Abstract
Purpose of Review
To review recent data describing the challenges and innovations in therapeutic research focused on the prevention and treatment of preeclampsia.
Recent Findings
Pregnant individuals have traditionally been excluded from therapeutic research, resulting in a paucity of innovation in therapeutics for pregnancy-specific medical conditions, especially preeclampsia. With the increased awareness of maternal morbidity and mortality, there is significant interest among researchers to expand therapeutic research in pregnancy. Several medications, including aspirin, pravastatin, metformin, and esomeprazole, which are commonly used in non-pregnant populations, are now being investigated for preeclampsia prevention. However, given the historic precedent of exclusion, along with the regulatory, ethical, and feasibility concerns that accompany this population, the study of these and novel medications has been complicated by numerous challenges.
Summary
While complex, and laden with challenges, there is great ongoing need for therapeutic research to address preeclampsia. Aspirin, pravastatin, metformin, and esomeprazole have all shown promise as potential therapeutic agents; however, their use remains to be optimized, and innovative therapeutics need to be developed.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006–2010. Obstet Gynecol. 2015;125(1):5–12. https://doi.org/10.1097/AOG.0000000000000564.
American College of Obstetricians and Gynecologists. Gestational hypertension and preeclampsia: ACOG practice bulletin 222. Obstet Gynecol. 2020;135(6):e237–60.
Michalczyk M, Celewicz A, Celewicz M, Woźniakowska-Gondek P, Rzepka R. The role of inflammation in the pathogenesis of preeclampsia. Mediators Inflamm. 2020;2020:1–9. https://doi.org/10.1155/2020/3864941.
Centers for Disease Control and Prevention. High blood pressure during pregnancy. Accessed June 19, 2023. https://www.cdc.gov/bloodpressure/pregnancy.htm.
Cameron NA, Everitt I, Seegmiller LE, Yee LM, Grobman WA, Khan SS. Trends in the incidence of new‐onset hypertensive disorders of pregnancy among rural and urban areas in the United States, 2007 to 2019. J Am Heart Assoc. 2022;11(2). https://doi.org/10.1161/JAHA.121.023791.
Ananth CV, Keyes KM, Wapner RJ. Pre-eclampsia rates in the United States, 1980–2010: age-period-cohort analysis. BMJ. 2013;347(nov07 15):f6564-f6564. https://doi.org/10.1136/bmj.f6564.
Zhang J, Troendle JF, Levine RJ. Risks of hypertensive disorders in the second pregnancy. Paediatr Perinat Epidemiol. 2001;15(3):226–31. https://doi.org/10.1046/j.1365-3016.2001.00347.x.
Bernardes TP, Mol BW, Ravelli ACJ, van den Berg P, Boezen HM, Groen H. Early and late onset pre-eclampsia and small for gestational age risk in subsequent pregnancies. PLoS ONE. 2020;15(3): e0230483. https://doi.org/10.1371/journal.pone.0230483.
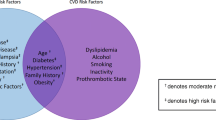
Mongraw-Chaffin ML, Cirillo PM, Cohn BA. Preeclampsia and cardiovascular disease death. Hypertension. 2010;56(1):166–71. https://doi.org/10.1161/HYPERTENSIONAHA.110.150078.
• Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335(7627):974. https://doi.org/10.1136/bmj.39335.385301.BE. This systematic review and meta-analysis characterizes the risk of future vascular disease among those diagnosed with preeclampsia and identifies an associated increased risk of mortality after 14.5 years.
Van Pampus MG, Aarnoudse JG. Long-term outcomes after preeclampsia. Clin Obstet Gynecol. 2005;48(2):489–94. https://doi.org/10.1097/01.grf.0000160316.67359.3d.
McDonald SD, Malinowski A, Zhou Q, Yusuf S, Devereaux PJ. Cardiovascular sequelae of preeclampsia/eclampsia: a systematic review and meta-analyses. Am Heart J. 2008;156(5):918–30. https://doi.org/10.1016/j.ahj.2008.06.042.
Kaaja RJ. Manifestations of chronic disease during pregnancy. JAMA. 2005;294(21):2751. https://doi.org/10.1001/jama.294.21.2751.
