Abstract
Positive deviance (PD) may have an important role in infection prevention and patient safety in the hospital. There are many descriptions of successful stories of PD in different sectors from public health to education to business. PD has been applied in the healthcare setting to improve hand hygiene compliance, reduce methicillin-resistant Staphylococcus aureus, and reduce bloodstream infections in an outpatient hemodialysis center. PD promotes dialogue among leaders, managers and healthcare workers, which is a key factor in establishing a safety culture. It also enables cultural changes aimed at empowering frontline workers (the positive deviants) to innovate and improve compliance with infection prevention measures. The structure and the process of PD, and its ability to offer a space for experience discussions, changing ideas and making plans that emerge from team participation will also be discussed.
Similar content being viewed by others
Introduction
Positive deviance (PD) is based on the observation that in every community there are certain individuals or groups whose uncommon practices enable them to find better solutions to problems than their neighbors or colleagues despite having access to the same resources. These individuals are known as positive deviants [1, 2].
History
PD, pioneered by Jerry and Monique Sternin of the Positive Deviance Initiative (PDI), has been used worldwide to combat such intractable problems as childhood malnutrition, sex trafficking of girls, and poor infant health [2]. PD has also been used to control MRSA in the healthcare setting [3••, 4, 5•].
A New Form of Management
The PD approach is totally different from the traditional approach for stimulating performance improvement in any area. In PD the healthcare workers decide how the work should be done and they promote discovery among their peers. The leadership and managers support frontline workers in implementing new ideas into their routine [5•, 6••, 7]. The positive deviants discuss problems that they have noticed (e.g., Dr. X did not wash his hands before a patient examination; Dr. Y did not perform hand hygiene even after examining a patient in contact precautions). Participants discuss ways to stimulate a discussion with noncompliant individuals in a positive manner. No embarrassment is permitted.
A core principle of PD is the belief that solutions to seemingly intractable problems already exist [1, 2]. Another important concept is that problems are discovered by members of the community, and the positive deviants with a spirit of creativity and innovation will share experiences, discuss these problems, and remove the barriers to find the solutions [2, 4, 8].
Different Initiatives
There are a number of successful interventions that have applied a PD approach. These successes have been observed in more than 41 countries in different fields such as education, healthcare, nutrition, public health, protecting vulnerable groups and for some other social problems [2].
The PDI’s web site (www.positivedeviance.org) [9] shares a network organization which is dedicated to amplifying the use of the PD approach in all those concepts mentioned above.
There are some examples from around the world that are important to mention:
-
(a)
A sustained 65 % to 80 % reduction in childhood malnutrition in Vietnamese communities, reaching a population of 2.2 million people [2, 9]
-
(b)
A significant reduction in childhood malnutrition in communities in 41 different countries around the world [2, 9]
-
(c)
A reduction in neonatal mortality in Pakistan, along with a blurring of defined gender roles and an increased voice for women [2, 9]
-
(d)
A reduction of 60 % in transmission of methicillin-resistant Staphylococcus aureus (MRSA) in American hospitals [3••, 4]
-
(e)
An increase of 50 % in primary school student retention in ten participating schools in Argentina [2, 9]
-
(f)
Thousands of female circumcisions averted in Egypt and the formation of dozens of female genital mutilation-free communities [2, 9]
-
(g)
A documented reduction in trafficking of girls in impoverished communities in East Java, Indonesia [2, 9]
There are other significant initiatives using PD that can be viewed at www.positivedeviance.org [9].
By sharing experiences it is possible to find solutions and to apply simple measures that can have a tremendous impact on society [8]. Positive deviants are reflective about their practices [10] and give thought to ways to improve their work. They are stimulated to find information through the internet or books or discussions with others [8]. At first glance the strategies employed by the deviants may not seem to be very unusual or innovative; in fact some of them appear to be common sense. The PD challenge is to disseminate these strategies to others. The leaders need to believe that PD can advance engagement of frontline workers in prevention efforts and implementation of all interventions.
