Abstract
Despite advances in medical and surgical management, infective endocarditis remains associated with significant morbidity and mortality. Septic embolization to the brain and other organs is one of the most dreaded complications of infective endocarditis. Given the critical role of platelets in bacterial vegetation formation on cardiac valves or cardiac device leads, antiplatelet agents, including aspirin, have recently generated much interest as adjunctive therapies in cardiovascular infections. In this article, we review the published evidence evaluating the role of platelets in the pathogenesis of cardiovascular infections and the rationale for using antiplatelet agents in these infections.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Le KY, Sohail MR, Friedman PA, et al. Impact of timing of device removal on mortality in patients with cardiovascular implantable electronic device infections. Hear Rhythm. 2011;8:1678–85.
Sohail MR, Henrikson CA, Braid-Forbes MJ, Forbes KF, Lerner DJ. Mortality and cost associated with cardiovascular implantable electronic device infections. Arch Intern Med. 2011;171:1821–8.
Sohail MR, Uslan DZ, Khan AH, et al. Management and outcome of permanent pacemaker and implantable cardioverter-defibrillator infections. J Am Coll Cardiol. 2007;49:1851–9.
Tleyjeh IM, Steckelberg JM, Murad HS, et al. Temporal trends in infective endocarditis: a population-based study in Olmsted County, Minnesota. JAMA. 2005;293:3022–8.
Vilacosta I, Graupner C, San Roman JA, et al. Risk of embolization after institution of antibiotic therapy for infective endocarditis. J Am Coll Cardiol. 2002;39:1489–95.
Bonow RO, Carabello BA, Chatterjee K, et al. 2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;52:e1–142.
Kim DH, Kang DH, Lee MZ, et al. Impact of early surgery on embolic events in patients with infective endocarditis. Circulation. 2010;122:S17–22.
Clawson CC, Rao GH, White JG. Platelet interaction with bacteria. IV. Stimulation of the release reaction. Am J Pathol. 1975;81:411–20.
Fowler VG Jr, Scheld W, Bayer AS. Endocarditis and Intravascular Infections. In: Mandell GLBJ, Dolin R, editors. Principles and Practice of Infectious Diseases. 7th ed. Philadelphia, PA: Elsevier Churchill Livingstone; 2009.
Kupferwasser LI, Yeaman MR, Shapiro SM, et al. Acetylsalicylic acid reduces vegetation bacterial density, hematogenous bacterial dissemination, and frequency of embolic events in experimental Staphylococcus aureus endocarditis through antiplatelet and antibacterial effects. Circulation. 1999;99:2791–7.
Scheld WM, Valone JA, Sande MA. Bacterial adherence in the pathogenesis of endocarditis. Interaction of bacterial dextran, platelets, and fibrin. J Clin Invest. 1978;61:1394–404.
Kupferwasser LI, Yeaman MR, Nast CC, et al. Salicylic acid attenuates virulence in endovascular infections by targeting global regulatory pathways in Staphylococcus aureus. J Clin Invest. 2003;112:222–33.
Nicolau DP, Freeman CD, Nightingale CH, et al. Reduction of bacterial titers by low-dose aspirin in experimental aortic valve endocarditis. Infect Immun. 1993;61:1593–5.
Nicolau DP, Marangos MN, Nightingale CH, Quintiliani R. Influence of aspirin on development and treatment of experimental Staphylococcus aureus endocarditis. Antimicrob Agents Chemother. 1995;39:1748–51.
Nicolau DP, Tessier PR, Nightingale CH. Beneficial effect of combination antiplatelet therapy on the development of experimental Staphylococcus aureus endocarditis. Int J Antimicrob Agents. 1999;11:159–61.
Nicolau DP, Tessier PR, Nightingale CH, Quintiliani R. Influence of adjunctive ticlopidine on the treatment of experimental Staphylococcus aureus endocarditis. Int J Antimicrob Agents. 1998;9:227–9.
Domenico P, Schwartz S, Cunha BA. Reduction of capsular polysaccharide production in Klebsiella pneumoniae by sodium salicylate. Infect Immun. 1989;57:3778–82.
Polonio RE, Mermel LA, Paquette GE, Sperry JF. Eradication of biofilm-forming Staphylococcus epidermidis (RP62A) by a combination of sodium salicylate and vancomycin. Antimicrob Agents Chemother. 2001;45:3262–6.
Taha TH, Durrant SS, Mazeika PK, Nihoyannopoulos P, Oakley CM. Aspirin to prevent growth of vegetations and cerebral emboli in infective endocarditis. J Intern Med. 1992;231:543–6.
