Abstract
Purpose of Review
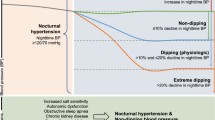
This narrative review article aims to discuss more recent evidence, current challenges, and future perspectives regarding the clinical importance of nocturnal hypertension and nighttime blood pressure dipping, with particular reference to diagnosis, prognostic value, and therapeutic approach.
Recent Findings
The importance of nighttime blood pressure and nighttime blood pressure dipping has been demonstrated in decades. Increased nighttime blood pressure has been acknowledged as an unfavorable clinical trait. However, more recent evidence suggests that the abolishment of normal circadian blood pressure rhythm is not always a solid predictor of adverse cardiovascular events and needs to be interpreted in the light of each patients’ individual characteristics. Physicians treating hypertensive patients with adverse nighttime blood pressure profiles often face the dilemma of chronotherapy. This has been a blurred field for years, yet very recent evidence from appropriately designed studies attempts to shed light on this puzzling question.
Summary
As 24-h ambulatory blood pressure monitoring is being increasingly recommended and applied in real-world practice for the diagnosis and monitoring of hypertension, information on nighttime blood pressure and nocturnal dipping profile is collected but is not always easy to interpret.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sherwood A, Steffen PR, Blumenthal JA, Kuhn C, Hinderliter AL. Nighttime blood pressure dipping: the role of the sympathetic nervous system. Am J Hypertens. 2002. https://doi.org/10.1016/S0895-7061(01)02251-8
Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018. https://doi.org/10.1093/eurheartj/ehy339
Yano Y, Kario K. Nocturnal blood pressure and cardiovascular disease: a review of recent advances. Hypertens Res. 2012. https://doi.org/10.1038/hr.2012.26
Makarem N, Alcántara C, Williams N, Bello NA, Abdalla M. Effect of sleep disturbances on blood pressure. Hypertension. 2021;7. https://doi.org/10.1161/HYPERTENSIONAHA.120.14479
Verdecchia P, Angeli F, Borgioni C, Gattobigio R, Reboldi G. Ambulatory blood pressure and cardiovascular outcome in relation to perceived sleep deprivation. Hypertension. 2007. https://doi.org/10.1161/01.HYP.0000258215.26755.20
Mulè G, Cottone S. How common is isolated nocturnal hypertension? J Hypertens. 2020. https://doi.org/10.1097/HJH.0000000000002319
Rhee M-Y, Kim JS, Kim CH, et al. Prevalence and characteristics of isolated nocturnal hypertension in the general population. Korean J Intern Med. 2021. https://doi.org/10.3904/kjim.2021.022
Salazar MR, Espeche WG, Balbín E, et al. Prevalence of isolated nocturnal hypertension according to 2018 European Society of Cardiology and European Society of Hypertension office blood pressure categories. J Hypertens. 2020. https://doi.org/10.1097/HJH.0000000000002278
Barochiner J, Díaz RR, Martínez R. Prevalence and characteristics of isolated nocturnal hypertension and masked nocturnal hypertension in a tertiary hospital in the city of Buenos Aires. Diagnostics. 2023. https://doi.org/10.3390/diagnostics13081419
Kim SH, Shin C, Kim S, et al. Prevalence of isolated nocturnal hypertension and development of arterial stiffness, left ventricular hypertrophy, and silent cerebrovascular lesions: the KoGES (Korean Genome and Epidemiology Study). J Am Heart Assoc. 2022. https://doi.org/10.1161/JAHA.122.025641
Ohkubo T. Relation between nocturnal decline in blood pressure and mortality the Ohasama study. Am J Hypertens. 1997. https://doi.org/10.1016/S0895-7061(97)00274-4
Kario K, Chia Y, Sukonthasarn A, et al. Diversity of and initiatives for hypertension management in Asia—why we need the HOPE Asia Network. J Clin Hypertens. 2020. https://doi.org/10.1111/jch.13733
Del Pozo-Valero R, Martín-Oterino JÁ, Rodríguez-Barbero A. Influence of elevated sleep-time blood pressure on vascular risk and hypertension-mediated organ damage. Chronobiol Int. 2021. https://doi.org/10.1080/07420528.2020.1835944
