Abstract
Purpose of Review
At any point in time, there are hundreds of armed conflicts throughout the world. Neuropsychological disorders are a major cause of morbidity during and after armed conflicts. Conditions such as closed and open head injuries, acute stress disorder, post-traumatic stress disorder, depression, anxiety, and psychosis are prevalent among survivors. Herein, we summarize information on the various forms of torture, the resultant neuropsychological pathology, and treatment strategies to help survivors.
Recent Findings
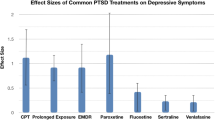
Strategies to address the needs of individuals who experienced neuropsychological trauma due to armed conflicts and torture include pharmacological and psychological interventions. The former includes antidepressant, antianxiety, and antipsychotic medications. The latter includes narrative exposure therapy and trauma-focused cognitive-behavioral therapy.
Summary
Neuropsychological disorders are major causes of morbidity among survivors of armed conflicts and torture. Treatment strategies must be affordable, applicable across cultures, and deliverable by individuals who understand the victims’ psychosocial and ethnic background.
Similar content being viewed by others
References
Papers of the particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wars in the World. List of ongoing conflicts. 2017. Accessed at https://www.warsintheworld.com/?page=static1258254223
• Jaung M, Jani S, Banu S, Mackey JM. International Emergency Psychiatry challenges: disaster medicine, war, human trafficking, displaced persons. Psychiatr Clin North Am. 2017;40(3):565–74. https://doi.org/10.1016/j.psc.2017.05.015. Neuropsychological disorders are major causes of morbidity among survivors of armed conflicts and torture. Treatment strategies must be affordable, applicable across cultures, community-based, and deliverable by individuals who understand the victims’ psychosocial and ethnic background
American Psychiatric Association. Diagnostic and statistical manual of mental disorders DSM-5. 5th ed. ed. Washington, D.C. 2013.
Ba I, Bhopal RS. Physical, mental and social consequences in civilians who have experienced war-related sexual violence: a systematic review (1981-2014). Public Health. 2017;142:121–35. https://doi.org/10.1016/j.puhe.2016.07.019.
Hirani K, Payne D, Mutch R, Cherian S. Health of adolescent refugees resettling in high-income countries. Arch Dis Child. 2016;101(7):670–6. https://doi.org/10.1136/archdischild-2014-307221.
United Nations High Commissioner for Refugees (UNHCR). Global Trends Forced Displacement in 2016. Geneva, Switzerland. 2017.
United Nations General Assembly. Convention against torture and other cruel, inhuman or degrading treatment or punishment: Resolution 39/46 1984.
United Nations High Commissioner for Refugees (UNHCR). Strengthening refugee resettlement and other pathways to admission and solutions 2016.
Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. Lancet. 2005;365(9467):1309–14. https://doi.org/10.1016/s0140-6736(05)61027-6.
Giacco D, Laxhman N, Priebe S. Prevalence of and risk factors for mental disorders in refugees. Semin Cell Dev Biol. 2017; https://doi.org/10.1016/j.semcdb.2017.11.030.
Member Centers of the National Consortium of Torture Treatment Programs (NCTTP). Descriptive, inferential, functional outcome data on 9,025 torture survivors over six years in the United States. Torture. 2015;25(12):34–60.
Bogic M, Njoku A, Priebe S. Long-term mental health of war-refugees: a systematic literature review. BMC Int Health Hum Rights 2015;15. doi:https://doi.org/10.1186/s12914-015-0064-9, 1.
Patel V, Chisholm D, Parikh R, Charlson F, Degenhardt L, Dua T, et al. Addressing the burden of mental, neurological, and substance use disorders: key messages from disease control priorities, 3rd edition. Lancet. 2016;387(10028):1672–85. https://doi.org/10.1016/S0140-6736(15)00390-6.
Steel Z, Chey T, Silove D, Marnane C, Bryant R, van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement. JAMA. 2009;302(5):537–49. https://doi.org/10.1001/jama.2009.1132.
Pham P, Vinck P, Stover E. Returning home: forced conscription, reintegration, and mental health status of former abductees of the Lord's Resistance Army in northern Uganda. BMC Psychiatry. 2009;9(1):23. https://doi.org/10.1186/1471-244X-9-23.
• Zandieh S, Bernt R, Knoll P, Wenzel T, Hittmair K, Haller J, et al. Analysis of the metabolic and structural brain changes in patients with torture-related post-traumatic stress disorder (TR-PTSD) using (1)(8)F-FDG PET and MRI. Medicine. 2016;95(15):e3387. https://doi.org/10.1097/MD.0000000000003387. In this observational study, the authors analyzed brain structures with magnetic resonance imaging and positron emission tomography in patients with torture-related PTSD and healthy controls. Results suggested metabolic and structural changes in patients with torture-related PTSD
Vindevogel S, Coppens K, Derluyn I, De Schryver M, Loots G, et al. Forced conscription of children during armed conflict: experiences of former child soliders in northern Uganda. Child Abuse Negl. 2011;35:551–62. https://doi.org/10.1016/j.chiabu.2011.03.011.
O'connor M. Sexual violence in armed conflict: the least condemned of war crimes. J Law Med. 2014;21(3):528–42.
Moore M, Barner J. Sexual minorities in conflict zones: a review of the literature. Aggress Violent Behav. 2017;35:33–7. https://doi.org/10.1016/j.avb.2017.06.006.
Stevens A. The invisible soldiers: understand how the life experiences of girl child soldiers impacts upon their health and rehabilitaiton needs. Arch Dis Child. 2014;99(5):458–62. https://doi.org/10.1136/archdischild-2013-305240.
