Abstract
Purpose of Review
Frailty in end-stage liver disease is a risk factor for mortality and other serious complications for transplant-waitlist patients. Multiple interventions have been studied to try to mitigate these effects by targeting contributors to frailty, most notably sarcopenia and hepatic encephalopathy. This review provides an evidence-based summary of interventions that have been recommended to prevent or reverse frailty and its contributors.
Recent Findings
Current nutritional recommendations for frailty in end-stage liver disease focus on mitigating the effects of ammonia toxicity, increased energy expenditure due to shifts in glucose metabolism, and micronutrient deficiency and supplementation.
Summary
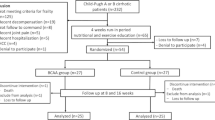
Data regarding targeted nutritional interventions for frailty in cirrhosis are limited. Current evidence supports increasing caloric intake, increasing protein intake, avoiding a fasting state, branched-chain amino acid supplementation, screening for and treating vitamin D deficiency, and to a lesser extent l-carnitine supplementation. Future randomized controlled trials are necessary to validate these interventions as modifiers of frailty.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–56.
Xue Q-L. The frailty syndrome: definition and natural history. Clin Geriatr Med. 2011;27:1–15.
Lai JC, Feng S, Terrault NA, Lizaola B, Hayssen H, Covinsky K. Frailty predicts waitlist mortality in liver transplant candidates: frailty in liver transplant candidates. Am J Transplant. 2014;14:1870–9.
Dunn MA, Josbeno DA, Tevar AD, Rachakonda V, Ganesh SR, Schmotzer AR, et al. Frailty as tested by gait speed is an independent risk factor for cirrhosis complications that require hospitalization. Am J Gastroenterol. 2016;111:1768–75.
• Lai JC, Sonnenday CJ, Tapper EB, Duarte-Rojo A, Dunn MA, Bernal W, et al. Frailty in liver transplantation: an expert opinion statement from the American Society of Transplantation Liver and Intestinal Community of Practice. Am J Transplant. 2019;19:1896–906 An opinion statement released by experts in the field of frailty in end-stage liver disease advocating for the measurement of frailty in all liver transplant candidates using a standardized tool. Experts also advocated for the use of frailty to guide nutritional interventions and physical therapy, incorporating frailty in determining suitability for transplant, and future areas of research.
Tapper EB, Finkelstein D, Mittleman MA, Piatkowski G, Lai M. Standard assessments of frailty are validated predictors of mortality in hospitalized patients with cirrhosis: liver failure/cirrhosis/portal hypertension. Hepatology. 2015;62:584–90.
Montano-Loza AJ, Meza-Junco J, Baracos VE, Prado CMM, Ma M, Meeberg G, et al. Severe muscle depletion predicts postoperative length of stay but is not associated with survival after liver transplantation: sarcopenia after liver transplantation. Liver Transpl. 2014;20:640–8.
Englesbe MJ, Patel SP, He K, Lynch RJ, Schaubel DE, Harbaugh C, et al. Sarcopenia and mortality after liver transplantation. J Am Coll Surg. 2010;211:271–8.
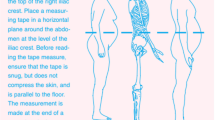
Carey EJ, Lai JC, Wang CW, Dasarathy S, Lobach I, Montano-Loza AJ, et al. A multicenter study to define sarcopenia in patients with end-stage liver disease. Liver Transpl. 2017;23:625–33.
Tapper EB, Derstine B, Baki J, Su GL. Bedside measures of frailty and cognitive function correlate with sarcopenia in patients with cirrhosis. Dig Dis Sci. 2019;64(12):3652–9.
Tapper EB, Konerman M, Murphy S, Sonnenday CJ. Hepatic encephalopathy impacts the predictive value of the Fried Frailty Index. Am J Transplant. 2018;18:2566–70.
Lai JC, Covinsky KE, Dodge JL, Boscardin WJ, Segev DL, Roberts JP, et al. Development of a novel frailty index to predict mortality in patients with end-stage liver disease. Hepatology. 2017;66:564–74.
• Amodio P, Bemeur C, Butterworth R, Cordoba J, Kato A, Montagnese S, et al. The nutritional management of hepatic encephalopathy in patients with cirrhosis: International Society for Hepatic Encephalopathy and Nitrogen Metabolism Consensus. Hepatology. 2013;58:325–36 Evidence-based guidelines for nutritional interventions in patients with hepatic encephalopathy.
