Abstract
Purpose of Review
Predicting whether a hospitalized patient is infected with an ESBL-E or CRE remains challenging and often leads to overutilization of broad-spectrum antibiotics. This review will describe the most common risk factors associated with ESBL-E and CRE infections and how to best apply them to clinical practice. A review of existing risk scoring tools to predict multidrug-resistant gram-negative pathogens (MDR GN) as well as considerations for implementation will be discussed.
Recent Findings
Prior use of a fluoroquinolone or broad-spectrum beta-lactam with the past 3 months, history of colonization or infection with an ESBL-E or CRE within the past year, presence of an indwelling device, and transfer from a long-term care facility are four shared risk factors for ESBL-E and CRE and should be considered when selecting empiric antimicrobial therapy. Adoption of a risk scoring tool can also help clinicians determine appropriate empiric antimicrobial therapy if appropriately validated against local data.
Summary
Identifying individual risk factors for MDR GN and utilization of risk scoring systems are valuable tools to optimize empiric antibiotic decision-making.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Nelson RE, Hatfield KM, Wolford H, Samore MH, Scott RD II, Reddy SC, et al. National estimates of healthcare costs associated with multidrug-resistant bacterial infections among hospitalized patients in the United States. Clin Infect Dis. 2021;72(Supplement_1):S17–26.
Cassini A, Högberg LD, Plachouras D, Quattrocchi A, Hoxha A, Simonsen GS, et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: a population-level modelling analysis. Lancet Infect Dis. 2019;19(1):56–66.
CDC. Antibiotic-resistant germs: new threats [Internet]. Centers for Disease Control and Prevention. 2021 [cited 2021 Nov 26]. Available from: https://www.cdc.gov/drugresistance/biggest-threats.html.
Wunderink RG, Srinivasan A, Barie PS, Chastre J, Dela Cruz CS, Douglas IS, et al. Antibiotic stewardship in the intensive care unit. An Official American Thoracic Society Workshop Report in Collaboration with the AACN, CHEST, CDC, and SCCM. Ann Am Thorac Soc. 2020;17(5):531–40.
Teshome BF, Vouri SM, Hampton N, Kollef MH, Micek ST. Duration of exposure to antipseudomonal β-lactam antibiotics in the critically ill and development of new resistance. Pharmacother J Hum Pharmacol Drug Ther. 2019;39(3):261–70.
Kollef MH, Sherman G, Ward S, Fraser VJ. Inadequate antimicrobial treatment of infections: a risk factor for hospital mortality among critically ill patients. Chest. 1999;115(2):462–74.
Kollef MH. Broad-spectrum antimicrobials and the treatment of serious bacterial infections: getting it right up front. Clin Infect Dis Off Publ Infect Dis Soc Am. 2008;15(47 Suppl 1):S3-13.
Pogue JM, Kaye KS, Veve MP, Patel TS, Gerlach AT, Davis SL, et al. Ceftolozane/tazobactam vs polymyxin or aminoglycoside-based regimens for the treatment of drug-resistant Pseudomonas aeruginosa. Clin Infect Dis Off Publ Infect Dis Soc Am. 2020;71(2):304–10.
Sullivan KV, Morgan DJ, Leekha S. Use of diagnostic stewardship practices to improve urine culturing among SHEA Research Network hospitals. Infect Control Hosp Epidemiol. 2018;7:1–4.
Pogue JM, Heil EL, Lephart P, Johnson JK, Mynatt RP, Salimnia H, et al. An antibiotic stewardship program blueprint for optimizing verigene BC-GN within an institution: a tale of two cities. Antimicrob Agents Chemother. 2018;62(5):e02538-e2617.
Kaye KS, Pogue JM. Infections caused by resistant gram-negative bacteria: epidemiology and management. Pharmacother J Hum Pharmacol Drug Ther. 2015;35(10):949–62.
Palacios-Baena ZR, Giannella M, Manissero D, Rodríguez-Baño J, Viale P, Lopes S, et al. Risk factors for carbapenem-resistant Gram-negative bacterial infections: a systematic review. Clin Microbiol Infect. 2021;27(2):228–35.
