Abstract
Purpose of Review
Artificial Intelligence (AI) has the potential to transform detection and management of nutrition-related complications through advances in wearable technology, mobile applications, and machine learning. The literature, however, lacks studies specific to the interplay between AI and nutrition in patients with liver disease. The aim of this article is to address the current state of AI in nutrition and metabolic liver disease. We seek to understand how AI can be utilized to address gaps in the care of patients with liver disease, particularly as it relates to their nutrition.
Recent Findings
Advances in AI, particularly in deep learning, have led to improved performance of diagnostic and prognostic models across many disease processes. AI-based systems in this realm include predictive modeling, natural language processing (NLP), and image recognition.
Summary
Ultimately, large-scale studies are needed to validate the use of AI in assessing and improving nutrition in this population.



Similar content being viewed by others
Abbreviations
- NAFLD:
-
Non-alcoholic fatty liver disease
- NASH:
-
Non-alcoholic steatohepatitis
- MAFLD:
-
Metabolic dysfunction-associated fatty liver disease
- AI:
-
Artificial intelligence
- SGA:
-
Subjective global assessment
- BIA:
-
Bioimpedance analysis
- HgbA1c:
-
Hemoglobin A1c
- MLA:
-
Machine learning algorithms
- CNN:
-
Convolutional neural networks
- NLP:
-
Natural language processing
- SVM:
-
Support vector machines
- ANN:
-
Artificial neural networks
- HCC:
-
Hepatocellular carcinoma
- CT:
-
Computed tomography
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Samuel VT, Shulman GI. Nonalcoholic fatty liver disease as a nexus of metabolic and hepatic diseases. Cell Metab. 2018;27(1):22–41.
Chen Z, Qin H, Qiu S, Chen G, Chen Y. Correlation of triglyceride to high-density lipoprotein cholesterol ratio with nonalcoholic fatty liver disease among the non-obese Chinese population with normal blood lipid levels: a retrospective cohort research. Lipids Health Dis. 2019;18(1):162.
Lallukka S, Yki-Järvinen H. Non-alcoholic fatty liver disease and risk of type 2 diabetes. Best Pract Res Clin Endocrinol Metab. 2016;30(3):385–95.
Buchard B, Boirie Y, Cassagnes L, Lamblin G, Coilly A, Abergel A. Assessment of malnutrition, sarcopenia and frailty in patients with cirrhosis: which tools should we use in clinical practice? Nutrients. 2020;12(1):186.
Traub J, Reiss L, Aliwa B, Stadlbauer V. Malnutrition in patients with liver cirrhosis. Nutrients. 2021;13(2):540.
Bruch JP, Álvares DASMR, Alves BC, Dall’alba V. Reduced hand grip strength in overweight and obese chronic hepatitis c patients. Arq Gastroenterol. 2016;53(1):31–5.
Meyer F, Bannert K, Wiese M, Esau S, Sautter LF, Ehlers L, et al. Molecular mechanism contributing to malnutrition and sarcopenia in patients with liver cirrhosis. Int J Mol Sci. 2020;21(15):5357.
Patel A, Silverman S, Baghdadi J, Shah O, Sundaram V. Osteoporotic fracture risk and health care burden in patients with cirrhosis. J Clin Gastroenterol. 2019;53(7):543–8.
Sam J, Nguyen GC. Protein-calorie malnutrition as a prognostic indicator of mortality among patients hospitalized with cirrhosis and portal hypertension. Liver Int. 2009;29(9):1396–402.
McFarlane M, Hammond C, Roper T, Mukarati J, Ford R, Burrell J, et al. Comparing assessment tools for detecting undernutrition in patients with liver cirrhosis. Clin Nutr ESPEN. 2018;23:156–61.
•• Maharshi S, Sharma BC, Srivastava S. Malnutrition in cirrhosis increases morbidity and mortality. J Gastroenterol Hepatol. 2015;30(10):1507–13. Prevalence of malnutrition is high in patients with cirrhosis. It is associated with increased complications and mortality.
Manne V, Saab S. Impact of nutrition and obesity on chronic liver disease. Clin Liver Dis. 2014;18(1):205–18.