• Merli M, Berzigotti A, Zelber-Sagi S, Dasarathy S, Montagnese S, Genton L, et al. EASL clinical practice guidelines on nutrition in chronic liver disease. J Hepatol. 2019;70:172–93 Nutritional guidelines for patients with chronic liver disease. Presents evidence-based recommendations for patients with chronic liver disease, cirrhosis, and specific comorbidities such as hepatic encephalopathy, patients with concurrent bone disease, and critically ill cirrhotic patients.
Carey EJ, Lai JC, Sonnenday C, Tapper EB, Tandon P, Duarte-Rojo A, et al. A North American expert opinion statement on sarcopenia in liver transplantation. Hepatology. 2019;70(5):1816–29.
Greco AV, Mingrone G, Benedetti G, Capristo E, Tataranni PA, Gasbarrini G. Daily energy and substrate metabolism in patients with cirrhosis. Hepatology. 1998;27:346–50.
Dasarathy S, Merli M. Sarcopenia from mechanism to diagnosis and treatment in liver disease. J Hepatol. 2016;65:1232–44.
Tsien CD, McCullough AJ, Dasarathy S. Late evening snack: exploiting a period of anabolic opportunity in cirrhosis. J Gastroenterol Hepatol. 2012;27:430–41.
Montano-Loza AJ, Angulo P, Meza-Junco J, Prado CMM, Sawyer MB, Beaumont C, et al. Sarcopenic obesity and myosteatosis are associated with higher mortality in patients with cirrhosis. J Cachexia Sarcopenia Muscle. 2016;7:126–35.
Everhart JE, Lok AS, Kim H-Y, Morgan TR, Lindsay KL, Chung RT, et al. Weight-related effects on disease progression in the hepatitis C antiviral long-term treatment against cirrhosis trial. Gastroenterology. 2009;137:549–57.
Guo Y-J, Tian Z-B, Jiang N, Ding X-L, Mao T, Jing X. Effects of late evening snack on cirrhotic patients: a systematic review and meta-analysis. Gastroenterol Res Pract. 2018;2018:9189062.
Fukushima H, Miwa Y, Ida E, Kuriyama S, Toda K, Shimomura Y, et al. Nocturnal branched-chain amino acid administration improves protein metabolism in patients with liver cirrhosis: comparison with daytime administration. JPEN J Parenter Enteral Nutr. 2003;27:315–22.
Yamanaka-Okumura H, Nakamura T, Takeuchi H, Miyake H, Katayama T, Arai H, et al. Effect of late evening snack with rice ball on energy metabolism in liver cirrhosis. Eur J Clin Nutr. 2006;60:1067–72.
Nakaya Y, Okita K, Suzuki K, Moriwaki H, Kato A, Miwa Y, et al. BCAA-enriched snack improves nutritional state of cirrhosis. Nutrition. 2007;23:113–20.
Korenaga K, Korenaga M, Uchida K, Yamasaki T, Sakaida I. Effects of a late evening snack combined with alpha-glucosidase inhibitor on liver cirrhosis. Hepatol Res. 2008;38:1087–97.
Plank LD, Gane EJ, Peng S, Muthu C, Mathur S, Gillanders L, et al. Nocturnal nutritional supplementation improves total body protein status of patients with liver cirrhosis: a randomized 12-month trial. Hepatology. 2008;48:557–66.
Yamanaka-Okumura H, Nakamura T, Miyake H, Takeuchi H, Katayama T, Morine Y, et al. Effect of long-term late-evening snack on health-related quality of life in cirrhotic patients. Hepatol Res. 2010;40:470–6.
Hiraoka A, Michitaka K, Kiguchi D, Izumoto H, Ueki H, Kaneto M, et al. Efficacy of branched-chain amino acid supplementation and walking exercise for preventing sarcopenia in patients with liver cirrhosis. Eur J Gastroenterol Hepatol. 2017;29:1416–23.
Riordan SM, Williams R. Treatment of hepatic encephalopathy. N Engl J Med. 1997;337:473–9.
Córdoba J, López-Hellín J, Planas M, Sabín P, Sanpedro F, Castro F, et al. Normal protein diet for episodic hepatic encephalopathy: results of a randomized study. J Hepatol. 2004;41:38–43.
Gheorghe L, Iacob R, Vădan R, Iacob S, Gheorghe C. Improvement of hepatic encephalopathy using a modified high-calorie high-protein diet. Rom J Gastroenterol. 2005;14:231–8.
