novo advanced-phase CML.
Millot F, Baruchel A, Guilhot J, Petit A, Leblanc T, Bertrand Y, et al. Imatinib Is effective in children with previously untreated chronic myelogenous leukemia in early chronic phase: results of the French national phase IV trial. J Clin Oncol. 2011;29(20):2827–32. https://doi.org/10.1200/JCO.2010.32.7114.
Champagne MA, Fu CH, Chang M, Chen H, Gerbing RB, Alonzo TA, et al. Higher dose imatinib for children with de novo chronic phase chronic myelogenous leukemia: a report from the Children’s Oncology Group. Pediatr Blood Cancer. 2011;57(1):56–62. https://doi.org/10.1002/pbc.23031.
•• Suttorp M, Schulze P, Glauche I, Göhring G, von Neuhoff N, Metzler M, et al. Front-line imatinib treatment in children and adolescents with chronic myeloid leukemia: results from a phase III trial. Leukemia. 2018;32(7):1657–69. https://doi.org/10.1038/s41375-018-0179-9This nonrandomized phase 3 clinical trial of imatinib for newly diagnosed pediatric CML includes 140 patients with chronic-phase CML, making it the largest prospective pediatric study to date. Results extend and confirm earlier phase trials showing efficacy and safety of imatinib.
• Vener C, Banzi R, Ambrogi F, Ferrero A, Saglio G, Pravettoni G, et al. First-line imatinib vs second- and third-generation TKIs for chronic-phase CML: a systematic review and meta-analysis. Blood Adv. 2020;4(12):2723–35. https://doi.org/10.1182/bloodadvances.2019001329The authors present a systematic review and meta-analysis of seven randomized controlled trials of frontline TKI treatment for chronic-phase CML in adults age ≥ 18 years, with a focus on both efficacy and toxicity. For adults with CML, data support use of a second- or third-generation TKI based on efficacy and use of imatinib for patients with comorbidities based on toxicity profiles.
•• Gore L, Kearns PR, de Martino ML, De Souza Lee CA, Bertrand Y, et al. Dasatinib in pediatric patients with chronic myeloid leukemia in chronic phase: results from a phase II trial. J Clin Oncol. 2018;36(13):1330–8. https://doi.org/10.1200/JCO.2017.75.9597This phase 2 clinical trial demonstrated efficacy and safety of dasatinib in 84 pediatric patients with newly diagnosed chronic-phase CML, providing data to support FDA approval.
•• Hijiya N, Maschan A, Rizzari C, Shimada H, Dufour C, Goto H, et al. Phase 2 study of nilotinib in pediatric patients with Philadelphia chromosome–positive chronic myeloid leukemia. Blood. 2019;134(23):2036–45. https://doi.org/10.1182/blood.2019000069This phase 2 clinical trial demonstrated efficacy and safety of nilotinib in 25 pediatric patients with newly diagnosed chronic-phase CML, providing data to support FDA approval.
Cortes JE, Kim D-W, Pinilla-Ibarz J, le Coutre PD, Paquette R, Chuah C, et al. Ponatinib efficacy and safety in Philadelphia chromosome–positive leukemia: final 5-year results of the phase 2 PACE trial. Blood. 2018;132(4):393–404. https://doi.org/10.1182/blood-2016-09-739086.
Lipton JH, Chuah C, Guerci-Bresler A, Rosti G, Simpson D, Assouline S, et al. Ponatinib versus imatinib for newly diagnosed chronic myeloid leukaemia: an international, randomised, open-label, phase 3 trial. Lancet Oncol. 2016;17(5):612–21. https://doi.org/10.1016/S1470-2045(16)00080-2.
Müller MC, Cervantes F, Hjorth-Hansen H, Janssen JJWM, Milojkovic D, Rea D, et al. Ponatinib in chronic myeloid leukemia (CML): consensus on patient treatment and management from a European expert panel. Crit Rev Oncol Hematol. 2017;120:52–9. https://doi.org/10.1016/j.critrevonc.2017.10.002.