Vieira PM, De-Souza DA, Oliveira LC. Nutritional assessment in hepatic cirrhosis; clinical, anthropometric, biochemical and hematological parameters. Nutr Hosp. 2013;28(5):1615–21.
Chaudhry A, Toori KU, Shaikh JI. To determine correlation between biochemical parameters of nutritional status with disease severity in HCV related liver cirrhosis. Pak J Med Sci. 2018;34(1):154–8.
Naqvi IH, Mahmood K, Salekeen S, Akhter ST. Determining the frequency and severity of malnutrition and correlating it with the severity of liver cirrhosis. Turk J Gastroenterol. 2013;24(5):415–22.
Ruiz-Margáin A, Macías-Rodríguez RU, Ampuero J, Cubero FJ, Chi-Cervera L, Ríos-Torres SL, et al. Low phase angle is associated with the development of hepatic encephalopathy in patients with cirrhosis. World J Gastroenterol. 2016;22(45):10064–70.
Bunchorntavakul C, Supanun R, Atsawarungruangkit A. Nutritional status and its impact on clinical outcomes for patients admitted to hospital with cirrhosis. J Med Assoc Thai. 2016;99(Suppl 2):S47-55.
Ribeiro HS, Maurício SF, Antônio da Silva T, de Vasconcelos Generoso S, Lima AS, Toulson Davisson Correia MI. Combined nutritional assessment methods to predict clinical outcomes in patients on the waiting list for liver transplantation. Nutrition. 2018;47:21–6.
Lindqvist C, Majeed A, Wahlin S. Body composition assessed by dual-energy X-ray absorptiometry predicts early infectious complications after liver transplantation. J Hum Nutr Diet. 2017;30(3):284–91.
García-Rodríguez MT, López-Calviño B, Piñón-Villar MDC, Otero-Ferreiro A, Suárez-López F, Gómez-Gutiérrez M, et al. Concordance among methods of nutritional assessment in patients included on the waiting list for liver transplantation. J Epidemiol. 2017;27(10):469–75.
Mesejo A, Juan M, Serrano A. Liver cirrhosis and encephalopathy: clinical and metabolic consequences and nutritional support. Nutr Hosp. 2008;23(Suppl 2):8–18.
Yao CK, Fung J, Chu NHS, Tan VPY. Dietary Interventions in Liver Cirrhosis. J Clin Gastroenterol. 2018;52(8):663–73.
Jensen GL, Compher C, Sullivan DH, Mullin GE. Recognizing malnutrition in adults: definitions and characteristics, screening, assessment, and team approach. JPEN J Parenter Enteral Nutr. 2013;37(6):802–7.
Iwasa M, Iwata K, Hara N, Hattori A, Ishidome M, Sekoguchi-Fujikawa N, et al. Nutrition therapy using a multidisciplinary team improves survival rates in patients with liver cirrhosis. Nutrition. 2013;29(11–12):1418–21.
Maharshi S, Sharma BC, Sachdeva S, Srivastava S, Sharma P. Efficacy of nutritional therapy for patients with cirrhosis and minimal hepatic encephalopathy in a randomized trial. Clin Gastroenterol Hepatol. 2016;14(3):454–60.e3; quiz e33.
Manguso F, D’Ambra G, Menchise A, Sollazzo R, D’Agostino L. Effects of an appropriate oral diet on the nutritional status of patients with HCV-related liver cirrhosis: a prospective study. Clin Nutr. 2005;24(5):751–9.
Dinani AM, Kowdley KV, Noureddin M. Application of artificial intelligence for diagnosis and risk stratification in NAFLD and NASH: the state of the art. Hepatology. 2021;74(4):2233–40.
Kenner B, Chari ST, Kelsen D, Klimstra DS, Pandol SJ, Rosenthal M, et al. Artificial intelligence and early detection of pancreatic cancer: 2020 summative review. Pancreas. 2021;50(3):251–79.
Ahn JC, Connell A, Simonetto DA, Hughes C, Shah VH. Application of artificial intelligence for the diagnosis and treatment of liver diseases. Hepatology. 2021;73(6):2546–63.
• Côté M, Lamarche B. Artificial intelligence in nutrition research: perspectives on current and future applications. Appl Physiol Nutr Metab. 2021:1–8. This article provides an overview of the main and latest applications of AI in nutrition research.