•• Burillo A, Muñoz P, Bouza E. Risk stratification for multidrug-resistant Gram-negative infections in ICU patients. Curr Opin Infect Dis. 2019;32(6):626–37. Burillo et al. summarize a series of scoring tools for multidrug-resistant gram-negative pathogens for adult ICU patients that have been published up to 2019 and evaluate risk factors for MDR GN.
Langdon A, Crook N, Dantas G. The effects of antibiotics on the microbiome throughout development and alternative approaches for therapeutic modulation. Genome Med. 2016;13(8):39.
MacAdam H, Zaoutis TE, Gasink LB, Bilker WB, Lautenbach E. Investigating the association between antibiotic use and antibiotic resistance: impact of different methods of categorising prior antibiotic use. Int J Antimicrob Agents. 2006;28(4):325–32.
Hyle EP, Bilker WB, Gasink LB, Lautenbach E. Impact of different methods for describing the extent of prior antibiotic exposure on the association between antibiotic use and antibiotic-resistant infection. Infect Control Hosp Epidemiol. 2007;28(6):647–54.
Augustine MR, Testerman TL, Justo JA, Bookstaver PB, Kohn J, Albrecht H, et al. Clinical risk score for prediction of extended-spectrum β-Lactamase-producing Enterobacteriaceae in bloodstream isolates. Infect Control Hosp Epidemiol. 2017;38(3):266–72.
Goodman KE, Lessler J, Cosgrove SE, Harris AD, Lautenbach E, Han JH, et al. A clinical decision tree to predict whether a bacteremic patient is infected with an extended-spectrum β-lactamase-producing organism. Clin Infect Dis Off Publ Infect Dis Soc Am. 2016;63(7):896–903.
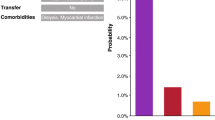
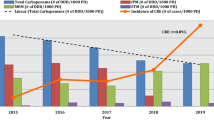
•• Lodise TP, Bonine NG, Ye JM, Folse HJ, Gillard P. Development of a bedside tool to predict the probability of drug-resistant pathogens among hospitalized adult patients with gram-negative infections. BMC Infect Dis. 2019;19(1):718. The authors created a clinical bedside prediction tool for 3GC, CRE, and MRDP infections in hospitalized adult patients and identified prior antibiotic use, infection during prior three months, and hospital prevalence of resistant organisms as key predictors for subsequent infection with the included MDR GN.
Chopra T, Marchaim D, Johnson PC, Chalana IK, Tamam Z, Mohammed M, et al. Risk factors for bloodstream infection caused by extended-spectrum β-lactamase–producing Escherichia coli and Klebsiella pneumoniae: a focus on antimicrobials including cefepime. Am J Infect Control. 2015;43(7):719–23.
Johnson SW, Anderson DJ, May DB, Drew RH. Utility of a clinical risk factor scoring model in predicting infection with extended-spectrum β-lactamase-producing enterobacteriaceae on hospital admission. Infect Control Hosp Epidemiol. 2013;34(4):385–92.
Nakai H, Hagihara M, Kato H, Hirai J, Nishiyama N, Koizumi Y, et al. Prevalence and risk factors of infections caused by extended-spectrum β-lactamase (ESBL)-producing Enterobacteriaceae. J Infect Chemother. 2016;22(5):319–26.
van Loon K, Voor In ’t Holt AF, Vos MC. A systematic review and meta-analyses of the clinical epidemiology of carbapenem-resistant Enterobacteriaceae. Antimicrob Agents Chemother. 2018;62(1):e01730–17.
Zhang AR, Wang Q, Zhou CE, Zhang JG, Wang XJ, Zhao JK, et al. Risk factors and clinical prognosis analysis of carbapenem-resistant Enterobacterales bacteria nosocomial infection. Zhonghua Yi Xue Za Zhi. 2021;101(21):1572–82.
Kim YA, Lee SJ, Park YS, Lee YJ, Yeon JH, Seo YH, et al. Risk factors for carbapenemase-producing Enterobacterales infection or colonization in a Korean intensive care unit: a case–control study. Antibiotics. 2020;9(10):680.
