Abstract
Purpose of Review
Resistant gram-negative infections are becoming increasingly difficult to treat, prompting increased focus on drug development. This review will focus primarily on the new beta-lactam agents developed in the past 5 years that target multidrug-resistant (MDR) gram-negative organisms, including those producing carbapenemases.
Recent Findings
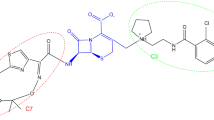
Four new agents including ceftazidime-avibactam (CAZ-AVI), meropenem-vaborbactam (MER-VAB), imipenem-relebactam (IMI-REL), and cefiderocol have recently been approved for the treatment of resistant gram-negative infections. CAZ-AVI remains an option for blaOXA-48–producing isolates and potentially MDR Pseudomonas aeruginosa, but the concern for resistance arises when using the agent for KPC-producing Enterobacteriales. MER-VAB appears to be more stable than CAZ-AVI in the treatment of KPC-producing Enterobacteriales but less is known about its propensity for the development of resistance and the drug does not reliably expand the coverage of meropenem-resistant P. aeruginosa isolates. IMI-REL expands the spectrum of imipenem-cilastatin to include KPC-producing Enterobacteriales as well as MDR P. aeruginosa but much less is known about its real-world clinical utility. Cefiderocol is the only of the four new agents with efficacy against metallo-beta-lactamases and resistant Acinetobacter species, but comparator studies using best available therapy for carbapenem-resistant gram-negative bacterial infections show higher mortality rates with the new drug, making its role in clinical therapy still to be determined.
Summary
The new beta-lactams differ in their mechanisms of combatting resistance and thus have unique roles in therapy. Additional evidence is needed regarding the potential for development of resistance in the newer combination agents, as well as for the role of cefiderocol in carbapenem-resistant gram-negative infections.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
CDC. The biggest antibiotic-resistant threats in the U.S. [Internet]. Centers for Disease Control and Prevention. 2019 [cited 2019 Oct 28]. Available from: https://www.cdc.gov/drugresistance/biggest-threats.html
Wang W, Jiang T, Zhang W, Li C, Chen J, Xiang D, et al. Predictors of mortality in bloodstream infections caused by multidrug-resistant gram-negative bacteria: 4 years of collection. Am J Infect Control. 2017 Jan 1;45(1):59–64.
Thaden JT, Li Y, Ruffin F, Maskarinec SA, Hill-Rorie JM, Wanda LC, et al. Increased costs associated with bloodstream infections caused by multidrug-resistant Gram-negative bacteria are due primarily to patients with hospital-acquired infections. Antimicrob Agents Chemother. 2017;61:e01709–16.
van Duin D, Kaye KS, Neuner EA, Bonomo RA. Carbapenem-resistant Enterobacteriaceae: a review of treatment and outcomes. Diagn Microbiol Infect Dis. 2013 Feb;75(2):115–20.
Thaden JT, Pogue JM, Kaye KS. Role of newer and re-emerging older agents in the treatment of infections caused by carbapenem-resistant Enterobacteriaceae. Virulence. 2017 May 19;8(4):403–16.
Gallagher JC, MacDougall C. Antibiotics simplified. Fourth ed. Burlington: Jones & Bartlett Learning; 2018. 352 p
Tracking CRE | HAI | CDC [Internet]. 2019 [cited 2019 Oct 28]. Available from: https://www.cdc.gov/hai/organisms/cre/trackingcre.html.
Bush K, Jacoby GA. Updated functional classification of β-lactamases. Antimicrob Agents Chemother. 2010;54(3):969–76.
Ceftazidime/avibactam [package insert]. Cincinnati, Ohio: Forest Laboratories; 2016.
Carmeli Y, Armstrong J, Laud PJ, Newell P, Stone G, Wardman A, et al. Ceftazidime-avibactam or best available therapy in patients with ceftazidime-resistant Enterobacteriaceae and Pseudomonas aeruginosa complicated urinary tract infections or complicated intra-abdominal infections (REPRISE): a randomised, pathogen-directed, phase 3 study. Lancet Infect Dis. 2016 Jun;16(6):661–73.