Leon LJ, McCarthy FP, Direk K, et al. Preeclampsia and cardiovascular disease in a large UK pregnancy cohort of linked electronic health records. Circulation. 2019;140(13):1050–60. https://doi.org/10.1161/CIRCULATIONAHA.118.038080.
Harmon QE, Huang L, Umbach DM, et al. Risk of fetal death with preeclampsia. Obstet Gynecol. 2015;125(3):628–35. https://doi.org/10.1097/AOG.0000000000000696.
Srinivas SK, Edlow AG, Neff PM, Sammel MD, Andrela CM, Elovitz MA. Rethinking IUGR in preeclampsia: dependent or independent of maternal hypertension? J Perinatol. 2009;29(10):680–4. https://doi.org/10.1038/jp.2009.83.
Meis PJ, Goldenberg RL, Mercer BM, et al. The preterm prediction study: risk factors for indicated preterm births. Am J Obstet Gynecol. 1998;178(3):562–7. https://doi.org/10.1016/S0002-9378(98)70439-9.
Ananth CV, Vintzileos AM. Maternal-fetal conditions necessitating a medical intervention resulting in preterm birth. Am J Obstet Gynecol. 2006;195(6):1557–63. https://doi.org/10.1016/j.ajog.2006.05.021.
Risnes K, Bilsteen JF, Brown P, et al. Mortality among young adults born preterm and early term in 4 Nordic nations. JAMA Netw Open. 2021;4(1): e2032779. https://doi.org/10.1001/jamanetworkopen.2020.32779.
Sejer EPF, Bruun FJ, Slavensky JA, Mortensen EL, Schiøler KU. Impact of gestational age on child intelligence, attention and executive function at age 5: a cohort study. BMJ Open. 2019;9(9): e028982. https://doi.org/10.1136/bmjopen-2019-028982.
Maher GM, O’Keeffe GW, Kearney PM, et al. Association of hypertensive disorders of pregnancy with risk of neurodevelopmental disorders in offspring. JAMA Psychiat. 2018;75(8):809. https://doi.org/10.1001/jamapsychiatry.2018.0854.
Tuovinen S, Eriksson JG, Kajantie E, et al. Maternal hypertensive disorders in pregnancy and self-reported cognitive impairment of the offspring 70 years later: the Helsinki Birth Cohort Study. Am J Obstet Gynecol. 2013;208(3):200.e1-200.e9. https://doi.org/10.1016/j.ajog.2012.12.017.
van Wassenaer AG, Westera J, van Schie PEM, et al. Outcome at 4.5 years of children born after expectant management of early-onset hypertensive disorders of pregnancy. Am J Obstet Gynecol. 2011;204(6):510.e1–510.e9. https://doi.org/10.1016/j.ajog.2011.02.032.
Sun BZ, Moster D, Harmon QE, Wilcox AJ. Association of preeclampsia in term births with neurodevelopmental disorders in offspring. JAMA Psychiat. 2020;77(8):823. https://doi.org/10.1001/jamapsychiatry.2020.0306.
Stevens W, Shih T, Incerti D, et al. Short-term costs of preeclampsia to the United States health care system. Am J Obstet Gynecol. 2017;217(3):237-248.e16. https://doi.org/10.1016/j.ajog.2017.04.032.
Centers for Disease Control and Prevention. Pregnancy mortality surveillance system. Published March 23, 2023. Accessed October 1, 2023. https://www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm.
Petersen EE, Davis NL, Goodman D, et al. Racial/ethnic disparities in pregnancy-related deaths — United States, 2007–2016. MMWR Morb Mortal Wkly Rep. 2019;68(35):762–5. https://doi.org/10.15585/mmwr.mm6835a3.
Petersen EE, Davis NL, Goodman D, et al. Vital signs: pregnancy-related deaths, United States, 2011–2015, and strategies for prevention, 13 states, 2013–2017. MMWR Morb Mortal Wkly Rep. 2019;68(18). https://doi.org/10.15585/mmwr.mm6818e1.