•• Limketkai BN, Mauldin K, Manitius N, Jalilian L, Salonen BR. The age of artificial intelligence: use of digital technology in clinical nutrition. Curr Surg Rep. 2021;9(7):20. This review discusses the implementation of AI for nutrition, highlighting mobile apps, wearable technologies, and machine learning and how these tools have translated into clinical practice.
Foster KR, Torous J. The opportunity and obstacles for smartwatches and wearable sensors. IEEE Pulse. 2019;10(1):22–5.
King CE, Sarrafzadeh M. A survey of smartwatches in remote health monitoring. J Healthc Inform Res. 2018;2(1–2):1–24.
Blaauw FJ, Schenk HM, Jeronimus BF, van der Krieke L, de Jonge P, Aiello M, et al. Let’s get Physiqual - An intuitive and generic method to combine sensor technology with ecological momentary assessments. J Biomed Inform. 2016;63:141–9.
Boushey CJ, Spoden M, Zhu FM, Delp EJ, Kerr DA. New mobile methods for dietary assessment: review of image-assisted and image-based dietary assessment methods. Proc Nutr Soc. 2017;76(3):283–94.
Eldridge AL, Piernas C, Illner AK, Gibney MJ, Gurinović MA, de Vries JHM, et al. Evaluation of new technology-based tools for dietary intake assessment-an ILSI Europe dietary intake and exposure task force evaluation. Nutrients. 2018;11(1):55.
Sun M, Burke LE, Mao ZH, Chen Y, Chen HC, Bai Y, et al. eButton: A wearable computer for health monitoring and personal assistance. Proc Des Autom Conf. 2014;2014:1–6.
Ji Y, Plourde H, Bouzo V, Kilgour RD, Cohen TR. Validity and usability of a smartphone image-based dietary assessment app compared to 3-day food diaries in assessing dietary intake among canadian adults: randomized controlled trial. JMIR Mhealth Uhealth. 2020;8(9): e16953.
Ceci L. Number of mHealth apps available in the Google Play Store from 1st quarter 2015 to 2nd quarter 2022. Statista. 2022.
Veazie S, Winchell K, Gilbert J, Paynter R, Ivlev I, Eden K, et al. AHRQ comparative effectiveness technical briefs. Mobile applications for self-management of diabetes. Rockville (MD): Agency for Healthcare Research and Quality (US); 2018.
Van Deen WK, van der Meulen-de Jong AE, Parekh NK, Kane E, Zand A, DiNicola CA, et al. Development and validation of an inflammatory bowel diseases monitoring index for use with mobile health technologies. Clin Gastroenterol Hepatol. 2016;14(12):1742-50.e7.
Atreja A, Khan S, Rogers JD, Otobo E, Patel NP, Ullman T, et al. Impact of the mobile HealthPROMISE platform on the quality of care and quality of life in patients with inflammatory bowel disease: study protocol of a pragmatic randomized controlled trial. JMIR Res Protoc. 2015;4(1): e23.
Zeevi D, Korem T, Zmora N, Israeli D, Rothschild D, Weinberger A, et al. Personalized nutrition by prediction of glycemic responses. Cell. 2015;163(5):1079–94.
• Van Vleck TT, Chan L, Coca SG, Craven CK, Do R, Ellis SB, et al. Augmented intelligence with natural language processing applied to electronic health records for identifying patients with non-alcoholic fatty liver disease at risk for disease progression. Int J Med Inform. 2019;129:334–41. Authors examined the utility of NLP for the identification of patients with NAFLD, to assess patterns of disease progression, and to identify gaps in care related to breakdowns in communication among provider.
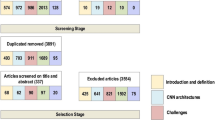
•• Balsano C, Alisi A, Brunetto MR, Invernizzi P, Burra P, Piscaglia F. The application of artificial intelligence in hepatology: a systematic review. Dig Liver Dis. 2022;54(3):299–308. This is a systematic review on the applications of AI to hepatology, highlighting the current challenges and crucial issues related to the use of such technologies.
• Nam D, Chapiro J, Paradis V, Seraphin TP, Kather JN. Artificial intelligence in liver diseases: Improving diagnostics, prognostics and response prediction. JHEP Rep. 2022;4(4):100443. This article summarizes the state of the art in AI in hepatology with a particular focus on histopathology and radiology data.