Lahiri SD, Johnstone MR, Ross PL, McLaughlin RE, Olivier NB, Alm RA. Avibactam and class C β-lactamases: mechanism of inhibition, conservation of the binding pocket, and implications for resistance. Antimicrob Agents Chemother. 2014;58(10):5704–13.
Mazuski JE, Gasink LB, Armstrong J, Broadhurst H, Stone GG, Rank D, et al. Efficacy and safety of ceftazidime-avibactam plus metronidazole versus meropenem in the treatment of complicated intra-abdominal infection: results from a randomized, controlled, double-blind, phase 3 program. Clin Infect Dis Off Publ Infect Dis Soc Am. 2016;62(11):1380–9.
Wagenlehner FM, Sobel JD, Newell P, Armstrong J, Huang X, Stone GG, et al. Ceftazidime-avibactam versus doripenem for the treatment of complicated urinary tract infections, including acute pyelonephritis: RECAPTURE, a phase 3 randomized trial program. Clin Infect Dis Off Publ Infect Dis Soc Am. 2016;63(6):754–62.
Torres A, Zhong N, Pachl J, Timsit JF, Kollef M, Chen Z, et al. Ceftazidime-avibactam versus meropenem in nosocomial pneumonia, including ventilator-associated pneumonia (REPROVE): a randomised, double-blind, phase 3 non-inferiority trial. Lancet Infect Dis. 2018;18:285–95.
• Shields RK, Nguyen MH, Chen L, Press EG, Potoski BA, Marini RV, et al. Ceftazidime-avibactam is superior to other treatment regimens against carbapenem-resistant Klebsiella pneumoniae bacteremia. Antimicrob Agents Chemother. 2017;61:e00883–17 Single-center study providing real-world clinical data supporting the use of ceftazidime-avibactam in comparison with best available therapy.
van Duin D, Lok JJ, Earley M, Cober E, Richter SS, Perez F, et al. Colistin versus ceftazidime-avibactam in the treatment of infections due to carbapenem-resistant Enterobacteriaceae. Clin Infect Dis Off Publ Infect Dis Soc Am. 2018;66(2):163–71.
Shields RK, Chen L, Cheng S, Chavda KD, Press EG, Snyder A, et al. Emergence of ceftazidime-avibactam resistance due to plasmid-borne blaKPC-3 mutations during treatment of carbapenem-resistant Klebsiella pneumoniae infections. Antimicrob Agents Chemother. 2016;61:e02097–16.
Lutgring JD, Limbago BM. The problem of carbapenemase-producing-carbapenem-resistant-Enterobacteriaceae detection. Kraft CS, editor. J Clin Microbiol. 2016;54(3):529–34.
Shields RK, Nguyen MH, Chen L, Press EG, Kreiswirth BN, Clancy CJ. 2018. Pneumonia and renal replacement therapy are risk factors for ceftazidime-avibactam treatment failures and resistance among patients with carbapenem-resistant Enterobacteriaceae infections. Antimicrob Agents Chemother. 2017;62:e02497–17.
Shields RK, Potoski BA, Haidar G, Hao B, Doi Y, Chen L, et al. Clinical outcomes, drug toxicity, and emergence of ceftazidime-avibactam resistance among patients treated for carbapenem-resistant Enterobacteriaceae infections: table 1. Clin Infect Dis. 2016;63(12):1615–8.
Stewart A, Harris P, Henderson A, Paterson D. Treatment of infections by OXA-48-producing Enterobacteriaceae. Antimicrob Agents Chemother. 2018 Aug 13;62(11):e01195–18.
Meropenem/vaborbactam [package insert]. Parsippany, NJ: The Medicines Company; 2017.
Lomovskaya O, Sun D, Rubio-Aparicio D, Nelson K, Tsivkovski R, Griffith DC, et al. Vaborbactam: spectrum of beta-lactamase inhibition and impact of resistance mechanisms on activity in Enterobacteriaceae. Antimicrob Agents Chemother. 2017;61(11):e01443–17.
Mills J. Comparative in vitro activity of meropenem/vaborbactam and meropenem against a collection of real-world clinical isolates of Pseudomonas aeruginosa. [Internet]. Poster presented at: ID Week; 2019; Washington D.C.