Karanika S, Karantanos T, Arvanitis M, Grigoras C, Mylonakis E. Fecal colonization with extended-spectrum beta-lactamase-producing Enterobacteriaceae and risk factors among healthy individuals: a systematic review and metaanalysis. Clin Infect Dis Off Publ Infect Dis Soc Am. 2016;63(3):310–8.
Carlet J. The gut is the epicentre of antibiotic resistance. Antimicrob Resist Infect Control. 2012;27(1):39.
Harris AD, McGregor JC, Johnson JA, Strauss SM, Moore AC, Standiford HC, et al. Risk factors for colonization with extended-spectrum beta-lactamase-producing bacteria and intensive care unit admission. Emerg Infect Dis. 2007;13(8):1144–9.
Massart N, Camus C, Benezit F, Moriconi M, Fillatre P, Le Tulzo Y. Incidence and risk factors for acquired colonization and infection due to extended-spectrum beta-lactamase-producing Gram-negative bacilli: a retrospective analysis in three ICUs with low multidrug resistance rate. Eur J Clin Microbiol Infect Dis Off Publ Eur Soc Clin Microbiol. 2020;39(5):889–95.
Detsis M, Karanika S, Mylonakis E. ICU acquisition rate, risk factors, and clinical significance of digestive tract colonization with extended-spectrum beta-lactamase–producing Enterobacteriaceae: a systematic review and meta-analysis*. Crit Care Med. 2017;45(4):705–14.
Anesi JA, Lautenbach E, Tamma PD, Thom KA, Blumberg EA, Alby K, et al. Risk factors for extended-spectrum β-lactamase–producing Enterobacterales bloodstream infection among solid-organ transplant recipients. Clin Infect Dis. 2021;72(6):953–60.
Tischendorf J, de Avila RA, Safdar N. Risk of infection following colonization with carbapenem-resistant Enterobactericeae: a systematic review. Am J Infect Control. 2016;44(5):539–43.
Li Y, Shen H, Zhu C, Yu Y. Carbapenem-resistant Klebsiella pneumoniae Infections among ICU admission patients in Central China: prevalence and prediction model. BioMed Res Int. 2019;2019:9767313.
Vazquez-Guillamet MC, Vazquez R, Micek ST, Kollef MH. Predicting resistance to piperacillin-tazobactam, cefepime and meropenem in septic patients with bloodstream infection due to gram-negative bacteria. Clin Infect Dis Off Publ Infect Dis Soc Am. 2017;65(10):1607–14.
Rodríguez-Baño J, Navarro MD, Romero L, Muniain MA, de Cueto M, Gálvez J, et al. Risk-factors for emerging bloodstream infections caused by extended-spectrum β-lactamase-producing Escherichia coli. Clin Microbiol Infect. 2008;14(2):180–3.
Wu UI, Yang CS, Chen WC, Chen YC, Chang SC. Risk factors for bloodstream infections due to extended-spectrum beta-lactamase-producing Escherichia coli. J Microbiol Immunol Infect Wei Mian Yu Gan Ran Za Zhi. 2010;43(4):310–6.
Hayakawa K, Gattu S, Marchaim D, Bhargava A, Palla M, Alshabani K, et al. Epidemiology and risk factors for isolation of Escherichia coli producing CTX-M-type extended-spectrum β-lactamase in a large U.S. Medical Center. Antimicrob Agents Chemother. 2013;57(8):4010–8.
Pop-Vicas A, Mitchell SL, Kandel R, Schreiber R, D’Agata EMC. Multidrug-resistant gram-negative bacteria in a long-term care facility: prevalence and risk factors. J Am Geriatr Soc. 2008;56(7):1276–80.
FastStats [Internet]. 2022 [cited 2022 Feb 28]. Available from: https://www.cdc.gov/nchs/fastats/nursing-home-care.htm.
Jump RLP, Crnich CJ, Mody L, Bradley SF, Nicolle LE, Yoshikawa TT. Infectious diseases in older adults of long-term care facilities: update on approach to diagnosis and management. J Am Geriatr Soc. 2018;66(4):789–803.