Chornock R, Iqbal SN, Kawakita T. Racial disparity in postpartum readmission due to hypertension among women with pregnancy-associated hypertension. Am J Perinatol. 2021;38(12):1297–302. https://doi.org/10.1055/s-0040-1712530.
Howell EA. Reducing disparities in severe maternal morbidity and mortality. Clin Obstet Gynecol. 2018;61(2):387–99. https://doi.org/10.1097/GRF.0000000000000349.
Shahul S, Tung A, Minhaj M, et al. Racial disparities in comorbidities, complications, and maternal and fetal outcomes in women with preeclampsia/eclampsia. Hypertens Pregnancy. 2015;34(4):506–15. https://doi.org/10.3109/10641955.2015.1090581.
Tanaka M, Jaamaa G, Kaiser M, et al. Racial disparity in hypertensive disorders of pregnancy in New York State: a 10-year longitudinal population-based study. Am J Public Health. 2007;97(1):163–70. https://doi.org/10.2105/AJPH.2005.068577.
Ford ND, Cox S, Ko JY, et al. Hypertensive disorders in pregnancy and mortality at delivery hospitalization — United States, 2017–2019. MMWR Morb Mortal Wkly Rep. 2022;71(17):585–91. https://doi.org/10.15585/mmwr.mm7117a1.
Merkt PT, Kramer MR, Goodman DA, et al. Urban-rural differences in pregnancy-related deaths, United States, 2011–2016. Am J Obstet Gynecol. 2021;225(2):183.e1-183.e16. https://doi.org/10.1016/j.ajog.2021.02.028.
Bailey ZD, Feldman JM, Bassett MT. How structural racism works — racist policies as a root cause of U.S. racial health inequities. New England J Med. 2021;384(8):768–773. https://doi.org/10.1056/NEJMms2025396.
Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. The Lancet. 2017;389(10077):1453–63. https://doi.org/10.1016/S0140-6736(17)30569-X.
American College of Obstetricians and Gynecologists. Low-dose aspirin use during pregnancy. ACOG Committee Opinion No. 743. Obstet Gynecol. 2018;132:e44–52.
Davidson KW, Barry MJ, Mangione CM, et al. Aspirin use to prevent preeclampsia and related morbidity and mortality. JAMA. 2021;326(12):1186. https://doi.org/10.1001/jama.2021.14781.
McKiever M, Frey H, Costantine MM. Challenges in conducting clinical research studies in pregnant women. J Pharmacokinet Pharmacodyn. 2020;47(4):287–93. https://doi.org/10.1007/s10928-020-09687-z.
Wesley BD, Sewell CA, Chang CY, Hatfield KP, Nguyen CP. Prescription medications for use in pregnancy–perspective from the US Food and Drug Administration. Am J Obstet Gynecol. 2021;225(1):21–32. https://doi.org/10.1016/j.ajog.2021.02.032.
Byrne JJ, Saucedo AM, Spong CY. Evaluation of drug labels following the 2015 pregnancy and lactation labeling rule. JAMA Netw Open. 2020;3(8): e2015094. https://doi.org/10.1001/jamanetworkopen.2020.15094.
United States Department of Health E, WPHSF, DA. General considerations for the clinical evaluation of drugs. 1977. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/general-considerations-clinical-evaluation-drugs. Accessed 31 Oct 2023.
Federal Register 1979. Labeling and prescription drug advertising: content and format for labeling for human prescription drugs. 1979.
National Institutes of Health Revitalization Act of 1993 Public Law 103–43. 1993. https://grants.nih.gov/policy/inclusion/women-and-minorities/guidelines.htm#:~:text=The%20NIH%20Revitalization%20Act%20of,and%20minorities%20in%20clinical%20research. Accessed 31 Oct 2023.
U.S. Food & Drug Administration. Guideline for the study and evaluation for gender differences in the clinical evaluation of drugs. 1993. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/study-and-evaluation-gender-differences-clinical-evaluation-drugs. Accessed 31 Oct 2023.
Task Force on research specific to pregnant women and lactating women: report to secretary, health and human services, Congress. 2018.
Byrne JJ, Saucedo AM, Spong CY. Task force on research specific to pregnant and lactating women. Semin Perinatol. 2020;44(3): 151226. https://doi.org/10.1016/j.semperi.2020.151226.