Chan KL, Dumesnil JG, Cujec B, et al. A randomized trial of aspirin on the risk of embolic events in patients with infective endocarditis. J Am Coll Cardiol. 2003;42:775–80.
Chan KL, Tam J, Dumesnil JG, et al. Effect of long-term aspirin use on embolic events in infective endocarditis. Clin Infect Dis. 2008;46:37–41.
Anavekar NS, Tleyjeh IM, Mirzoyev Z, et al. Impact of prior antiplatelet therapy on risk of embolism in infective endocarditis. Clin Infect Dis. 2007;44:1180–6.
•• Anavekar NS, Schultz JC, De Sa DD, et al. Modifiers of symptomatic embolic risk in infective endocarditis. Mayo Clin Proc. 2011;86:1068–74. This study showed that embolization risk in patients with endocarditis was significantly less in patients receiving statin therapy, but not with chronic antiplatelet therapy. Neither chronic statin therapy nor aspirin therapy had a significant effect on 6-month mortality.
Serebruany VL, Miller M, Pokov AN, et al. Effect of statins on platelet PAR-1 thrombin receptor in patients with the metabolic syndrome (from the PAR-1 inhibition by statins [PARIS] study). Am J Cardiol. 2006;97:1332–6.
Tleyjeh IM, Kashour T, Hakim FA, et al. Statins for the prevention and treatment of infections: a systematic review and meta-analysis. Arch Intern Med. 2009;169:1658–67.
• Snygg-Martin U, Rasmussen RV, Hassager C, Bruun NE, Andersson R, Olaison L. The relationship between cerebrovascular complications and previously established use of antiplatelet therapy in left-sided infective endocarditis. Scand J Infect Dis. 2011;43:899–904. This study showed no significant reduction in cerebrovascular complication rate in endocarditis patients receiving chronic antiplatelet therapy.
• Eisen DP, Corey GR, McBryde ES, et al. Reduced valve replacement surgery and complication rate in Staphylococcus aureus endocarditis patients receiving acetyl-salicylic acid. J Infect. 2009;58:332–8. This was a randomized trial that showed that recent aspirin therapy was associated with reduced rate of acute valve replacement surgery without a significant effect on rate of embolization or hemorrhagic stroke.
Pepin J, Tremblay V, Bechard D, et al. Chronic antiplatelet therapy and mortality among patients with infective endocarditis. Clin Microbiol Infect. 2009;15:193–9.
•• Habib A, Le KY, Baddour LM, et al. Predictors of Mortality in Patients With Cardiovascular Implantable Electronic Device Infections. Am J Cardiol 2012. This study showed that patients with CIED infection that were on chronic aspirin therapy were less likely to have vegetations on cardiac device leads or heart valves, and less likely to have systemic manifestations of infection. There was no significant difference in mortality or pathogen distribution, however.
Greenspon AJ, Prutkin JM, Sohail MR, et al. Timing of the most recent device procedure influences the clinical outcome of lead-associated endocarditis results of the MEDIC (Multicenter Electrophysiologic Device Infection Cohort). J Am Coll Cardiol. 2012;59:681–7.
Le KY, Sohail MR, Friedman PA, et al. Clinical predictors of cardiovascular implantable electronic device-related infective endocarditis. Pacing Clin Electrophysiol. 2011;34:450–9.
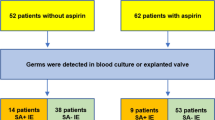
Habib A, Irfan M, Baddour LM, et al. Impact of prior aspirin therapy on clinical manifestations of cardiovascular implantable electronic device infections. Europace 2012.
Jagneaux T, Taylor DE, Kantrow SP. Coagulation in sepsis. Am J Med Sci. 2004;328:196–204.
Hart RG, Kagan-Hallet K, Joerns SE. Mechanisms of intracranial hemorrhage in infective endocarditis. Stroke. 1987;18:1048–56.
Compliance with Ethics Guidelines
Conflict of Interest
Ammar Habib, Larry M. Baddour, and M. Rizwan Sohail declare that they have no conflict of interest
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Habib, A., Baddour, L.M. & Sohail, M.R. Impact of Antiplatelet Therapy on Clinical Manifestations and Outcomes of Cardiovascular Infections. Curr Infect Dis Rep 15, 347–352 (2013). https://doi.org/10.1007/s11908-013-0347-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11908-013-0347-z