Abstract
Purpose of Review
Apraxia of speech (AOS) is a motor speech disorder that has long been recognized to occur secondary to acute neurologic insults and, more recently, to neurodegenerative diseases as a harbinger for progressive supranuclear palsy and corticobasal syndrome. This article reviews recent findings regarding the clinic phenotypes of AOS, neuroimaging correlates, and the underlying disease processes.
Recent Findings
Two clinical subtypes of AOS map onto two underlying 4-repeat tauopathies. New imaging techniques have recently been applied to the study of progressive AOS. There is no data on the impact of behavioral intervention, although studies of nonfluent/agrammatic primary progressive aphasia that include patients with AOS suggest some benefit in speech intelligibility and maintenance.
Summary
While recent findings suggest subtypes of AOS exist that are linked to molecular pathology and have important implications for disease progression, further research is needed to assess outcome of behavioral and other types of intervention.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Allison KM, Cordella C, Iuzzini-Seigel J, Green JR. Differential diagnosis of apraxia of speech in children and adults: a scoping review. J Speech Lang Hear Res. 2020;63:2952–94.
Josephs KA, Duffy JR, Strand EA, Machulda MM, Senjem ML, Master AV, Lowe VJ, Jack CR Jr, Whitwell JL. Characterizing a neurodegenerative syndrome: primary progressive apraxia of speech. Brain. 2012;135:1522–36.
Josephs KA, Duffy JR, Strand EA, Machulda MM, Senjem ML, Lowe VJ, Jack CR, Whitwell JL. Syndromes dominated by apraxia of speech show distinct characteristics from agrammatic PPA. Neurology. 2013;81:337–45.
Gorno-Tempini M, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SE, Manes F. Classification of primary progressive aphasia and its variants. Neurology. 2011;76:1006–14.
•• Bouvier L, Monetta L, Laforce R Jr, Vitali P, Bocti C, Martel-Sauvageau V. Progressive apraxia of speech in Quebec French speakers: a case series. Int J Lang Commun Disord. 2021;56:528–48. The authors report a relatively large series of patients with PAOS and PPAOS in French speakers from Quebec demonstrating that these syndromic diagnoses are not limited to English speakers.
Bouvier L, Monetta L, Vitali P, Laforce R Jr, Martel-Sauvageau V. A preliminary look into the clinical evolution of motor speech characteristics in primary progressive apraxia of speech in Québec French. Am J Speech Lang Pathol. 2021;30:1459–76.
Duffy J. Apraxia of speech in degenerative neurologic disease. Aphasiology. 2006;20(6):511–27.
Duffy JR, Strand EA, Clark H, Machulda M, Whitwell JL, Josephs KA. Primary progressive apraxia of speech: clinical features and acoustic and neurologic correlates. Am J Speech Lang Pathol. 2015;24:88–100.
Poole ML, Brodtmann A, Darby D, Vogel AP. Motor speech phenotypes of frontotemporal dementia, primary progressive aphasia, and progressive apraxia of speech. J Speech Lang Hear Res. 2017;60:897–911.
Botha H, Duffy JR, Whitwell JL, et al. Classification and clinicoradiologic features of primary progressive aphasia (PPA) and apraxia of speech. Cortex. 2015;69:220–36.
Botha H, Utianski RL, Whitwell JL, et al. Disrupted functional connectivity in primary progressive apraxia of speech. Neuroimage Clin. 2018;18:617–29.
Utianski RL, Duffy JR, Clark HM, et al. Prosodic and phonetic subtypes of primary progressive apraxia of speech. Brain Lang. 2018;184:54–65.
Whitwell JL, Duffy JR, Strand EA, Machulda MM, Senjem ML, Gunter JL, Kantarci K, Eggers SD, Jack CR, Josephs KA. Neuroimaging comparison of primary progressive apraxia of speech and progressive supranuclear palsy. Eur J Neurol. 2013;20:629–37.
Josephs KA, Duffy JR, Strand E, et al. Clinicopathological and imaging correlates of progressive aphasia and apraxia of speech. Brain. 2006;129:1385–98.
Josephs KA, Duffy JR, Fossett TR, et al. Fluorodeoxyglucose f18 positron emission tomography in progressive apraxia of speech and primary progressive aphasia variants. Arch Neurol. 2010;67:596–605.
Seckin ZI, Whitwell JL, Utianski RL, et al. Ioflupane 123I (DAT scan) SPECT identifies dopamine receptor dysfunction early in the disease course in progressive apraxia of speech. J Neurol. 2020;267:2603–11.
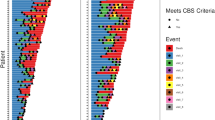
•• Josephs KA, Duffy JR, Clark HM, et al. A molecular pathology, neurobiology, biochemical, genetic and neuroimaging study of progressive apraxia of speech. Nat Commun. 2021;12:3452. The authors identified an association between phonetic AOS and corticobasal degeneration pathology, and between prosodic AOS and progressive supranuclear palsy pathology highlighting the importance of subtyping AOS.