Nooney J, Thor S, Vries C, et al. Assuring access to safe medicines in Pregnancy and breastfeeding. Clin Pharmacol Ther. 2021;110(4):941–5. https://doi.org/10.1002/cpt.2212.
Dorato MA, Engelhardt JA. The no-observed-adverse-effect-level in drug safety evaluations: Use, issues, and definition(s). Regul Toxicol Pharmacol. 2005;42(3):265–74. https://doi.org/10.1016/j.yrtph.2005.05.004.
Ahmed S, Brewer A, Tsigas EZ, Rogers C, Chappell L, Hewison J. Women’s attitudes, beliefs and values about tests, and management for hypertensive disorders of pregnancy. BMC Pregnancy Childbirth. 2021;21(1):665. https://doi.org/10.1186/s12884-021-04144-2.
Schonfeld T. The perils of protection: vulnerability and women in clinical research. Theor Med Bioeth. 2013;34(3):189–206. https://doi.org/10.1007/s11017-013-9258-0.
Rolnik DL, Nicolaides KH, Poon LC. Prevention of preeclampsia with aspirin. Am J Obstet Gynecol. 2022;226(2):S1108–19. https://doi.org/10.1016/j.ajog.2020.08.045.
Goodlin RC, Haesslein HO, Fleming J. Aspirin for the treatment of recurrent toxaemia. The Lancet. 1978;312(8079):51. https://doi.org/10.1016/S0140-6736(78)91367-3.
Beaufils M, Donsimoni R, Uzan S, Colau JC. Prevention of pre-eclampsia by early antiplatelet therapy. The Lancet. 1985;325(8433):840–2. https://doi.org/10.1016/S0140-6736(85)92207-X.
Askie LM, Duley L, Henderson-Smart DJ, Stewart LA. Antiplatelet agents for prevention of pre-eclampsia: a meta-analysis of individual patient data. The Lancet. 2007;369(9575):1791–8. https://doi.org/10.1016/S0140-6736(07)60712-0.
• Duley L, Meher S, Hunter KE, Seidler AL, Askie LM. Antiplatelet agents for preventing pre-eclampsia and its complications. Cochr Data Syst Rev. 2019;(10). https://doi.org/10.1002/14651858.CD004659.pub3. This systematic review found reductions in adverse pregnancy outcomes, including reduced risk of preeclampsia, preterm birth, small for gestational age infants, and fetal or neonatal death associated with use of low dose aspirin during pregnancy.
Roberge S, Sibai B, McCaw-Binns A, Bujold E. Low-dose aspirin in early gestation for prevention of preeclampsia and small-for-gestational-age neonates: meta-analysis of large randomized trials. Am J Perinatol. 2016;33(08):781–5. https://doi.org/10.1055/s-0036-1572495.
World Health Organization. WHO recommendations for prevention and treatment of pre-eclampsia and eclampsia. Published online 2011. Accessed April 6, 2023. http://apps.who.int/iris/bitstream/10665/44703/1/9789241548335_eng.pdf.
American College of Obstetricians and Gynecologists. Hypertension in pregnancy. Published online 2013. Accessed April 6, 2023. http://www.acog.org/Resources-And-Publications/Task-Force-and-Work-Group-Reports/Hypertension-in-Pregnancy.
LeFevre ML. Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;161(11):819. https://doi.org/10.7326/M14-1884.
American College of Obstetricians and Gynecologists. ACOG committee opinion No. 743: low-dose aspirin use during pregnancy. Obstet Gynecol. 2018;132(1):e44-e52. https://doi.org/10.1097/AOG.0000000000002708.
Ayala NK, Rouse DJ. A nudge toward universal aspirin for preeclampsia prevention. Obstet Gynecol. 2019;133(4):725–8. https://doi.org/10.1097/AOG.0000000000003167.
Rolnik DL, Wright D, Poon LC, et al. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. N Engl J Med. 2017;377(7):613–22. https://doi.org/10.1056/NEJMoa1704559.