Swart GR, van den Berg JW, van Vuure JK, Rietveld T, Wattimena DL, Frenkel M. Minimum protein requirements in liver cirrhosis determined by nitrogen balance measurements at three levels of protein intake. Clin Nutr. 1989;8:329–36.
Weber FL, Minco D, Fresard KM, Banwell JG. Effects of vegetable diets on nitrogen metabolism in cirrhotic subjects. Gastroenterology. 1985;89:538–44.
Yoon M-S. mTOR as a key regulator in maintaining skeletal muscle mass. Front Physiol. 2017;8:788.
Qiu J, Tsien C, Thapalaya S, Narayanan A, Weihl CC, Ching JK, et al. Hyperammonemia-mediated autophagy in skeletal muscle contributes to sarcopenia of cirrhosis. Am J Physiol Endocrinol Metab. 2012;303:E983–93.
Chen H-W, Dunn MA. Muscle at risk: the multiple impacts of ammonia on sarcopenia and frailty in cirrhosis. Clin Transl Gastroenterol. 2016;7:e170.
Tsien C, Davuluri G, Singh D, Allawy A, Ten Have GAM, Thapaliya S, et al. Metabolic and molecular responses to leucine-enriched branched chain amino acid supplementation in the skeletal muscle of alcoholic cirrhosis. Hepatology. 2015;61:2018–29.
Leenders M, van Loon LJC. Leucine as a pharmaconutrient to prevent and treat sarcopenia and type 2 diabetes. Nutr Rev. 2011;69:675–89.
Holecek M. Three targets of branched-chain amino acid supplementation in the treatment of liver disease. Nutrition. 2010;26:482–90.
Román E, Torrades MT, Nadal MJ, Cárdenas G, Nieto JC, Vidal S, et al. Randomized pilot study: effects of an exercise programme and leucine supplementation in patients with cirrhosis. Dig Dis Sci. 2014;59:1966–75.
Les I, Doval E, García-Martínez R, Planas M, Cárdenas G, Gómez P, et al. Effects of branched-chain amino acids supplementation in patients with cirrhosis and a previous episode of hepatic encephalopathy: a randomized study. Am J Gastroenterol. 2011;106:1081–8.
Als-Nielsen B, Koretz RL, Kjaergard LL, Gluud C. Branched-chain amino acids for hepatic encephalopathy. Cochrane Database Syst Rev. 2003;2003:CD001939.
Gluud LL, Dam G, Les I, Marchesini G, Borre M, Aagaard NK, et al. Branched-chain amino acids for people with hepatic encephalopathy. Cochrane Database Syst Rev. 2017;5:CD001939.
Holeček M. Branched-chain amino acid supplementation in treatment of liver cirrhosis: updated views on how to attenuate their harmful effects on cataplerosis and ammonia formation. Nutrition. 2017;41:80–5.
Martin P, DiMartini A, Feng S, Brown R, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59:1144–65.
Buonomo AR, Zappulo E, Scotto R, Pinchera B, Perruolo G, Formisano P, et al. Vitamin D deficiency is a risk factor for infections in patients affected by HCV-related liver cirrhosis. Int J Infect Dis. 2017;63:23–9.
Konstantakis C, Tselekouni P, Kalafateli M, Triantos C. Vitamin D deficiency in patients with liver cirrhosis. Ann Gastroenterol. 2016;29:297–306.
Kubesch A, Quenstedt L, Saleh M, Rüschenbaum S, Schwarzkopf K, Martinez Y, et al. Vitamin D deficiency is associated with hepatic decompensation and inflammation in patients with liver cirrhosis: a prospective cohort study. PLoS One. 2018;13:e0207162.
Yang F, Ren H, Gao Y, Zhu Y, Huang W. The value of severe vitamin D deficiency in predicting the mortality risk of patients with liver cirrhosis: a meta-analysis. Clin Res Hepatol Gastroenterol. 2019;43(6):722–9.
Kotlarczyk MP, Perera S, Ferchak MA, Nace DA, Resnick NM, Greenspan SL. Vitamin D deficiency is associated with functional decline and falls in frail elderly women despite supplementation. Osteoporos Int. 2017;28:1347–53.
Bruyère O, Cavalier E, Reginster J-Y. Vitamin D and osteosarcopenia: an update from epidemiological studies. Curr Opin Clin Nutr Metab Care. 2017;20:498–503.