Utianski RL, Whitwell JL, Schwarz CG, et al. Tau-PET imaging with [18F]AV-1451 in primary progressive apraxia of speech. Cortex. 2018;99:358–74.
Josephs KA, Duffy JR, Strand EA, et al. The evolution of primary progressive apraxia of speech. Brain. 2014;137:2783–95.
Seckin ZI, Duffy JR, Strand EA, et al. The evolution of parkinsonism in primary progressive apraxia of speech: a 6-year longitudinal study. Parkinsonism Relat Disord. 2020;81:34–40.
Whitwell JL, Duffy JR, Machulda MM, et al. Tracking the development of agrammatic aphasia: a tensor-based morphometry study. Cortex. 2017;90:138–48.
Whitwell JL, Weigand S, Duffy J, Clark H, Strand E, Machulda M, Spychalla A, Senjem M, Jack CR, Josephs KA. Predicting clinical decline in progressive agrammatic aphasia and apraxia of speech. Neurology. 2017;89:2271–9.
Utianski RL, Duffy JR, Clark HM, Strand EA, Boland SM, Machulda MM, Whitwell JL, Josephs KA. Clinical progression in four cases of primary progressive apraxia of speech. Am J Speech Lang Pathol. 2021;27:1303–18.
Duffy JR, Utianski RL, Josephs KA. Primary progressive apraxia of speech: from recognition to diagnosis and care. Aphasiology. 2021;35:560–91.
Botha H, Josephs KA. Primary progressive aphasias and apraxia of speech. Contin Lifelong Learn Neurol. 2019;25:101.
Duffy JR, Martin PR, Clark HM, Utianski RL, Strand EA, Whitwell JL, Josephs KA. The apraxia of speech rating scale: reliability, validity, and utility. Am J Speech Lang Pathol. 2023;32(2):469–91.
Duffy JR. Motor speech disorders: substrates, differential diagnosis, and management, 4e. St. Louis: Mosby; 2020.
Utianski RL. Primary progressive aphasia and other frontotemporal dementias: diagnosis and treatment of associated communication disorders. 1e. San Diego: Plural Publishing Inc; 2019.
Mailend ML, Maas E. To lump or to split? Possible subtypes of apraxia of speech. Aphasiology. 2020;35:592–613.
Takakura Y, Otsuki M, Sakai S, et al. Sub-classification of apraxia of speech in patients with cerebrovascular and neurodegenerative diseases. Brain Cogn. 2019;130:1–10.
Botha H, Duffy JR, Strand EA, Machulda MM, Whitwell JL, Josephs KA. Nonverbal oral apraxia in primary progressive aphasia and apraxia of speech. Neurology. 2014;82:1729–35.
Morihara K, Ota S, Kakinuma K, Kawakami N, Higashiyama Y, Kanno S, Tanaka F, Suzuki K. Buccofacial apraxia in primary progressive aphasia. Cortex. 2023;158:61–70.
Duffy JR, Strand EA, Josephs KA. Motor speech disorders associated with primary progressive aphasia. Aphasiology. 2014;28:1004–17.
Ash S, McMillan C, Gunawardena D, Avants B, Morgan B, Khan A, Moore P, Gee J, Grossman M. Speech errors in progressive non-fluent aphasia. Brain Lang. 2010;113:13–20.
Croot K, Ballard K, Leyton CE, Hodges JR. Apraxia of speech and phonological errors in the diagnosis of nonfluent/agrammatic and logopenic variants of primary progressive aphasia. J Speech Lang Hear Res. 2012;55:S1562–72.
Scheffel L, Duffy JR, Strand EA, Josephs KA. Word fluency test performance in primary progressive aphasia and primary progressive apraxia of speech. Am J Speech Lang Pathol. 2021;30:2635–42.
Polsinelli AJ, Machulda MM, Martin PR, et al. Neuropsychological profiles of patients with progressive apraxia of speech and aphasia. J Int Neuropsychol Soc. 2022;28(5):441–51.
Valls Carbo A, Reid RI, Tosakulwong N, et al. Tractography of supplementary motor area projections in progressive speech apraxia and aphasia. NeuroImage Clin. 2022;34:102999.
Whitwell JL, Stevens CA, Duffy JR, et al. An evaluation of the progressive supranuclear palsy speech/language variant. Mov Disord Clin Pract. 2019;6:452–61.
•• Whitwell JL, Martin P, Duffy JR, Clark HM, Utianski RL, Botha H, Machulda MM, Strand EA, Josephs KA. Survival analysis in primary progressive apraxia of speech and agrammatic aphasia. Neurol Clin Pract. 2021;11:249–55. The authors found evidence for patients with PPAOS to have better survival compared to patients with PAOS (i.e., having aphasia) highlighting the importance of distinguishing PPAOS from PPA.