Van Doorn R, Mukhtarova N, Flyke IP, et al. Dose of aspirin to prevent preterm preeclampsia in women with moderate or high-risk factors: a systematic review and meta-analysis. PLoS ONE. 2021;16(3): e0247782. https://doi.org/10.1371/journal.pone.0247782.
Stossel TP. The discovery of statins. Cell. 2008;134(6):903–5. https://doi.org/10.1016/j.cell.2008.09.008.
Stancu C, Sima A. Statins: mechanism of action and effects. J Cell Mol Med. 2001;5(4):378–87. https://doi.org/10.1111/j.1582-4934.2001.tb00172.x.
Ahmed A, Singh J, Khan Y, Seshan SV, Girardi G. A new mouse model to explore therapieS FOR PREECLAMPSIA. PLoS ONE. 2010;5(10): e13663. https://doi.org/10.1371/journal.pone.0013663.
Singh J, Ahmed A, Girardi G. Role of complement component C1q in the onset of preeclampsia in mice. Hypertension. 2011;58(4):716–24. https://doi.org/10.1161/HYPERTENSIONAHA.111.175919.
Fox KA, Longo M, Tamayo E, et al. Effects of pravastatin on mediators of vascular function in a mouse model of soluble Fms-like tyrosine kinase-1–induced preeclampsia. Am J Obstet Gynecol. 2011;205(4):366.e1-366.e5. https://doi.org/10.1016/j.ajog.2011.06.083.
Costantine MM, Tamayo E, Lu F, et al. Using pravastatin to improve the vascular reactivity in a mouse model of soluble Fms-like tyrosine kinase-1–induced preeclampsia. Obstet Gynecol. 2010;116(1):114–20. https://doi.org/10.1097/AOG.0b013e3181e10ebd.
Costantine MM, Cleary K, Hebert MF, et al. Safety and pharmacokinetics of pravastatin used for the prevention of preeclampsia in high-risk pregnant women: a pilot randomized controlled trial. Am J Obstet Gynecol. 2016;214(6):720.e1-720.e17. https://doi.org/10.1016/j.ajog.2015.12.038.
Costantine MM, West H, Wisner KL, et al. A randomized pilot clinical trial of pravastatin versus placebo in pregnant patients at high risk of preeclampsia. Am J Obstet Gynecol. 2021;225(6):666.e1-666.e15. https://doi.org/10.1016/j.ajog.2021.05.018.
Akbar MIA, Azis MA, Riu DS, et al. INOVASIA study: a multicenter randomized clinical trial of pravastatin to prevent preeclampsia in High-risk patients. Am J Perinatol. Published online March 15, 2022. https://doi.org/10.1055/a-1798-1925.
Döbert M, Varouxaki AN, Mu AC, et al. Pravastatin versus placebo in pregnancies at high risk of term preeclampsia. Circulation. 2021;144(9):670–9. https://doi.org/10.1161/CIRCULATIONAHA.121.053963.
• Costantine MM, Cleary K. Pravastatin for the prevention of preeclampsia in high-risk pregnant women. Obstet Gynecol. 2013;121(2):349–353. https://doi.org/10.1097/AOG.0b013e31827d8ad5. This commentary reviews the biologic plausibility, safety, and existing animal and human data regarding the use of pravastatin for preeclampsia prevention.
Kazmin A, Garcia-Bournissen F, Koren G. Motherisk rounds: risks of Statin use during pregnancy: a systematic review. J Obstet Gynaecol Can. 2007;29(11):906–8. https://doi.org/10.1016/S1701-2163(16)32656-1.
Bateman BT, Hernandez-Diaz S, Fischer MA, et al. Statins and congenital malformations: cohort study. BMJ. 2015;350(mar17 10):h1035-h1035. https://doi.org/10.1136/bmj.h1035.
Edison RJ, Muenke M. Mechanistic and epidemiologic considerations in the evaluation of adverse birth outcomes following gestational exposure to statins. Am J Med Genet. 2004;131A(3):287–98. https://doi.org/10.1002/ajmg.a.30386.