• Rossoff J, Huynh V, Rau RE, Macy ME, Sulis ML, Schultz KR, et al. Experience with ponatinib in paediatric patients with leukaemia. Br J Haematol. 2020;189(2):363–8. https://doi.org/10.1111/bjh.16338One of two multi-institutional retrospective studies published in 2020 that describes clinical experience with ponatinib in pediatric patients’ results shows tolerability of ponatinib with no reports of vascular toxicity thus far. Despite having low patient numbers, both studies are important for clinicians considering ponatinib in pediatric patients resistant to all approved TKIs.
• Millot F, Suttorp M, Versluys AB, Kalwak K, Nelken B, Ducassou S, et al. Ponatinib in childhood Philadelphia chromosome–positive leukaemias: an international registry of childhood chronic myeloid leukaemia study. Eur J Cancer. 2020;136:107–12. https://doi.org/10.1016/j.ejca.2020.05.020One of two multi-institutional retrospective studies published in 2020 that describes clinical experience with ponatinib in pediatric patients’ results shows tolerability of ponatinib with no reports of vascular toxicity thus far. Despite having low patient numbers, both studies are important for clinicians considering ponatinib in pediatric patients resistant to all approved TKIs.
Andolina JR, Burke MJ, Hijiya N, Chaudhury S, Schultz KR, Roth ME. Practice patterns of physician treatment for pediatric chronic myelogenous leukemia. Biol Blood Marrow Transplant. 2019;25(2):321–7. https://doi.org/10.1016/j.bbmt.2018.09.029.
de la Fuente J, Baruchel A, Biondi A, de Bont E, Dresse M-F, Suttorp M, et al. Managing children with chronic myeloid leukaemia (CML): recommendations for the management of CML in children and young people up to the age of 18 years. Br J Haematol. 2014;167(1):33–47. https://doi.org/10.1111/bjh.12977.
Jabbour E, Kantarjian H. Chronic myeloid leukemia: 2020 update on diagnosis, therapy and monitoring. Am J Hematol. 2020;95(6):691–709. https://doi.org/10.1002/ajh.25792.
Hughes TP, Mauro MJ, Cortes JE, Minami H, Rea D, DeAngelo DJ, et al. Asciminib in chronic myeloid leukemia after ABL kinase inhibitor failure. New England Journal of Medicine. 2019;381(24):2315–26. https://doi.org/10.1056/NEJMoa1902328.
Shima H, Kada A, Tanizawa A, Yuza Y, Watanabe A, Ito M, et al. Discontinuation of tyrosine kinase inhibitor in children with chronic myeloid leukemia (JPLSG STKI-14 study). Blood. 2019;134(Supplement_1):25. https://doi.org/10.1182/blood-2019-122623.
Millot F, Claviez A, Leverger G, Corbaciglu S, Groll AH, Suttorp M. Imatinib cessation in children and adolescents with chronic myeloid leukemia in chronic phase: imatinib cessation in children with CML. Pediatr Blood Cancer. 2014;61(2):355–7. https://doi.org/10.1002/pbc.24521.
• Giona F, Malaspina F, Putti MC, Ladogana S, Mura R, Burnelli R, et al. Results and outcome of intermittent imatinib (ON/OFF schedule) in children and adolescents with chronic myeloid leukaemia. Br J Haematol. 2020;188(6):e101–5. https://doi.org/10.1111/bjh.16388This brief report presents a novel intermittent imatinib dosing strategy that was used in 15 pediatric patients in one of three distinct clinical scenarios: (a) deep molecular response as a bridge before stopping TKI, (b) deep molecular response with adverse long-term effects from TKI, or (3) poor adherence to continuous imatinib. While preliminary and based on low patient numbers, results support feasibility of this approach for some patients and lay the groundwork for future studies.
Berger MG, Pereira B, Rousselot P, Cony-Makhoul P, Gardembas M, Legros L, et al. Longer treatment duration and history of osteoarticular symptoms predispose to tyrosine kinase inhibitor withdrawal syndrome. Br J Haematol. 2019;187(3):337–46. https://doi.org/10.1111/bjh.16083.
Moslehi JJ, Deininger M. Tyrosine kinase inhibitor-associated cardiovascular toxicity in chronic myeloid leukemia. J Clin Oncol. 2015;33(35):4210–8. https://doi.org/10.1200/JCO.2015.62.4718.
Chow EJ, Antal Z, Constine LS, Gardner R, Wallace WH, Weil BR, et al. New agents, emerging late effects, and the development of precision survivorship. J Clin Oncol. 2018;36(21):2231–40. https://doi.org/10.1200/JCO.2017.76.4647.