Armstrong MJ, Litvan I, Lang AE, Bak TH, Bhatia KP, Borroni B, et al. Criteria for the diagnosis of corticobasal degeneration. Neurology. 2013;80:496–503.
Hokelekli FO, Duffy JR, Clark HM, et al. Autopsy validation of progressive supranuclear palsy-predominant speech/language disorder criteria. Mov Disord Off J Mov Disord Soc. 2022;37:213–8.
Hokelekli FO, Ali F, Carlos AF, et al. Sleep disturbances in the speech-language variant of progressive supranuclear palsy. Parkinsonism Relat Disord. 2021;91:9–12.
Hokelekli FO, Duffy JR, Clark HM, Utianski RL, Botha H, Stierwalt JA, Strand EA, Machulda MM, Whitwell JL, Josephs KA. Cross-sectional and longitudinal assessment of behavior in primary progressive apraxia of speech and agrammatic aphasia. Dement Geriatr Cogn Disord. 2022;51:193–202.
Robinson CG, Duffy JR, Clark HA, et al. Clinicopathological associations of hemispheric dominance in primary progressive apraxia of speech. Eur J Neurol. 2023;30:1209–19.
Tetzloff KA, Duffy JR, Strand EA, et al. Clinical and imaging progression over 10 years in a patient with primary progressive apraxia of speech and autopsy-confirmed corticobasal degeneration. Neurocase. 2018;24:111–20.
Josephs KA, Duffy JR, Strand EA, Machulda MM, Senjem ML, Lowe VJ, Jack CR, Whitwell JL. APOE ε4 influences β-amyloid deposition in primary progressive aphasia and speech apraxia. Alzheimers Dement. 2014;10:630–6.
Lowe V, Curran G, Fang P, et al. An autoradiographic evaluation of AV-1451 Tau PET in dementia. Acta Neuropathol Commun. 2016;4:58.
Whitwell JL, Höglinger GU, Antonini A, et al. Radiological biomarkers for diagnosis in PSP: where are we and where do we need to be? Mov Disord Off J Mov Disord Soc. 2017;32:955–71.
Sintini I, Duffy JR, Clark HM, et al. Functional connectivity to the premotor cortex maps onto longitudinal brain neurodegeneration in progressive apraxia of speech. Neurobiol Aging. 2022;120:105–16.
Satoh R, Arani A, Senjem ML, et al. Spatial patterns of elevated magnetic susceptibility in progressive apraxia of speech. NeuroImage Clin. 2023;38:103394.
Sjöström H, Granberg T, Westman E, Svenningsson P. Quantitative susceptibility mapping differentiates between parkinsonian disorders. Parkinsonism Relat Disord. 2017;44:51–7.
Josephs KA, Boeve B, Duffy J, Smith G, Knopman D, Parisi J, Petersen R, Dickson D (2005) Atypical progressive supranuclear palsy underlying progressive apraxia of speech and nonfluent aphasia. Neurocase 283–296
Buciuc M, Koga S, Pham NTT, et al. The many faces of globular glial tauopathy: a clinical and imaging study. Eur J Neurol. 2023;30:321–33.
Flanagan EP, Baker MC, Perkerson RB, Duffy JR, Strand EA, Whitwell JL, Machulda MM, Rademakers R, Josephs KA. Dominant frontotemporal dementia mutations in 140 cases of primary progressive aphasia and speech apraxia. Dement Geriatr Cogn Disord. 2015;39:281–6.
Henry ML, Hubbard HI, Grasso SM, et al. Retraining speech production and fluency in non-fluent/agrammatic primary progressive aphasia. Brain. 2018;141:1799–814.
• Themistocleous C, Webster K, Tsapkini K. Effects of tDCS on sound duration in patients with apraxia of speech in primary progressive aphasia. Brain Sci. 2021;11:335. The authors provide some evidence for transcranial direct current stimulation to be beneficial to maximizing the efficacy of speech therapy in patients with PAOS.
Shpiner DS, McInerney KF, Miller M, Allen J, Rice J, Luca CC, Adams D, Gomes-Osman J. High frequency repetitive transcranial magnetic stimulation for primary progressive apraxia of speech: a case series. Brain Stimulat. 2019;12:1581–2.
Strand EA, Duffy JR, Clark HM, Josephs KA. The apraxia of speech rating scale: a new tool for diagnosis and description of AOS. J Commun Disord. 2014;51:43–50.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Utianski, R.L., Josephs, K.A. An Update on Apraxia of Speech. Curr Neurol Neurosci Rep 23, 353–359 (2023). https://doi.org/10.1007/s11910-023-01275-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-023-01275-1