Kaye KS, Bhowmick T, Metallidis S, Bleasdale SC, Sagan OS, Stus V, et al. Effect of meropenem-vaborbactam vs piperacillin-tazobactam on clinical cure or improvement and microbial eradication in complicated urinary tract infection: the TANGO I randomized clinical trial. JAMA. 2018 Feb 27;319(8):788–99.
• Wunderink RG, Giamarellos-Bourboulis EJ, Rahav G, Mathers AJ, Bassetti M, Vazquez J, et al. Effect and safety of meropenem-vaborbactam versus best-available therapy in patients with carbapenem-resistant Enterobacteriaceae infections: the TANGO II randomized clinical trial. Infect Dis Ther. 2018;7(4):439–55 Open-label clinical study suggesting a potential advantage of MER-VAB compared with best available therapy for improved outcomes in CRE infections.
Dudley M. New antibiotics: what’s in the pipeline. Presented at IDWeek; 2017. San Diego, CA.
Sabet M, Tarazi Z, Rubio-Aparicio D, Nolan TG, Parkinson J, Lomovskaya O, et al. Activity of simulated human dosage regimens of meropenem and vaborbactam against carbapenem-resistant Enterobacteriaceae in an in vitro hollow-fiber model. Antimicrob Agents Chemother. 2018;62(2):e01969–17.
Sun D, Rubio-Aparicio D, Nelson K, Dudley MN, Lomovskaya O. Meropenem-vaborbactam resistance selection, resistance prevention, and molecular mechanisms in mutants of KPC-producing Klebsiella pneumoniae. Antimicrob Agents Chemother. 2017;61:e01694–17.
Lomovskaya O, Lomovskaya O. Assessment of MIC increases with meropenem-vaborbactam and ceftazidime-avibactam in TANGO II (a phase 3 study of the treatment of CRE infections). Presented at IDWeek; 2017. San Diego, CA.
Blizzard TA, Chen H, Kim S, Wu J, Bodner R, Gude C, et al. Discovery of MK-7655, a β-lactamase inhibitor for combination with Primaxin 1. Bioorg Med Chem Lett. 2014;24(3):780–5.
Commissioner of the FDA approves new treatment for complicated urinary tract and complicated intra-abdominal infections [Internet]. FDA. 2019 [cited 2019 Sep 19]. Available from: http://www.fda.gov/news-events/press-announcements/fda-approves-new-treatment-complicated-urinary-tract-and-complicated-intra-abdominal-infections
Hirsch EB, Ledesma KR, Chang K-T, Schwartz MS, Motyl MR, Tam VH. In vitro activity of MK-7655, a novel β-lactamase inhibitor, in combination with imipenem against carbapenem-resistant Gram-negative bacteria. Antimicrob Agents Chemother. 2012 Jul;56(7):3753–7.
Lob SH, Hackel MA, Kazmierczak KM, Hoban DJ, Young K, Motyl MR, et al. In vitro activity of imipenem-relebactam against gram-negative bacilli isolated from patients with lower respiratory tract infections in the United States in 2015 - results from the SMART global surveillance program. Diagn Microbiol Infect Dis. 2017 Jun;88(2):171–6.
Schmidt-Malan SM, Mishra AJ, Mushtaq A, Brinkman CL, Patel R. In vitro activity of imipenem-relebactam and ceftolozane-tazobactam against resistant Gram-negative Bacilli. Antimicrob Agents Chemother. 2018;62(8):e00533–18.
Lapuebla A, Abdallah M, Olafisoye O, Cortes C, Urban C, Quale J, et al. Activity of meropenem combined with RPX7009, a novel β-lactamase inhibitor, against Gram-negative clinical isolates in New York City. Antimicrob Agents Chemother. 2015 Aug 1;59(8):4856–60.
Livermore DM, Warner M, Mushtaq S. Activity of MK-7655 combined with imipenem against Enterobacteriaceae and Pseudomonas aeruginosa. J Antimicrob Chemother. 2013 Oct;68(10):2286–90.