Hirschfeld HP, Kinsella R, Duque G. Osteosarcopenia: where bone, muscle, and fat collide. Osteoporos Int. 2017;28:2781–90.
Phu S, Bani Hassan E, Vogrin S, Kirk B, Duque G. Effect of denosumab on falls, muscle strength, and function in community-dwelling older adults. J Am Geriatr Soc. 2019;67(12):2660–1.
Remelli F, Vitali A, Zurlo A, Volpato S. Vitamin D deficiency and sarcopenia in older persons. Nutrients. 2019;11:E2861.
Rudman D, Sewell CW, Ansley JD. Deficiency of carnitine in cachectic cirrhotic patients. J Clin Invest. 1977;60:716–23.
Shiraki M, Shimizu M, Moriwaki H, Okita K, Koike K. Carnitine dynamics and their effects on hyperammonemia in cirrhotic Japanese patients. Hepatol Res. 2017;47(4):321–327.
de Sousa C, Leung NW, Chalmers RA, Peters TJ. Free and total carnitine and acylcarnitine content of plasma, urine, liver and muscle of alcoholics. Clin Sci. 1988;75:437–40.
Ohara M, Ogawa K, Suda G, Kimura M, Maehara O, Shimazaki T, et al. L-Carnitine suppresses loss of skeletal muscle mass in patients with liver cirrhosis. Hepatol Commun. 2018;2:906–18.
Hiramatsu A, Aikata H, Uchikawa S, Ohya K, Kodama K, Nishida Y, et al. Levocarnitine use is associated with improvement in sarcopenia in patients with liver cirrhosis. Hepatol Commun. 2019;3:348–55.
Nakanishi H, Kurosaki M, Tsuchiya K, Nakakuki N, Takada H, Matsuda S, et al. L-carnitine reduces muscle cramps in patients with cirrhosis. Clin Gastroenterol Hepatol. 2015;13:1540–3.
Malaguarnera M. Acetyl-L-carnitine in hepatic encephalopathy. Metab Brain Dis. 2013;28:193–9.
Bode JC, Hanisch P, Henning H, Koenig W, Richter FW, Bode C. Hepatic zinc content in patients with various stages of alcoholic liver disease and in patients with chronic active and chronic persistent hepatitis. Hepatology. 1988;8:1605–9.
Chavez-Tapia NC, Cesar-Arce A, Barrientos-Gutiérrez T, Villegas-López FA, Méndez-Sanchez N, Uribe M. A systematic review and meta-analysis of the use of oral zinc in the treatment of hepatic encephalopathy. Nutr J. 2013;12:74.
Shen Y-C, Chang Y-H, Fang C-J, Lin Y-S. Zinc supplementation in patients with cirrhosis and hepatic encephalopathy: a systematic review and meta-analysis. Nutr J. 2019;18:34.
Takuma Y, Nouso K, Makino Y, Hayashi M, Takahashi H. Clinical trial: oral zinc in hepatic encephalopathy. Aliment Pharmacol Ther. 2010;32:1080–90.
Sengupta S, Wroblewski K, Aronsohn A, Reau N, Reddy KG, Jensen D, et al. Screening for zinc deficiency in patients with cirrhosis: when should we start? Dig Dis Sci. 2015;60:3130–5.
Bajaj JS, Salzman NH, Acharya C, Sterling RK, White MB, Gavis EA, et al. Fecal microbial transplant capsules are safe in hepatic encephalopathy: a phase 1, randomized, placebo-controlled trial. Hepatology. 2019;70:1690–703.
Ticinesi A, Lauretani F, Milani C, Nouvenne A, Tana C, Del Rio D, et al. Aging gut microbiota at the cross-road between nutrition, physical frailty, and sarcopenia: is there a gut-muscle axis? Nutrients. 2017;9:E1303.
Casula EP, Bisiacchi PS, Corrias M, Schiff S, Merkel C, Amodio P, et al. Acute hyperammonaemia induces a sustained decrease in vigilance, which is modulated by caffeine. Metab Brain Dis. 2015;30:143–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Duarte-Rojo reports non-financial support from Echosens, other from Mallinckrodt, other from Axcella, outside the submitted work. The other authors declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Nutrition in Patients with Chronic Liver Disease
Electronic Supplementary Material
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Salim, T., Stark, S.A. & Duarte-Rojo, A. Food as Therapy for Frailty. Curr Hepatology Rep 19, 23–29 (2020). https://doi.org/10.1007/s11901-020-00509-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11901-020-00509-x