Millot F, Guilhot J, Baruchel A, Petit A, Leblanc T, Bertrand Y, et al. Growth deceleration in children treated with imatinib for chronic myeloid leukaemia. Eur J Cancer. 2014;50(18):3206–11. https://doi.org/10.1016/j.ejca.2014.10.007.
Tauer JT, Nowasz C, Sedlacek P, de Bont ESJM, Aleinikova OV, Suttorp M. Impairment of longitudinal growth by tyrosine kinase inhibitor (TKI) treatment-data from a large pediatric cohort with chronic myeloid leukemia (CML). Blood. 2014;124(21):522. https://doi.org/10.1182/blood.V124.21.522.522.
Bansal D, Shava U, Varma N, Trehan A, Marwaha RK. Imatinib has adverse effect on growth in children with chronic myeloid leukemia. Pediatr Blood Cancer. 2012;59(3):481–4. https://doi.org/10.1002/pbc.23389.
Rastogi MV, Stork L, Druker B, Blasdel C, Nguyen T, Boston BA. Imatinib mesylate causes growth deceleration in pediatric patients with chronic myelogenous leukemia. Pediatr Blood Cancer. 2012;59(5):840–5. https://doi.org/10.1002/pbc.24121.
Hobernicht SL, Schweiger B, Zeitler P, Wang M, Hunger SP. Acquired growth hormone deficiency in a girl with chronic myelogenous leukemia treated with tyrosine kinase inhibitor therapy. Pediatr Blood Cancer. 2011;56(4):671–3. https://doi.org/10.1002/pbc.22945.
Sabnis HS, Keenum C, Lewis RW, Patterson B, Bergsagel J, Effinger KE, et al. Growth disturbances in children and adolescents receiving long-term tyrosine kinase inhibitor therapy for chronic myeloid leukaemia or Philadelphia chromosome-positive acute lymphoblastic leukaemia. Br J Haematol. 2019;185(4):795–9. https://doi.org/10.1111/bjh.15633.
Narayanan KR, Bansal D, Walia R, Sachdeva N, Bhansali A, Varma N, et al. Growth failure in children with chronic myeloid leukemia receiving imatinib is due to disruption of GH/IGF-1 axis. Pediatr Blood Cancer. 2013;60(7):1148–53. https://doi.org/10.1002/pbc.24397.
Walia R, Aggarwal A, Bhansali A, Aggarwal A, Varma N, Sachdeva N, et al. Acquired neuro-secretory defect in growth hormone secretion due to imatinib mesylate and the efficacy of growth hormone therapy in children with chronic myeloid leukemia. Pediatr Hematol Oncol. 2020;37(2):99–108. https://doi.org/10.1080/08880018.2019.1689320.
Vandyke K, Dewar AL, Fitter S, Menicanin D, To LB, Hughes TP, et al. Imatinib mesylate causes growth plate closure in vivo. Leukemia. 2009;23(11):2155–9. https://doi.org/10.1038/leu.2009.150.
Balakumaran J, Birk T, Golemiec B, Helmeczi W, Inkaran J, Kao Y-Y, et al. Evaluating the endometabolic and bone health effects of tyrosine kinase inhibitors in chronic myeloid leukaemia: a systematic review protocol. BMJ Open. 2019;9(9):e030092. https://doi.org/10.1136/bmjopen-2019-030092.
Samis J, Lee P, Zimmerman D, Arceci RJ, Suttorp M, Hijiya N. Recognizing endocrinopathies associated with tyrosine kinase inhibitor therapy in children with chronic myelogenous leukemia. Pediatr Blood Cancer. 2016;63(8):1332–8. https://doi.org/10.1002/pbc.26028.
Salem W, Li K, Krapp C, Ingles SA, Bartolomei MS, Chung K, et al. Imatinib treatments have long-term impact on placentation and embryo survival. Sci Rep. 2019;9(1):1–10. https://doi.org/10.1038/s41598-019-39134-0.
Seshadri T, Seymour JF, McArthur GA. Oligospermia in a patient receiving imatinib therapy for the hypereosinophilic syndrome. N Engl J Med. 2004;351(20):2134–5. https://doi.org/10.1056/NEJM200411113512024.