U.S. Food & Drug Administration. FDA requests removal of strongest warning against using cholesterol-lowering statins during pregnancy; still advises most pregnant patients should stop taking statins. Accessed November 6, 2022. https://www.fda.gov/drugs/drug-safety-and-availability/fda-requests-removal-strongest-warning-against-using-cholesterol-lowering-statins-during-pregnancy.
Ahmed A, Williams D, Cheed V, et al. Pravastatin for early-onset pre-eclampsia: a randomised, blinded, placebo-controlled trial. BJOG. 2020;127(4):478–88. https://doi.org/10.1111/1471-0528.16013.
Costantine MM. Long-term child follow-up of the pravastatin for prevention of preeclampsia pilot trials. Am J Obstet Gynecol. 2022;226(1):S74–5. https://doi.org/10.1016/j.ajog.2021.11.142.
Coetzee EJ, Jackson WPU. Metformin in management of pregnant insulin-independent diabetics. Diabetologia. 1979;16(4):241–5. https://doi.org/10.1007/BF01221950.
Moore LE, Briery CM, Clokey D, et al. Metformin and insulin in the management of gestational diabetes mellitus: preliminary results of a comparison. J Reprod Med. 2007;52(11):1011–5.
Gui J, Liu Q, Feng L. Metformin vs insulin in the management of gestational diabetes: a meta-analysis. PLoS ONE. 2013;8(5): e64585. https://doi.org/10.1371/journal.pone.0064585.
Butalia S, Gutierrez L, Lodha A, Aitken E, Zakariasen A, Donovan L. Short- and long-term outcomes of metformin compared with insulin alone in pregnancy: a systematic review and meta-analysis. Diabet Med. 2017;34(1):27–36. https://doi.org/10.1111/dme.13150.
Syngelaki A, Nicolaides KH, Balani J, et al. Metformin versus placebo in obese pregnant women without diabetes mellitus. N Engl J Med. 2016;374(5):434–43. https://doi.org/10.1056/NEJMoa1509819.
• Romero R, Erez O, Hüttemann M, et al. Metformin, the aspirin of the 21st century: its role in gestational diabetes mellitus, prevention of preeclampsia and cancer, and the promotion of longevity. Am J Obstet Gynecol. 2017;217(3):282–302. https://doi.org/10.1016/j.ajog.2017.06.003. This review discusses the benefits of metformin for use in pregnancy outside of gestational diabetes treatment, along with the mechanisms by which it may be beneficial.
Hu J, Zhang J, Zhu B. Protective effect of metformin on a rat model of lipopolysaccharide-induced preeclampsia. Fundam Clin Pharmacol. 2019;33(6):649–58. https://doi.org/10.1111/fcp.12501.
Brownfoot FC, Hastie R, Hannan NJ, et al. Metformin as a prevention and treatment for preeclampsia: effects on soluble fms-like tyrosine kinase 1 and soluble endoglin secretion and endothelial dysfunction. Am J Obstet Gynecol. 2016;214(3):356.e1-356.e15. https://doi.org/10.1016/j.ajog.2015.12.019.
Cluver CA, Hiscock R, Decloedt EH, et al. Use of metformin to prolong gestation in preterm preeclampsia. Obstet Anesth Dig. 2022;42(3):135–6. https://doi.org/10.1097/01.aoa.0000853584.48469.4e.
Teng M, Khoo AL, Zhao YJ, et al. Meta-analysis of the effectiveness of esomeprazole in gastroesophageal reflux disease and Helicobacter pylori infection. J Clin Pharm Ther. 2015;40(4):368–75. https://doi.org/10.1111/jcpt.12277.
Saleh L, Samantar R, Garrelds IM, van den Meiracker AH, Visser W, Danser AHJ. Low soluble Fms-like tyrosine kinase-1, endoglin, and endothelin-1 levels in women with confirmed or suspected preeclampsia using proton pump inhibitors. Hypertension. 2017;70(3):594–600. https://doi.org/10.1161/HYPERTENSIONAHA.117.09741.
Onda K, Tong S, Beard S, et al. Proton pump inhibitors decrease soluble fms-like tyrosine kinase-1 and soluble endoglin secretion, decrease hypertension, and rescue endothelial dysfunction. Hypertension. 2017;69(3):457–68. https://doi.org/10.1161/HYPERTENSIONAHA.116.08408.