Nikolaidou B, Anyfanti P, Gavriilaki E, et al. Non-dipping pattern in early-stage diabetes: association with glycemic profile and hemodynamic parameters. J Hum Hypertens. 2022. https://doi.org/10.1038/s41371-021-00587-4
Sarafidis PA, Ruilope LM, Loutradis C, et al. Blood pressure variability increases with advancing chronic kidney disease stage. J Hypertens. 2018. https://doi.org/10.1097/HJH.0000000000001670
Gkaliagkousi E, Anyfanti P, Chatzimichailidou S, et al. Association of nocturnal blood pressure patterns with inflammation and central and peripheral estimates of vascular health in rheumatoid arthritis. J Hum Hypertens. 2018. https://doi.org/10.1038/s41371-018-0047-0
Stergiou GS, Palatini P, Parati G, et al. 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021. https://doi.org/10.1097/HJH.0000000000002843
Stergiou GS, Nasothimiou EG, Destounis A, Poulidakis E, Evagelou I, Tzamouranis D. Assessment of the diurnal blood pressure profile and detection of non-dippers based on home or ambulatory monitoring. Am J Hypertens. 2012. https://doi.org/10.1038/ajh.2012.82
Kollias A, Ntineri A, Stergiou GS. Association of night-time home blood pressure with night-time ambulatory blood pressure and target-organ damage: a systematic review and meta-analysis. J Hypertens. 2017. https://doi.org/10.1097/HJH.0000000000001189
Mancia G, Facchetti R, Bombelli M, Quarti-Trevano F, Cuspidi C, Grassi G. Short- and long-term reproducibility of nighttime blood pressure phenotypes and nocturnal blood pressure reduction. Hypertension. 2021. https://doi.org/10.1161/HYPERTENSIONAHA.120.16827
Rey RH, Martin-Baranera M, Sobrino J, et al. Reproducibility of the circadian blood pressure pattern in 24-h versus 48-h recordings: the Spanish Ambulatory Blood Pressure Monitoring Registry. J Hypertens. 2007. https://doi.org/10.1097/HJH.0b013e3282effed1
Dolan E, Stanton A, Thijs L, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension. 2005. https://doi.org/10.1161/01.HYP.0000170138.56903.7a
Hansen TW, Li Y, Boggia J, Thijs L, Richart T, Staessen JA. Predictive role of the nighttime blood pressure. Hypertension. 2011;5. https://doi.org/10.1161/HYPERTENSIONAHA.109.133900
Sega R, Facchetti R, Bombelli M, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005. https://doi.org/10.1161/01.CIR.0000160923.04524.5B
Staplin N, Sierra A De, Ruilope LM, et al. Articles Relationship between clinic and ambulatory blood pressure and mortality : an observational cohort study in 59 124 patients. Lancet. 2023. https://doi.org/10.1016/S0140-6736(23)00733-X
Verdecchia P, Schillaci G, Guerrieri M, et al. Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation. 1990. https://doi.org/10.1161/01.CIR.81.2.528
Cicek Y, Durakoglugil ME, Kocaman SA, et al. Non-dipping pattern in untreated hypertensive patients is related to increased pulse wave velocity independent of raised nocturnal blood pressure. Blood Press. 2013. https://doi.org/10.3109/08037051.2012.701409
de la Sierra A, Gorostidi M, Banegas JR, Segura J, de la Cruz JJ, Ruilope LM. Nocturnal hypertension or nondipping: which is better associated with the cardiovascular risk profile? Am J Hypertens. 2014. https://doi.org/10.1093/ajh/hpt175
Cuspidi C, Sala C, Tadic M, Gherbesi E, Grassi G, Mancia G. Nondipping pattern and carotid atherosclerosis. J Hypertens. 2016. https://doi.org/10.1097/HJH.0000000000000812
Salles GF, Reboldi G, Fagard RH, et al. Prognostic effect of the nocturnal blood pressure fall in hypertensive patients. Hypertension. 2016. https://doi.org/10.1161/HYPERTENSIONAHA.115.06981
• Kario K, Hoshide S, Mizuno H, et al. Nighttime blood pressure phenotype and cardiovascular prognosis: practitioner-based nationwide JAMP study. Circulation. 2020. https://doi.org/10.1161/CIRCULATIONAHA.120.049730. Findings from this study suggest that the cumulative rate of cardiovascular events is independently correlated with nighttime blood pressure levels and a riser pattern.