Changing Behavior
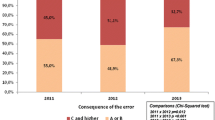
In our experience, using PD to improve hand hygiene compliance, nurse managers facilitate the discussions among frontline workers and give the positive deviants opportunities to express their feelings about the best practices for hand hygiene to be implemented and to discuss what needs to be changed, what needs to be improved, what is wrong and what is right. One of the strategies from the PD project for improving hand hygiene compliance was to show the number of alcohol gel handrub aliquots dispensed per unit and to compare data and the impressions of healthcare workers [6••, 11].
Participants in PD meetings include, in addition to the nursing staff, physical therapists, pharmacists, dietitians, physicians, and cleaning and food service staff. During one of these meetings, the idea of using an indirect metric to assess staff adherence to hand hygiene practices emerged, i.e. the ratio between the number of alcohol gel handrub aliquots dispensed (registered on electronic counters) and the number of nurse visits to patients’ rooms (obtained from the nurse call system reports). The proposal was brought up during a discussion about the value of the month-by-month comparison of alcohol gel handrub use, where there was concern regarding variation in product use due to changes in occupancy rates and workload in the hospital unit [12].
Positive deviants are multipliers, and this contributes to the success of the PD program in the different initiatives [2, 6••, 8, 9].
Infection Prevention
The infection control unit was created to prevent healthcare-associated infections in the hospital by focusing on surveillance, organizational processes, and standardization of procedures and routines. A major objective of infection control is the creation of a proactive process and a structure for systematic data collection, interpretation and dissemination of information. Some hospital settings such as the intensive care unit, the oncology unit, the bone marrow transplantation unit and the dialysis unit require more attention [13]. Our infection control unit is staffed by infectious diseases physicians and nurses (infection preventionists). These individuals are responsible for infection control across hundreds of beds. However, it is unfair to assign all of these responsibilities to only one department.
All hospital personnel (doctors, nurses, physical therapists, speech pathologists, nutritionists and pharmacists) need to act as infection preventionists. Moreover, all hospital quality indicators need to be discussed at group meetings [14]. Priorities need to be analyzed and strategies need to be defined. Everyone should understand that the knowledge of some specific processes, such as central venous catheter insertion and hand hygiene compliance, and bring valuable information that could be addressed during PD meetings or case discussions [6••, 15]. The PD strategy worked because it had the accountability of the multidisciplinary team in the planning and implementation of different measures for improving infection control and prevention in the unit [6••, 7, 16, 17]. The hospital leadership needs to be involved. There are no leaders without followers [18].
Many solutions have been suggested by positive deviants in hospital settings. Some examples include: changing the position of the alcohol gel handrub dispensers to allow easier access and use; putting alcohol gel handrub dispensers on mobile x-ray machines [19]; changing the procedure for monitoring the consumption of alcohol gel handrub, which was initially performed by one single staff member each 48 h, and gradually evolved to become the responsibility of every professional involved with patient care at the end of their shift [6••]. Other solutions using the PD process were discovery and action dialogues (DADs) with colleagues on how to make the time around change of shift safer for patients [20•]. The outcome of one DAD was an agreement that the entire dialysis unit should be cleaned and disinfected by the prior shift before allowing patients on the next dialysis shift to enter the treatment area [20•].
Infection control personnel know that such improvement processes have a tremendous impact on the quality of care, but the question remains as to how to initiate and sustain this improvement.
The first step is to decrease the distance between the infection control unit personnel and the healthcare workers. PD promotes ownership of problems by frontline workers, and empowers the positive deviants to implement the infection control prevention processes. The next step is to accept and support ideas that arise during the team observations in their daily practice.
Recently, the number of nurse visits to patient rooms was measured by a nurse call system, which was installed in two step-down units [12]. The additional metric of compliance with the use of alcohol gel handrub by the nursing staff allowed calculation of the number of alcohol gel handrub aliquots dispensed/number of nurse visits to patient rooms [12].