Kaitu’u-Lino TJ, Brownfoot FC, Beard S, et al. Combining metformin and esomeprazole is additive in reducing sFlt-1 secretion and decreasing endothelial dysfunction – implications for treating preeclampsia. PLoS One. 2018;13(2):e0188845. https://doi.org/10.1371/journal.pone.0188845.
• Cluver CA, Hannan NJ, van Papendorp E, et al. Esomeprazole to treat women with preterm preeclampsia: a randomized placebo controlled trial. Am J Obstet Gynecol. 2018;219(4):388.e1–388.e17. https://doi.org/10.1016/j.ajog.2018.07.019. This randomized placebo controlled trial of esomeprazole for the treatment of preterm preeclampsia did not find any associated difference in pregnancy prolongation or in markers of endothelial dysfunction.
Ornaghi S, Paidas MJ. Novel therapy for the treatment of early-onset preeclampsia. Clin Obstet Gynecol. 2017;60(1):169–82. https://doi.org/10.1097/GRF.0000000000000249.
Sharp A, Cornforth C, Jackson R, et al. Maternal sildenafil for severe fetal growth restriction (STRIDER): a multicentre, randomised, placebo-controlled, double-blind trial. Lancet Child Adolesc Health. 2018;2(2):93–102. https://doi.org/10.1016/S2352-4642(17)30173-6.
Levin G, Rottenstreich A. Sildenafil citrate in obstetrics – caution is advised. BJOG. 2019;126(6):736–736. https://doi.org/10.1111/1471-0528.15605.
Pels A, Derks J, Elvan-Taspinar A, et al. Maternal sildenafil vs placebo in pregnant women with severe early-onset fetal growth restriction: a randomized clinical trial. JAMA Netw Open. 2020;3(6): e205323. https://doi.org/10.1001/jamanetworkopen.2020.5323.
Turanov AA, Lo A, Hassler MR, et al. RNAi modulation of placental sFLT1 for the treatment of preeclampsia. Nat Biotechnol. 2018;36(12):1164–73. https://doi.org/10.1038/nbt.4297.
Robertson SA. Preventing preeclampsia by silencing soluble Flt-1? N Engl J Med. 2019;380(11):1080–2. https://doi.org/10.1056/NEJMcibr1817501.
Mcdougall AR, Tuttle A, Goldstein M, Ammerdorffer A, Gülmezoglu AM, Vogel JP. Target product profiles for novel medicines to prevent and treat preeclampsia: an expert consensus. PLOS Global Public Health. 2022;2(11): e0001260. https://doi.org/10.1371/journal.pgph.0001260.
Backes CH, Markham K, Moorehead P, Cordero L, Nankervis CA, Giannone PJ. Maternal preeclampsia and neonatal outcomes. J Pregnancy. 2011;2011:1–7. https://doi.org/10.1155/2011/214365.
Ghulmiyyah L, Sibai B. Maternal mortality from preeclampsia/eclampsia. Semin Perinatol. 2012;36(1):56–9. https://doi.org/10.1053/j.semperi.2011.09.011.
Funding
MMC is supported by a grant from The Eunice Kennedy Shriver National Institute of Child Health and Human Development (UG1HD027915) and the National Heart, Lung, and Blood Institute (UH3HL140131).
Eunice Kennedy Shriver National Institute of Child Health and Human Development,UG1HD027915,National Heart,Lung,and Blood Institute,UH3HL140131
Author information
Authors and Affiliations
Contributions
T.C.B. and D.K. contributed equally to the main manuscript creation and share co-leading authorship. M.M.C. contributed significant additions to the text and all authors reviewed the manuscript.
Corresponding author
Ethics declarations
Disclaimer
This commentary does not necessarily represent the official views of the NICHD, NHLBI, or the National Institute of Health.
Competing Interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any unpublished research involving human and animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bank, T.C., Kline, D. & Costantine, M.M. Challenges in Conducting Clinical Trials for Preeclampsia. Curr Hypertens Rep 26, 59–68 (2024). https://doi.org/10.1007/s11906-023-01276-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11906-023-01276-y