Palatini P, Verdecchia P, Beilin LJ, et al. Association of extreme nocturnal dipping with cardiovascular events strongly depends on age. Hypertension. 2020. https://doi.org/10.1161/HYPERTENSIONAHA.119.14085
Lopez-Sublet M, Girerd N, Bozec E, et al. Nondipping pattern and cardiovascular and renal damage in a population-based study (the STANISLAS cohort study). Am J Hypertens. 2019. https://doi.org/10.1093/ajh/hpz020
Gavriilaki M, Anyfanti P, Nikolaidou B, et al. Nighttime dipping status and risk of cardiovascular events in patients with untreated hypertension: a systematic review and meta-analysis. J Clin Hypertens (Greenwich). 2020. https://doi.org/10.1111/jch.14039
Androulakis E, Papageorgiou N, Chatzistamatiou E, Kallikazaros I, Stefanadis C, Tousoulis D. Improving the detection of preclinical organ damage in newly diagnosed hypertension: nocturnal hypertension versus non-dipping pattern. J Hum Hypertens. 2015. https://doi.org/10.1038/jhh.2015.5
Gkaliagkousi E, Anyfanti P, Lazaridis A, et al. Clinical impact of dipping and nocturnal blood pressure patterns in newly diagnosed, never-treated patients with essential hypertension. J Am Soc Hypertens. 2018. https://doi.org/10.1016/j.jash.2018.08.004
Gkaliagkousi E, Anyfanti P, Douma S. In the deep end of dipping: nocturnal blood pressure fall and surrogate cardiovascular risk markers in individuals with optimal 24-hour blood pressure. Am J Hypertens. 2019. https://doi.org/10.1093/ajh/hpz033
Anyfanti P, Douma S, Gkaliagkousi E. Prognostic value of daytime and nighttime blood pressure in treated hypertensives: one size does not fit all. J Clin Hypertens (Greenwich). 2020. https://doi.org/10.1111/jch.14027
Jones NR, McCormack T, Constanti M, McManus RJ. Diagnosis and management of hypertension in adults: NICE guideline update 2019. Br J Gen Pract. 2020. https://doi.org/10.3399/bjgp20X708053
Parati G, Lombardi C, Hedner J, et al. Recommendations for the management of patients with obstructive sleep apnoea and hypertension. Eur Respir J. 2013. https://doi.org/10.1183/09031936.00226711
Poulter NR, Savopoulos C, Anjum A, et al. Randomized crossover trial of the impact of morning or evening dosing of antihypertensive agents on 24-hour ambulatory blood pressure. Hypertension. 2018. https://doi.org/10.1161/HYPERTENSIONAHA.118.11101
Lafeber M, Grobbee DE, Schrover IM, et al. Comparison of a morning polypill, evening polypill and individual pills on LDL-cholesterol, ambulatory blood pressure and adherence in high-risk patients; a randomized crossover trial. Int J Cardiol. 2015. https://doi.org/10.1016/j.ijcard.2014.11.176
Zappe DH, Crikelair N, Kandra A, Palatini P. Time of administration important? Morning versus evening dosing of valsartan. J Hypertens. 2015. https://doi.org/10.1097/HJH.0000000000000397
Kario K, Hoshide S, Uchiyama K, et al. Dose Timing of an angiotensin II receptor blocker/calcium channel blocker combination in hypertensive patients with paroxysmal atrial fibrillation. J Clin Hypertens. 2016. https://doi.org/10.1111/jch.12814
Huangfu W, Duan P, Xiang D, Gao R. Administration time-dependent effects of combination therapy on ambulatory blood pressure in hypertensive subjects. Int J Clin Exp Med. 2015;8(10):19156–61.