Patient Safety
Patient safety is the cornerstone of a high-quality healthcare system [21]. Many quality indicators have been developed to quantify the best measures for taking care of patients [18, 21]. These quality indicators are also valuable tools for guiding and evaluating the interventions that are developed in response to adverse events [21, 22].
The 100,000 Lives Campaign and the subsequent 5 Million Lives Campaign promoted by the Institute for Healthcare Improvement (IHI) were important early steps in the patient safety movement [23]. These IHI campaigns supported the improvement of medical care and encouraged hospitals to follow 12 steps to reduce harm and deaths. Four of these steps are related to infection prevention (prevention of central line infections, prevention of ventilator-associated pneumonia, prevention of surgical site infections and reducing MRSA infection). This initiative inspired other nationwide patient safety and quality improvement efforts around the world [22].
In parallel there was a need to help organize and strengthen patient safety efforts standardizing hospitals with accreditation [23]. The National Patient Safety Goals developed by the Joint Commission [24], include improving hand hygiene compliance, preventing infections that are difficult to treat (such as MRSA), preventing bloodstream infection from central lines, preventing infection after surgery, and preventing catheter-associated urinary tract infections [25, 26, 27••, 28–30].
In most settings there are numerous violations of standard procedures that can put patients at risk, and yet comparatively few lead to harm or real danger [31]. They are therefore tolerated and even viewed as normal occurrences in routine work. Furthermore, they are influenced by a range of personal, social and organizational factors and their occurrence may also have a distinct time-course as a system migrates to the boundaries of safety or recalibrates following an adverse incident [31, 32].
PD tries to improve processes every single day by analyzing work flow, questioning possible errors, and promoting the view that all tasks are as insignificant as they are important for the final result. And the improvement continues, learning together, sharing tasks, sharing knowledge and ideas, and analyzing all tasks and actions.
Social Networks
Networks that have a large core of overlapping clusters of individuals from different units or organizations and a sizeable periphery of loose connections that bring in new ideas and resources are particularly effective in generating and diffusing innovations [33••].
Recent studies using social network analysis confirm that we are influenced not only by people close to us (parents, siblings, friends), but also friends of friends [20•, 33••]. Thus, the impact of the PD approach is propagated in a social network much greater than the network of its participants [10, 20•]. In this sense, we can understand it as a complex system in which different parts of the system interact, influencing and being influenced in this regard.
PD seeks to engage all those whose behavior affects the problem and has facilitators skilled in fostering open discussion as well as in encouraging the participation of smaller groups. PD seeks those with a differential efficacy, but also involves people in their discussions that despite being part of the process are not usually involved. For example, in the case of infection prevention, human resources and transportation personnel are invited to contribute their knowledge and insights [5•]. Leaders encourage everyone to participate actively in decisions of change or who wish to try a change in their units in order to achieve better results. They also need to respond quickly when the team identifies barriers to best practices in infection prevention. The goal is for the team to be responsible for identifying opportunities for improvement, and to propose solutions and to follow the proceedings.
The structure and the PD process offer a space for discussion of experiences, ideas and plans that emerge from team participation. This requires that those managers who are experts learn to tolerate a certain amount of uncertainty in this process.
The exercise to practice thinking can lead to high-impact actions. An example is the idea to place alcohol gel handrub on portable x-ray machines that traverse the hospital, so that radiologic technicians have alcohol gel handrub available to use at any time [19].
Another study used network mapping as part of the PD strategy to prevent MRSA transmission and infection in hospitals. This mapping process revealed that network health, as measured by a set of social network analysis metrics, corresponds to low MRSA transmission rates. The analysis process also showed steps that could be taken—using a combination the interest of staff in working with others and some additional strategic linkages to connect individuals across units—that would be likely to further lower MRSA rates throughout the hospital [33••].
Most important is that all the changes that have occurred or are occurring are developed by people performing the tasks. The socialization of thought and attitude become the main role of PD.
Conclusions
The PD approach is particularly appropriate in situations where organizations can track the results with valid performance measures and where there is substantial natural variation in performance. Thus emerges a favorable environment for the discussion of practices and interventions to achieve improvements in patient safety.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Marsh DR, Schroeder DG, Dearden KA, Sternin J, Sternin M. The power of positive deviance. BMJ. 2004;329:1177–9.
