Abstract
Many antihypertensive drugs are now available in generic formulations at fractions of the cost of their branded counterparts. In the United States, marketing approval for generic medications is usually granted by the Food and Drug Administration on the basis of two simple studies involving dissolution rates and bioavailability in 24 – 36 healthy people, without data regarding antihypertensive efficacy, safety, or long-term outcomes. This process leaves many true disciples of “Evidence-Based Medicine” in a quandary: prescribe only brand-name medications that have been demonstrated in clinical trials to both lower blood pressure and prevent cardiovascular events, or instead recommend lower-priced generic agents that are usually supported by no such data. This review summarizes the current evidence that generic antihypertensive drugs are likely to be safe and effective, may increase the probability of medication availability and adherence for many patients, but, by law, must have a different physical appearance than the original product.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Hoyert DL, Zu J. Deaths: Preliminary data for 2011. National Vital Statistics Reports. 2012;61:1–52. Available on the internet at: http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_06.pdf, accessed 26 FEB 13. The most recent US national data about cause of death (gathered from death certificates) suggest that cardiovascular disease will likely lose its #1 position to cancer in 2013.
•• Go AS, Mazaffarian D, Roger VL, et al. Heart disease and stroke statistics—2013 update: A report from the American heart association. Circulation. 2013;127:e6–e245. Available on the internet at: http://www.circ.ahajournal.org/content/127/1/e6, accessed 26 FEB 13. The most up-to-date compilation of data regarding the epidemiology of cardiovascular disease (and its risk factors) in the US.
Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment and control of hypertension: 1998–2008. JAMA. 2010;303:2043–50.
Vital signs: Awareness and treatment of uncontrolled hypertension among adults—United States, 2003–2010. MMWR 2012;61(35):703–9. Available on the internet at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6135a3.htm, accessed 26 FEB 13.
• Hypertension: Clinical management of primary hypertension in adults. NICE Clinical Guideline 127, issued August 2011. Available on the internet at: http://www.guidance.nice.org.uk/CG127, accessed 26 FEB 13. The last three sets of British NICE guidelines are based on pharmacoeconomic analyses, and the most recent dataset shows a very large reduction in the cost of antihypertensive medications to the British National Health Service.
Centers for Medicare and Medicaid Services. National Health Expenditure Projections 2010–2020. National Health Care Expenditure Data. Available on the internet at: https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/downloads/proj2010.pdf, accessed 18 MAR 13.
Abbreviated New Drug Application (ANDA): Generics. U.S. Food and Drug Administration. Last Updated 01/04/2013. Available on the Internet at: http://www.fda.gov/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/ApprovalApplications/AbbreviatedNewDrugApplicationANDAGenerics/default.htm, accessed 18 MAR 13.
Carter BL. Equivalence of generic and brand-name drugs for cardiovascular disease [Letter]. JAMA. 2009;301:1654.
Meredith PA. Potential concerns about generic substitution: Bioequivalence versus therapeutic equivalence of different amlodipine salt forms. Curr Med Res Opin. 2009;25:2179–89.
• Woodcock J, Khan M, Yu LX. Withdrawal of generic budeprion for nonbioequivalence. N Engl J Med. 2012;367:2463–5. Perhaps the most recent example of official FDA actions that resulted in removal of a nonbioequivalent drug product from the US market.
Orange Book: Approved drug products with therapeutic equivalence evaluations. Available on the Internet at: http://www.accessdata.fda.gov/scripts/cder/ob/default.cmf, accessed 26 FEB 13.
Kesselheim AS, Misono AS, Lee JL, et al. Clinical equivalence of generic and brand-name drugs used in cardiovascular disease: a systematic review and meta-analysis. JAMA. 2008;300:2514–26.
Black HR, Elliott WJ, Grandits G, CONVINCE Research Group, et al. Principal results of the Controlled Onset Verapamil Investigation of Cardiovascular Endpoints (CONVINCE) trial. JAMA. 2003;289:2073–82.