Xie Z, Zhang J, Wang C, Yan X. Chronotherapy for morning blood pressure surge in hypertensive patients: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2021. https://doi.org/10.1186/s12872-021-02081-8
Hermida RC, Ayala DE, Mojón A, Fernández JR. Influence of circadian time of hypertension treatment on cardiovascular risk: results of the MAPEC study. Chronobiol Int. 2010. https://doi.org/10.3109/07420528.2010.510230
Hermida RC, Crespo JJ, Domínguez-Sardiña M, et al. Bedtime hypertension treatment improves cardiovascular risk reduction: the Hygia Chronotherapy Trial. Eur Heart J. 2020. https://doi.org/10.1093/eurheartj/ehz754
Kreutz R, Kjeldsen SE, Burnier M, Narkiewicz K, Oparil S, Mancia G. Blood pressure medication should not be routinely dosed at bedtime. We must disregard the data from the HYGIA project. Blood Press. 2020. https://doi.org/10.1080/08037051.2020.1747696
• Mackenzie IS, Rogers A, Poulter NR, et al. Cardiovascular outcomes in adults with hypertension with evening versus morning dosing of usual antihypertensives in the UK (TIME study): a prospective, randomised, open-label, blinded-endpoint clinical trial. Lancet. 2022. https://doi.org/10.1016/S0140-6736(22)01786-X. Findings from this study suggest that administration of the usual antihypertensive agents in the evening does not differ from morning dosing in terms of cardiovascular outcomes. Thus, antihypertensive treatment may be given at a time when it is convenient for the patient and limits the adverse effects of the medications.
•• Stergiou G, Brunström M, MacDonald T, et al. Bedtime dosing of antihypertensive medications: systematic review and consensus statement: International Society of Hypertension position paper endorsed by World Hypertension League and European Society of Hypertension. J Hypertens. 2022. https://doi.org/10.1097/HJH.0000000000003240.This Position Paper by the International Society of Hypertension provides consensus recommendations for clinical practice based on available evidence on the clinical relevance of the diurnal variation in blood pressure and the timing of antihypertensive drug dosing.
Sobiczewski W, Wirtwein M, Gruchała M, Kocić I. Mortality in hypertensive patients with coronary heart disease depends on chronopharmacotherapy and dipping status. Pharmacol Reports. 2014. https://doi.org/10.1016/j.pharep.2013.12.009
Farah R, Makhoul N, Arraf Z, Khamisy-Farah R. Switching therapy to bedtime for uncontrolled hypertension with a nondipping pattern: a prospective randomized-controlled study. Blood Press Monit. 2013. https://doi.org/10.1097/MBP.0b013e3283624aed
Black HR, Elliott WJ, Grandits G, et al. Principal results of the controlled onset verapamil investigation of cardiovascular end points (CONVINCE) Trial. Jama. 2003. https://doi.org/10.1001/jama.289.16.2073
Funding
The authors have received no funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Anyfanti, P., Malliora, A., Chionidou, A. et al. Clinical Significance of Nocturnal Hypertension and Nighttime Blood Pressure Dipping in Hypertension. Curr Hypertens Rep 26, 69–80 (2024). https://doi.org/10.1007/s11906-023-01277-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11906-023-01277-x