Werner RM, Hoffman AK, Coe NB. Long-term care policy after Covid-19 — solving the nursing home crisis. N Engl J Med. 2020;383(10):903–5.
Rodríguez-Villodres Á, Martín-Gandul C, Peñalva G, Guisado-Gil AB, Crespo-Rivas JC, Pachón-Ibáñez ME, et al. Prevalence and Risk factors for multidrug-resistant organisms colonization in long-term care facilities around the world: a review. Antibiotics. 2021;10(6):680.
Flokas ME, Alevizakos M, Shehadeh F, Andreatos N, Mylonakis E. Extended-spectrum β-lactamase-producing Enterobacteriaceae colonisation in long-term care facilities: a systematic review and meta-analysis. Int J Antimicrob Agents. 2017;50(5):649–56.
Chen HY, Jean SS, Lee YL, Lu MC, Ko WC, Liu PY, et al. Carbapenem-resistant Enterobacterales in long-term care facilities: a global and narrative review. Front Cell Infect Microbiol. 2021;11: 601968.
Xiao T, Wu Z, Shi Q, Zhang X, Zhou Y, Yu X, et al. A retrospective analysis of risk factors and outcomes in patients with extended-spectrum beta-lactamase-producing Escherichia coli bloodstream infections. J Glob Antimicrob Resist. 2019;1(17):147–56.
•• Mohd Sazlly Lim S, Wong PL, Sulaiman H, Atiya N, Hisham Shunmugam R, Liew SM. Clinical prediction models for ESBL-Enterobacteriaceae colonization or infection: a systematic review. J Hosp Infect. 2019 May;102(1):8–16. Mohd Sazlly Lim and colleagues critically evaluate existing risk scoring tools to predict ESBL-E infections or colonization and current barriers to implementation in a clinical setting.
Steyerberg EW, Harrell FE, Borsboom GJ, Eijkemans MJ, Vergouwe Y, Habbema JD. Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J Clin Epidemiol. 2001;54(8):774–81.
Steyerberg EW, Bleeker SE, Moll HA, Grobbee DE, Moons KGM. Internal and external validation of predictive models: a simulation study of bias and precision in small samples. J Clin Epidemiol. 2003;56(5):441–7.
Sonti R, Conroy ME, Welt EM, Hu Y, Luta G, Jamieson DB. Modeling risk for developing drug resistant bacterial infections in an MDR-naive critically ill population. Ther Adv Infect Dis. 2017 Jul;4(4):95–103.
Sick-Samuels AC, Goodman KE, Rapsinski G, Colantouni E, Milstone AM, Nowalk AJ, et al. A decision tree using patient characteristics to predict resistance to commonly used broad-spectrum antibiotics in children with gram-negative bloodstream infections. J Pediatr Infect Dis Soc. 2020 Apr 30;9(2):142–9.
Cwengros LN, Mynatt RP, Timbrook TT, Mitchell R, Salimnia H, Lephart P, et al. Minimizing time to optimal antimicrobial therapy for enterobacteriaceae bloodstream infections: A retrospective, hypothetical application of predictive scoring tools vs rapid diagnostics tests. Open Forum Infect Dis. 2020 Aug 1;7(8):ofaa278.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs. Li and Heil declare that they have no conflicts of interest. Dr. Claeys reports Advisory Board membership for La Jolla Therapeutics, AbbVie Biotherapeutics, and Melinta Therapeutics, has served on the Speakers Bureau for BioFire Diagnostics, and has received grants from Merck and Co, outside the submitted work. Dr. Justo reports personal fees from bioMerieux, Merck, Spero Therapeutics, Entasis Therapeutics, Therapeutic Research Center, and Shionogi, outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Healthcare Associated Infections
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, C., Claeys, K.C., Justo, J.A. et al. No Crystal Ball? Using Risk Factors and Scoring Systems to Predict Extended-Spectrum Beta-Lactamase Producing Enterobacterales (ESBL-E) and Carbapenem-Resistant Enterobacterales (CRE) Infections. Curr Infect Dis Rep 24, 147–158 (2022). https://doi.org/10.1007/s11908-022-00785-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11908-022-00785-2