Chang X, Zhou L, Chen X, Xu B, Cheng Y, Sun S, et al. Impact of imatinib on the fertility of male patients with chronic myelogenous leukaemia in the chronic phase. Target Oncol. 2017;12(6):827–32. https://doi.org/10.1007/s11523-017-0521-6.
Weatherald J, Chaumais M-C, Savale L, Jaïs X, Seferian A, Canuet M, et al. Long-term outcomes of dasatinib-induced pulmonary arterial hypertension: a population-based study. Eur Respir J. 2017;50(1):1700217. https://doi.org/10.1183/13993003.00217-2017.
Minson AG, Cummins K, Fox L, Costello B, Yeung D, Cleary R, et al. The natural history of vascular and other complications in patients treated with nilotinib for chronic myeloid leukemia. Blood Adv. 2019;3(7):1084–91. https://doi.org/10.1182/bloodadvances.2018028035.
Caocci G, Mulas O, Annunziata M, Luciano L, Abruzzese E, Bonifacio M, et al. Long-term mortality rate for cardiovascular disease in 656 chronic myeloid leukaemia patients treated with second- and third-generation tyrosine kinase inhibitors. Int J Cardiol. 2020;301:163–6. https://doi.org/10.1016/j.ijcard.2019.10.036.
Jain P, Kantarjian H, Boddu PC, Nogueras-González GM, Verstovsek S, Garcia-Manero G, et al. Analysis of cardiovascular and arteriothrombotic adverse events in chronic-phase CML patients after frontline TKIs. Blood Adv. 2019;3(6):851–61. https://doi.org/10.1182/bloodadvances.2018025874.
Chen MH, Kerkela R, Force T. Mechanisms of cardiac dysfunction associated with tyrosine kinase inhibitor cancer therapeutics. Circulation. 2008;118(1):84–95. https://doi.org/10.1161/CIRCULATIONAHA.108.776831.
Efficace F, Baccarani M, Breccia M, Alimena G, Rosti G, Cottone F, et al. Health-related quality of life in chronic myeloid leukemia patients receiving long-term therapy with imatinib compared with the general population. Blood. 2011;118(17):4554–60. https://doi.org/10.1182/blood-2011-04-347575.
Efficace F, Cannella L. The value of quality of life assessment in chronic myeloid leukemia patients receiving tyrosine kinase inhibitors. Hematol Am Soc Hematol Educ Program. 2016;1:170–9. https://doi.org/10.1182/asheducation-2016.1.170.
Efficace F, Cardoni A, Cottone F, Vignetti M, Mandelli F. Tyrosine-kinase inhibitors and patient-reported outcomes in chronic myeloid leukemia: a systematic review. Leuk Res. 2013;37(2):206–13. https://doi.org/10.1016/j.leukres.2012.10.021.
Hewison A, Atkin K, McCaughan D, Roman E, Smith A, Smith G, et al. Experiences of living with chronic myeloid leukaemia and adhering to tyrosine kinase inhibitors: a thematic synthesis of qualitative studies. Eur J Oncol Nurs. 2020;45:101730. https://doi.org/10.1016/j.ejon.2020.101730.
Children’s Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers, Version 5.0 (2018). Available at: http://survivorshipguidelines.org/. Accessed 7/2/2020.
International Late Effects of Childhood Cancer Guideline Harmonization Group Guidelines. Available at: https://www.ighg.org/guidelines/topics/. Accessed 8/7/2020.
Smith G, Apperley J, Milojkovic D, Cross NCP, Foroni L, Byrne J, et al. A British Society for Haematology Guideline on the diagnosis and management of chronic myeloid leukaemia. Br J Haematol. 2020. https://doi.org/10.1111/bjh.16971.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Stephanie M. Smith and Kathleen M. Sakamoto declare no conflict of interest. Nobuko Hijiya has served on data and safety monitoring boards (DSMB) for Novartis and Incyte Corporation.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Oncology
Rights and permissions
About this article
Cite this article
Smith, S.M., Hijiya, N. & Sakamoto, K.M. Chronic Myelogenous Leukemia in Childhood. Curr Oncol Rep 23, 40 (2021). https://doi.org/10.1007/s11912-021-01025-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s11912-021-01025-x