Pascale R, Sternin J, Sternin M. The power of positive deviance: how unlikely innovators solve the world’s toughest problems. Boston, MA: Harvard Business Press; 2010.
•• Jain R, Kralovic SM, Evans ME, Ambrose M, Simbartl LA, Obrosky DS, et al. Veterans Affairs initiative to prevent methicillin-resistant Staphylococcus aureus infections. N Engl J Med. 2011;364:1419–30. This study describes the VA Initiative to prevent MRSA empowering frontline workers to innovate ways to control infection.
Singhal A, Buscell P, Lindberg C. Inviting everyone: healing healthcare through positive deviance. Bordentown, NJ: Plexus Press; 2010.
• Bruscell P. More we than me: how the fight against MRSA led to a new way of collaborating at Albert Einstein Medical Center. Plexus Institute; 2008. Available at: http://c.ymcdn.com/sites/www.plexusinstitute.org/resource/resmgr/docs/more-we-than-me-mrsa-vol1no5.pdf. This paper demonstrates that with wide dissemination of a positive deviance strategy, practice change is possible with multidisciplinary efforts and administrative support.
•• Marra AR, Guastelli LR, de Araújo CM, dos Santos, Filho MA, Silva CV, et al. Positive deviance: a new strategy for improving hand hygiene compliance. Infect Control Hosp Epidemiol. 2010;31:12–20. This is the first controlled trial adopting the positive deviance methodology for improving hand hygiene and decreasing healthcare-associated infections.
Rangachari P. Knowledge sharing and organizational learning the context of hospital infection prevention. Qual Manag Health Care. 2010;19:34–46.
Gawande A. Better – a surgeon's notes on performance. 1st ed. New York: Metropolitan Books; 2007.
Positive Deviance Initiative. Medford, MA: Tufts University. Available at: http://www.positivedeviance.org.
Zaidi Z, Jaffery T, Shahid A, Moin S, Gilani A, Burdick W. Change in action: using positive deviance to improve student clinical performance. Adv Health Sci Educ Theory Pract. 2012;17:95–105.
Marra AR, Guastelli LR, de Araújo CM, dos Santos JL, Filho MA, et al. Positive deviance: a program for sustained improvement in hand hygiene compliance. Am J Infect Control. 2011;39:1–5.
Macedo Rde C, Jacob EM, Silva VP, Santana EA, Souza AF, et al. Positive deviance: using a nurse call system to evaluate hand hygiene practices. Am J Infect Control. 2012;40:946–50.
Wenzel RP, Edmond MB. Infection control: the case for horizontal rather than vertical interventional programs. Int J Infect Dis. 2010;14 Suppl 4:3–5.
Caserta RA, Marra AR, Durão MS, Silva CV, Pavão dos Santos OF, Neves HS, et al. A program for sustained improvement in preventing ventilator associated pneumonia in an intensive care setting. BMC Infect Dis. 2012;12:234.
Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med. 2006;355:2725–32.
Christian G, Classen D, Griffin FA. Leadership best practices to prevent hospital-associated infections. J Patient Saf. 2012;8:144–8.
Cendoroglo Neto M, Brandt RA. Accountability and leadership in modern corporations. Einstein. 2012 (Sao Paulo);10:ix–x.
Saint S, Howell JD, Krein SL. Implementation science: how to jump-start infection prevention. Infect Control Hosp Epidemiol. 2010;31 Suppl 1:14–7.
Marra AR, Edmond MB. Hand hygiene: state-of-the-art review with emphasis on new technologies and mechanisms of surveillance. Curr Infect Dis Rep. 2012;14:585–91.
• Lindberg C, Downham G, Buscell P, Jones E, Peterson P, Krebs V. Embracing collaboration: a novel strategy for reducing bloodstream infections in outpatient hemodialysis centers. Am J Infect Control. 2013;41:513–9. The authors conclude that engaging healthcare workers through positive deviance resulted in a significant decline in bloodstream infections in outpatient hemodialysis centers.