Pepine CJ, Handberg EM, Cooper-DeHoff RM, et al. A calcium antagonist vs. A non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease: The International Verapamil-Trandolapril Study (INVEST): a randomized controlled trial. The INVEST investigators. JAMA. 2003;290:2805–16.
The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs. Diuretic: The Antihypertensive and Lipid Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288:2981–97.
Davis BR, Cutler JA, Gordon DJ, et al. Rationale and design for the Antihypertensive and Lipid Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Am J Hypertens. 1996;9:342–60.
Elliott WJ. ALLHAT: The largest and most important blood pressure trial ever in the USA [editorial]. Am J Hypertension. 1996;9:409–11.
Materson BJ, Reda DJ, Cushman WC, Massie BM, Freis ED, Kochar MS, et al. Single-drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. N Engl J Med. 1993;328:914–21.
Gagne JJ, Avorn J, Shrank WH, Schneeweiss S. Refilling and switching of antiepileptic drugs and seizure-related events. Clin Pharmacol Ther. 2010;88:347–53.
Moore N, Berdaï D, Bégaud B. Are generic drugs really inferior medicines? Clin Pharmacol Ther. 2010;88:302–4.
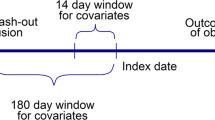
•• Cummings DM, Letter AJ, Howard G, et al. Generic medications and blood pressure control in diabetic hypertensive subjects: Results from the REasons for geographic and racial differences in stroke (REGARDS) study. Diabetes Care. 2013;36:591–7. After adjustment for baseline covariates, no significant relationship was seen between generic antihypertensive drug use and blood pressure control in this cross-sectional study involving 5,375 diabetics between 2003 and 2007.
World Health Orgainization. Adherence to long-term therapies: evidence for action. 2003. Available on the internet at: http://www.who.int/chp/knowledge/publications/adherence_report/en/ , accessed 17 MAR 13.
Cutler DM, Everett W. Thinking outside the pillbox–medication adherence as a priority for health care reform. N Engl J Med. 2010;362:1553–5.
• Viswanathan M, Golin CE, Jones CD, et al. Interventions to improve adherence to self-administered medications for chronic diseases in the united states: A systematic review. Ann Intern Med. 2012;157:785–95. A systematic review found 62 trials, 4 observational studies, and 1 trial of policy intervention that evaluated the effects of reduced medication copayments or improved prescription drug coverage; hypertension was but one therapeutic area in which such interventions improved medication adherence, but whether this directly improves outcomes is still an open question.
Briesacher BA, Andrade SE, Fouayzi H, Chan KA. Medication adherence and use of generic drug therapies. Am J Manag Care. 2009;15:450–6.
• Kesselheim AS, Misono AS, Shrank WH, et al. Variations in pill appearance of antiepileptic drugs and the risk of nonadherence. JAMA Intern Med. 2013;173:202–8. In a case–control study of 11,472 patients who were non-persistent with their antiepileptic drug therapy and 50,050 controls that maintained therapy, changes in the appearance of the pills was associated with a 53 % higher risk of non-persistence.
Yu LX, Geba GP. Generic pills from the patient perspective: Comment on “variations in pill appearance of antiepileptic drugs and the risk of nonadherence.” JAMA Intern Med. 2013;173:208–9.
• Campbell EG, Pham-Kanter G, Vogeli C, Iezzoni LI. Physician acquiescence to patient demands for brand-name drugs: Results of a national survey of physicians [research letter]. JAMA Intern Med. 2013;173:237–9. A national survey of 1891 physicians identified several behaviors of physicians who sometimes or often prescribed branded medications at the request of patients, including several measures of closer relationships with the pharmaceutical industry.
Conflict of Interest
R.M. Cooper-DeHoff declares that she has no conflict of interest.
W.J. Elliott has received research support from Forest Research Institute, payment for lectures including service on speakers’ bureaus from Forest Laboratories, and royalties from Elsevier.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Cooper-DeHoff, R.M., Elliott, W.J. Generic Drugs for Hypertension: Are They Really Equivalent?. Curr Hypertens Rep 15, 340–345 (2013). https://doi.org/10.1007/s11906-013-0353-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11906-013-0353-4