Sims M, Mariyanovski V, McLeroth P, Akers W, Lee Y-C, Brown ML, et al. Prospective, randomized, double-blind, phase 2 dose-ranging study comparing efficacy and safety of imipenem/cilastatin plus relebactam with imipenem/cilastatin alone in patients with complicated urinary tract infections. J Antimicrob Chemother. 2017;72(9):2616–26.
Lucasti C, Vasile L, Sandesc D, Venskutonis D, McLeroth P, Lala M, et al. Phase 2, dose-ranging study of relebactam with imipenem-cilastatin in subjects with complicated intra-abdominal infection. Antimicrob Agents Chemother. 2016;60(10):6234–43.
Ito A, Nishikawa T, Matsumoto S, Yoshizawa H, Sato T, Nakamura R, et al. Siderophore cephalosporin cefiderocol utilizes ferric iron transporter systems for antibacterial activity against Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2016;60(12):7396–401. https://doi.org/10.1128/AAC.01405-16.
Hsueh S-C, Lee Y-J, Huang Y-T, Liao C-H, Tsuji M, Hsueh P-R. In vitro activities of cefiderocol, ceftolozane/tazobactam, ceftazidime/avibactam and other comparative drugs against imipenem-resistant Pseudomonas aeruginosa and Acinetobacter baumannii, and Stenotrophomonas maltophilia, all associated with bloodstream infections in Taiwan. J Antimicrob Chemother. 2019;74(2):380–6. https://doi.org/10.1093/jac/dky425.
Tomaras AP, Crandon JL, McPherson CJ, Banevicius MA, Finegan SM, Irvine RL, et al. Adaptation-based resistance to siderophore-conjugated antibacterial agents by Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2013;57(9):4197–207. https://doi.org/10.1128/AAC.00629-13.
Katsube T, Wajima T, Ishibashi T, Arjona Ferreira JC, Echols R. Pharmacokinetic/pharmacodynamic modeling and simulation of cefiderocol, a parenteral siderophore cephalosporin, for dose adjustment based on renal function. Antimicrob Agents Chemother. 2017;61(1). https://doi.org/10.1128/AAC.01381-16.
Portsmouth S, van Veenhuyzen D, Echols R, Machida M, Ferreira JCA, Ariyasu M, et al. Cefiderocol versus imipenem-cilastatin for the treatment of complicated urinary tract infections caused by Gram-negative uropathogens: a phase 2, randomised, double-blind, non-inferiority trial. Lancet Infect Dis. 2018;18(12):1319–28. https://doi.org/10.1016/S1473-3099(18)30554-1.
Wagenlehner FME, Naber KG. Cefiderocol for treatment of complicated urinary tract infections. Lancet Infect Dis. 2019;19(1):22–3. https://doi.org/10.1016/S1473-3099(18)30722-9.
Shionogi, Inc. Antimicrobial drugs advisory committee cefiderocol briefing document, NDA #209445. 2019. https://www.fda.gov/media/131705/download. Accessed 30 Oct 2019.
• Pogue JM, Bonomo RA, Kaye KS. Ceftazidime/avibactam, meropenem/vaborbactam, or both? Clinical and formulary considerations. Clin Infect Dis. 2019;68(3):519–24. Review and editorial describing the difference between CAZ/AVI and MER/VAB that summarizes the place of each agent in therapy.
Jayol A, Nordmann P, Poirel L, Dubois V. Ceftazidime/avibactam alone or in combination with aztreonam against colistin-resistant and carbapenemase-producing Klebsiella pneumoniae. J Antimicrob Chemother. 2018;73(2):542–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Noval declares that she has nothing to disclose. Dr. Banoub declares that she has nothing to disclose. Dr. Claeys received research support from GenMark Diagnostics and BioFire Diagnostics and has served as a speaker for Luminex Corporation and GenMark Diagnostics. Dr. Heil declares that she has nothing to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Healthcare Associated Infections
Rights and permissions
About this article
Cite this article
Noval, M., Banoub, M., Claeys, K.C. et al. The Battle Is on: New Beta-Lactams for the Treatment of Multidrug-Resistant Gram-Negative Organisms. Curr Infect Dis Rep 22, 1 (2020). https://doi.org/10.1007/s11908-020-0710-9
Published:
DOI: https://doi.org/10.1007/s11908-020-0710-9