Shekelle PG, Pronovost PJ, Wachter RM, McDonald KM, Schoelles K, Dy SM, et al. The top patient safety strategies that can be encouraged for adoption now. Ann Intern Med. 2013;158:365–8.
Krein SL, Damschroder LJ, Kowalski CP, Forman J, Hofer TP, Saint S. The influence of organizational context on quality improvement and patient safety efforts in infection prevention: a multi-center qualitative center. Soc Sci Med. 2010;71:1692–701.
Institute for Healthcare Improvement. 5 Million Lives Campaign. Cambridge, MA: Institute for Healthcare Improvement. http://www.ihi.org/offerings/Initiatives/PastStrategicInitiatives/5MillionLivesCampaign/Pages/default.aspx.
The Joint Commission. Benefits of Joint Commission Accreditation. http://www.jointcommission.org/assets/1/18/Benefits_of_Accreditation.pdf.
Boyce JM, Pittet D, Healthcare Infection Control Practices Advisory Committee; HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Guideline for Hand Hygiene in Health-Care Settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HIPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Am J Infect Control. 2002;30:S1–46.
Stone SP, Fuller C, Savage J, Cookson B, Hayward A, Cooper B, et al. Evaluation of the national Cleanyourhands campaign to reduce Staphylococcus aureus bacteraemia and Clostridium difficile infection in hospitals in England and Wales by improved hand hygiene: four year, prospective, ecological, interrupted time series study. BMJ. 2012;344:1–11.
•• Gould DJ, Moralejo D, Drey N, Chudleigh JH. Interventions to improve hand hygiene compliance in patient care. Cochrane Database Syst Rev. 2010;(9):CD005186. This paper evaluates multiple studies assessing different hand hygiene strategies for improving hand hygiene and the authors highlight the need for studies with more robust methodology.
World Health Organization. Patient Safety. WHO guidelines on hand hygiene in health care. First global patient safety challenge: clean care is safer care. Geneva: World Health Organization; 2009. http://whqlibdoc.who.int/publications/2009/9789241597906_eng.pdf.
O'Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, et al. Healthcare Infection Control Practices Advisory Committee. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2011;39 Suppl 1:1–34.
Marra AR, Sampaio Camargo TZ, Gonçalves P, Sogayar AM, Moura Jr DF, Guastelli LR, et al. Preventing catheter-associated urinary tract infection in the zero-tolerance era. Am J Infect Control. 2011;39:817–22.
Amalberti R, Vicent C, Auroy Y, de Saint Maurice G. Violations and migrations in health care: a framework for understanding and management. Qual Saf Health Care. 2006;15 Suppl 1:66–71.
Latif A, Rawat N, Pustavoitau A, Pronovost PJ, Pham JC. National study on the distribution, causes, and consequences of voluntary reported medication errors between the ICU and non-ICU settings. Crit Care Med. 2013;41:389–98.
•• Buscell P. Pathways to prevention. Mapping the positive deviance/MRSA prevention networks at Pennsylvania and Montana healthcare facilities shows promise. Prevention Strategist. 2008;Autumn:41–45. http://www.positivedeviance.org/pdf/evaluation/Pathways%20to%20Prevention.pdf. This review highlights the social networks that are helping healthcare workers control MRSA infection using a positive deviance strategy.
Compliance with Ethics Guidelines
Conflicts of Interest
Alexandre R. Marra declares that he has no conflict of interest.
Oscar Fernando Pavão dos Santos declares that he has no conflict of interest.
Miguel Cendoroglo Neto declares that he has no conflict of interest.
Michael B. Edmond declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not report any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marra, A.R., Pavão dos Santos, O.F., Cendoroglo Neto, M. et al. Positive Deviance: A New Tool for Infection Prevention and Patient Safety. Curr Infect Dis Rep 15, 544–548 (2013). https://doi.org/10.1007/s11908-013-0372-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11908-013-0372-y