Poon AIF, Sung JJY. Opening the black box of AI-Medicine. J Gastroenterol Hepatol. 2021;36(3):581–4.
Huisman EJ, Trip EJ, Siersema PD, van Hoek B, van Erpecum KJ. Protein energy malnutrition predicts complications in liver cirrhosis. Eur J Gastroenterol Hepatol. 2011;23(11):982–9.
Montano-Loza AJ, Meza-Junco J, Prado CM, Lieffers JR, Baracos VE, Bain VG, et al. Muscle wasting is associated with mortality in patients with cirrhosis. Clin Gastroenterol Hepatol. 2012;10(2):166–73, 73.e1.
Fialla AD, Israelsen M, Hamberg O, Krag A, Gluud LL. Nutritional therapy in cirrhosis or alcoholic hepatitis: a systematic review and meta-analysis. Liver Int. 2015;35(9):2072–8.
Putadechakum S, Klangjareonchai T, Soponsaritsuk A, Roongpisuthipong C. Nutritional status assessment in cirrhotic patients after protein supplementation. ISRN Gastroenterol. 2012;2012: 690402.
Ney M, Vandermeer B, van Zanten SJ, Ma MM, Gramlich L, Tandon P. Meta-analysis: oral or enteral nutritional supplementation in cirrhosis. Aliment Pharmacol Ther. 2013;37(7):672–9.
Plauth M, Cabré E, Riggio O, Assis-Camilo M, Pirlich M, Kondrup J, et al. ESPEN guidelines on enteral nutrition: liver disease. Clin Nutr. 2006;25(2):285–94.
Yin L, Song C, Cui J, Lin X, Li N, Fan Y, et al. A fusion decision system to identify and grade malnutrition in cancer patients: machine learning reveals feasible workflow from representative real-world data. Clin Nutr. 2021;40(8):4958–70.
Bischoff SC, Escher J, Hébuterne X, Kłęk S, Krznaric Z, Schneider S, et al. ESPEN practical guideline: clinical nutrition in inflammatory bowel disease. Clin Nutr. 2020;39(3):632–53.
Wang NC, Zhang P, Tapper EB, Saini S, Wang SC, Su GL. Automated measurements of muscle mass using deep learning can predict clinical outcomes in patients with liver disease. Am J Gastroenterol. 2020;115(8):1210–6.
Zou WY, Enchakalody BE, Zhang P, Shah N, Saini SD, Wang NC, et al. Automated measurements of body composition in abdominal ct scans using artificial intelligence can predict mortality in patients with cirrhosis. Hepatol Commun. 2021;5(11):1901–10.
Subhi Y, Bube SH, Rolskov Bojsen S, Skou Thomsen AS, Konge L. Expert involvement and adherence to medical evidence in medical mobile phone apps: a systematic review. JMIR Mhealth Uhealth. 2015;3(3): e79.
Tabi K, Randhawa AS, Choi F, Mithani Z, Albers F, Schnieder M, et al. Mobile apps for medication management: review and analysis. JMIR Mhealth Uhealth. 2019;7(9): e13608.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Both malnutrition and obesity play a role in the development and progression of liver disease and related complications.
• Malnutrition is a common complication of liver cirrhosis and is associated with poor outcomes.
• Understanding what interventions have been shown to be efficacious in addressing malnutrition in cirrhosis will assist in the development of AI technology customized to address the problem at hand.
• Using AI for nutritional purposes in the general population and in disease-specific states is promising, but more research is needed to improve and validate algorithms.
• While there are barriers to the use of wearable technologies, mobile apps, and machine learning algorithms, they can provide real-time information and provide data allowing for appropriate clinical intervention.
• There is enormous potential of AI in collecting data that physicians can use to inform healthcare decisions. There is a need for future AI interventions to address nutrition in patients with liver disease and to improve patient health outcomes.
This article is part of the Topical Collection on Nutrition
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schmidt, K.A., Penrice, D.D. & Simonetto, D.A. Artificial Intelligence in the Assessment and Management of Nutrition and Metabolism in Liver Disease. Curr Hepatology Rep 21, 120–130 (2022). https://doi.org/10.1007/s11901-022-00594-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11901-022-00594-0