•• Perez-Sales P, Navarro-Lashayas MA, Plaza A, Morentin B, Salinas OB. Incommunicado detention and torture in Spain, part III: 'Five days is enough': the concept of torturing environments. Torture. 2016;26(3):21–33. The authors describe torturing environments and the psychological methods of torture in victims of incommunicado detention in Spain. Western civilizations have increasingly adopted psychological torture methods
Gudjonsson GH. The psychology of interrogations and confessions: a handbook. Wiley & Sons, Ltd: England; 2003.
Istanbul Protocol Project in the Basque Country Working Group. Incommunicado detention and torture in Spain, part I: the Istanbul Protocol Project in the Basque Country. Torture. 2016;26(3):3.
Johnson H, Thompson A. The development and maintenance of post-traumatic stress disorder (PTSD) in civilian adult survivors of war trauma and torture: a review. Clin Psychol Rev. 2008;28(1):36–47. https://doi.org/10.1016/j.cpr.2007.01.017.
Bryant RA, Harvey AG. Acute stress disorder: a handbook of theory, assessment, and treatment. Washington DC: American Psychological Association; 2000.
•• Navarro-Lashayas MA, Perez-Sales P, Lopez-Neyra G, Martinez MA, Morentin B. Incommunicado detention and torture in Spain, Part IV: Psychological and psychiatric consequences of ill-treatment and torture: trauma and human worldviews. Torture. 2016;26(3):34–45. The authors report on the enduring psychological effects (PTSD, depressive disorder, anxiety, personality changes) of short-term incommunicado detention in Spain
Mollica RF, Brooks R, Tor S, Lopes-Cardozo B, Silove D. The enduring mental health impact of mass violence: a community comparison study of Cambodian civilians living in Cambodia and Thailand. Int J Soc Psychiatry. 2014;60(1):6–20. https://doi.org/10.1177/0020764012471597.
•• Nygaard M, Sonne C, Carlsson J. Secondary Psychotic features in refugees diagnosed with post-traumatic stress disorder: a retrospective cohort study. BMC Psychiatry. 2017;17(1):5. https://doi.org/10.1186/s12888-016-1166-1. The authors conducted a retrospective cohort study in refugees with PTSD and revealed that 40% had secondary psychotic features. Patients with psychotic features were more likely to having had experienced torture and imprisonment
Jenewein J, Erni J, Moergeli H, Grillon C, Schumacher S, Mueller-Pfeiffer C, et al. Altered pain perception and fear-learning deficits in subjects with posttraumatic stress disorder. J Pain. 2016;17(12):1325–33. https://doi.org/10.1016/j.jpain.2016.09.002.
Tsur N, Defrin R, Ginzburg K. Posttraumatic stress disorder, orientation to pain, and pain perception in ex-prisoners of war who underwent torture. Psychosom Med. 2017;79(6):655–63. https://doi.org/10.1097/psy.0000000000000461.
Tsur N, Shahar G, Defrin R, Lahav Y, Ginzburg K. Torturing personification of chronic pain among torture survivors. J Psychosom Res. 2017;99:155–61. https://doi.org/10.1016/j.jpsychores.2017.06.016.
•• Slobodin O, de Jong J. Mental health interventions for traumatized asylum seekers and refugees: what do we know about their efficacy? Int J Soc Psychiatry. 2015;61:17–26. https://doi.org/10.1177/0020764014535752. In this review, the authors highlight the shortage of guiding frameworks available to investigators and clinicians who are interested in tailoring interventions to work with refugees and asylum seekers. The authors discuss theoretical, ethical, and methodological considerations for future research
• Patel N, Kellezi B, Williams AC. Psychological, social and welfare interventions for psychological health and well-being of torture survivors. Cochrane Database Syst Rev. 2014(11):CD009317. doi: 10.1002/14651858.CD009317.pub2. Health and welfare agencies offer varied rehabilitation services to survivors of torture. These include conventional mental health treatment and needs-based interventions. Narrative exposure therapy and trauma-focused cognitive-behavioral therapy have been found to confer at least moderate benefits in reducing distress and symptoms of PTSD.
Gwozdziewycz N, Mehl-Madrona L. Meta-analysis of the use of narrative exposure therapy for the effects of trauma among refugee populations. Perm J. 2013;17(1):70–6. https://doi.org/10.7812/TPP/12-058.
Deblinger E, Pollio E, Dorsey S. Applying trauma-focused cognitive-behavioral therapy in group format. Child Maltreat. 2016;21:59–73. https://doi.org/10.1177/1077559515620668.
de Arellano M, Lyman D, Jobe-Shields L, George P, Dougherty R, Daniels A, et al. Trauma-focused cognitive-behavioral therapy for children and adolescents: assessing the evidence. Psychiatr Serv. 2014;65(5):591–602. https://doi.org/10.1176/appi.ps.201300255.
Visser E, Gosens T, Den Oudsten BL, De Vries J. The course, prediction, and treatment of acute and posttraumatic stress in trauma patients. J Trauma Acute Care Surg. 2017;82(6):1158–83. https://doi.org/10.1097/ta.0000000000001447.
Acknowledgements
The authors wish to acknowledge the invaluable assistance of Stephanie Schulte.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Pedro Weisleder and Caitlin Rublee declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Neurology of Systemic Diseases
Rights and permissions
About this article
Cite this article
Weisleder, P., Rublee, C. The Neuropsychological Consequences of Armed Conflicts and Torture. Curr Neurol Neurosci Rep 18, 9 (2018). https://doi.org/10.1007/s11910-018-0818-6
Published:
DOI: https://doi.org/10.1007/s11910-018-0818-6