Abstract
Purpose of Review
Use of antihypertensives in older adults can be complicated by the potential for undesired effects on comorbidities, adverse effects of the drugs, and overall medication burden. The purpose of this two-part review is to discuss contemporary issues encountered in the management of hypertension in aged individuals, with a particular focus on the individualization of treatment. In part 1, we discuss the evaluation of the aged hypertensive patient and review the clinical trial evidence for treatment benefit of hypertension in the elderly.
Recent Findings
Elderly patients with suspected hypertension need careful evaluation of their blood pressure, as errors in measurement technique, inaccurate devices, or overreliance on office blood pressure readings may lead to under- or over-treatment, thereby increasing risks of adverse medication effects and/or cardiovascular events. Epidemiologic evidence in older adults suggests a link between low blood pressure and increased mortality. However, key prospective hypertension trials such as HYVET and SPRINT, which were focused in mostly healthy, community-dwelling elderly cohorts, have unequivocally demonstrated benefits of lowering blood pressure in reducing cardiovascular events in the very elderly. Recent evidence also suggests benefit in reducing the risks of cognitive impairment.
Summary
Hypertension is a major modifiable risk factor and the benefits of treatment in lowering cardiovascular events are realized for most individuals, even at advanced ages.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
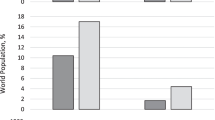
NCD Risk Factor Collaboration. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389(10064):37–55.
Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310(9):959–68.
Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT Jr, et al. Potential U.S. population impact of the 2017 ACC/AHA high blood pressure guideline. J Am Coll Cardiol. 2018;71(2):109–18.
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–23.
Franklin SS, Gustin W, Wong ND, Larson MG, Weber MA, Kannel WB, et al. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation. 1997;96(1):308–15.
O’Rourke MF. From theory into practice: arterial haemodynamics in clinical hypertension. J Hypertens. 2002;20(10):1901–15.
• Lv YB, Gao X, Yin ZX, Chen HS, Luo JS, Brasher MS, et al. Revisiting the association of blood pressure with mortality in oldest old people in China: community based, longitudinal prospective study. BMJ. 2018;361:k2158. In this large cohort of 144,403 participants aged 80 years and older, systolic blood pressure trajectories showed an accelerated decline in the last 2 years of life which did not appear due to intensification of antihypertensive therapy. This suggests that epidemiological associations of low systolic BP with higher mortality may be due to reverse causation bias.
Delgado J, Bowman K, Ble A, Masoli J, Han Y, Henley W, et al. Blood pressure trajectories in the 20 years before death. JAMA Intern Med. 2018;178(1):93–9.
Ravindrarajah R, Hazra NC, Hamada S, Charlton J, Jackson SHD, Dregan A, et al. Systolic blood pressure trajectory, frailty, and all-cause mortality >80 years of age: cohort study using electronic health records. Circulation. 2017;135(24):2357–68.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13–e115.
Messerli FH, Ventura HO, Amodeo C. Osler’s maneuver and pseudohypertension. N Engl J Med. 1985;312(24):1548–51.
Tsapatsaris NP, Napolitana GT, Rothchild J. Osler’s maneuver in an outpatient clinic setting. Arch Intern Med. 1991;151(11):2209–11.
Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I, et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Auton Neurosci. 2011;161(1–2):46–8.
Gupta V, Lipsitz LA. Orthostatic hypotension in the elderly: diagnosis and treatment. Am J Med. 2007;120(10):841–7.
Gibbons CH, Schmidt P, Biaggioni I, Frazier-Mills C, Freeman R, Isaacson S, et al. The recommendations of a consensus panel for the screening, diagnosis, and treatment of neurogenic orthostatic hypotension and associated supine hypertension. J Neurol. 2017;264(8):1567–82.
Bulpitt CJ, Beckett N, Peters R, Staessen JA, Wang JG, Comsa M, et al. Does white coat hypertension require treatment over age 80?: results of the hypertension in the very elderly trial ambulatory blood pressure side project. Hypertension. 2013;61(1):89–94.
Cacciolati C, Hanon O, Alperovitch A, Dufouil C, Tzourio C. Masked hypertension in the elderly: cross-sectional analysis of a population-based sample. Am J Hypertens. 2011;24(6):674–80.
Veterans Administration Cooperative Study Group on Antihypertensive Agents. Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg. JAMA. 1967;202(11):1028–34.
Amery A, Birkenhager W, Brixko P, Bulpitt C, Clement D, Deruyttere M, et al. Mortality and morbidity results from the European Working Party on High Blood Pressure in the Elderly trial. Lancet. 1985;1(8442):1349–54.
Dahlof B, Lindholm LH, Hansson L, Schersten B, Ekbom T, Wester PO. Morbidity and mortality in the Swedish Trial in Old Patients with Hypertension (STOP-Hypertension). Lancet. 1991;338(8778):1281–5.
SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 1991;265(24):3255–64.
Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhager WH, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) trial investigators. Lancet. 1997;350(9080):757–64.
JATOS Study Group. Principal results of the Japanese trial to assess optimal systolic blood pressure in elderly hypertensive patients (JATOS). Hypertens Res 2008;31(12):2115–2127.
Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887–98.
Verdecchia P, Staessen JA, Angeli F, de Simone G, Achilli A, Ganau A, et al. Usual versus tight control of systolic blood pressure in non-diabetic patients with hypertension (Cardio-Sis): an open-label randomised trial. Lancet 2009;374(9689):525–533
Ogihara T, Saruta T, Rakugi H, Matsuoka H, Shimamoto K, Shimada K, et al. Target blood pressure for treatment of isolated systolic hypertension in the elderly: valsartan in elderly isolated systolic hypertension study. Hypertension 2010;56(2):196–202.
•• Williamson JD, Supiano MA, Applegate WB, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016;315(24):2673–82. This pre-planned analysis of patients ≥ 75 years of age that were enrolled in SPRINT found that an intensive SBP goal of < 120 mmHg decreased the primary cardiovascular composite outcome as well as all-cause mortality compared with the standard SBP goal of < 140 mmHg in ambulatory, community-dwelling seniors.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–20.
Wright JT Jr, Fine LJ, Lackland DT, Ogedegbe G, Dennison Himmelfarb CR. Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view. Ann Intern Med. 2014;160(7):499–503.
Sprint Research Group, Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–16.
• SPRINT MIND Investigators for the SPRINT Research Group. Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA. 2019;321(6):553–61. This sub-study of SPRINT found that treating to an intensive SBP goal of < 120 mmHg was associated with a decreased risk of mild cognitive impairment and the combined rate of mild cognitive impairment or probable dementia. While there was no decrease in the primary cognitive outcome of adjudicated dementia, it is important to note that this outcome was likely underpowered as SPRINT was stopped early and there were fewer cases of dementia than expected.
Nasrallah IM, Pajewski NM, Auchus AP, Chelune G, Cheung AK, Cleveland ML; 2 SPRINT MIND Investigators for the SPRINT Research Group. Association of intensive vs standard blood pressure control with cererbral white matter lesions. JAMA 2019;322(6):524–534.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Antihypertensive Agents: Mechanisms of Drug Action
Rights and permissions
About this article
Cite this article
MacLaughlin, E.J., Ernst, M.E. From Clinical Trials to Bedside: the Use of Antihypertensives in Aged Individuals. Part 1: Evaluation and Evidence of Treatment Benefit. Curr Hypertens Rep 21, 82 (2019). https://doi.org/10.1007/s11906-019-0987-y
Published:
DOI: https://doi.org/10.1007/s11906-019-0987-y