Abstract
Purpose of Review
The study aims to evaluate the impact of COVID-19 on the delivery of health care and services to patients with chronic myeloid leukemia in low- and middle-income countries (LMICs) accessing treatment through The Max Foundation.
Recent Findings
An online survey was developed and sent via email to 527 partner physicians who had active patients under their care in July 2020, asking about the disruption of health services with multiple-choice answers or a five-point ordinal scale. Data from The Max Foundation’s Patient Access Tracking System (PATS®) was analyzed to evaluate program performance in 2020 compared with 2019. PATS® is used to track key patient information and supply chain data to ensure robust reporting, quality assurance, and safety. Among the 111 physicians who responded (20% response rate), 48% reported that someone on their team had contracted COVID-19. A total of 95 (85%) physicians reported at least some disruption of services to patients due to COVID-19, with 29 (26%) reporting frequent or complete disruption. Almost all physicians in the South Asia and Asia Pacific regions reported disruption (96% and 95%, respectively), compared with three quarters of physicians in Latin America. Institutions overcame challenges using a variety of solutions including telemedicine (60%), electronic prescriptions (45%), home delivery via courier services (31%), government workers (9%), and dispensation coordination with regional hospitals (14%).
Summary
The COVID-19 pandemic has disrupted services for CML physicians and patients worldwide. Overall, these disruptions did not appear to significantly affect The Max Foundation’s ability to provide patients with access to treatment, as novel approaches in telemedicine, supply chain, and dispensing, as well as provision of guidance and support for physicians were utilized to overcame disruption of services.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic myeloid leukemia (CML) is the model for modern “precision” medicine, where treatment is targeted based on a patient’s genetic makeup. All CML patients have a rearrangement of the BCR gene from chromosome 22 with the kinase domain of ABL from chromosome 9. This chimeric gene can be used for diagnosis (either by cytogenetics or RT-PCR) and monitoring to follow disease response. Tyrosine kinase inhibitor (TKI) therapy, aimed at the BCR-ABL protein, blocks the ABL ATP kinase function and inhibits disease proliferation. TKIs are remarkably effective and have changed the natural history from approximately 7 years to a near-normal lifespan [1•].
However, none of this remarkable progress matters if you are a CML patient and cannot get TKI therapy. This is sadly a common problem for CML patients in low- and middle-income countries (LMICs), who encounter myriad obstacles to accessing health care in general, let alone cancer care and access to medicines [2••].
Since 2001, The Max Foundation has partnered with Novartis, first through The Glivec International Patient Assistance Program (GIPAP; 2001–2017) and subsequently through the Max Access Solutions (MAS) program (2017–present), to provide imatinib (Glivec®) at no cost to eligible CML patients from LMICs until the drug is available through local health authorities [3•]. Other manufacturers of TKIs joined The Max Foundation’s efforts since 2017 and as a result through Max Access Solutions treating physicians in the MAS countries have access to multiple TKIs to treat their patients. These collaborations, while centered on the delivery of TKI to CML patients in LMICs, offer a unique model for care delivery in other diseases as well. This simplicity of the objective belies the complexity of the task, including making the diagnosis of CML, identifying potential patients and physician partners, working with the local bureaucracy of the individual LMIC, and developing the logistics of obtaining and distributing drugs. Nonetheless, the Max Foundation has supported more than 90,000 CML patients in over 75 countries, and has facilitated the delivery of over 100 million doses of TKIs [4]. And the results are spectacular: the patients served by The Max Foundation enjoy a similar survival to CML patients treated in Western and European nations (Fig. 1) [2••].
Challenge: the Impact of COVID-19 on CML Patient Care
The COVID-19 pandemic has had a major impact on the delivery of health services worldwide. At the beginning of the pandemic in March 2020, The Max Foundation was actively supporting over 32,000 patients under the care of 527 physicians in 72 LMICs. COVID-19 substantially impacted the lives of people in LMICs [5, 6••, 7]. The Max Foundation’s MAS programs providing access to cancer medicines were severely impacted by the pandemic. Dynamic solutions were developed at every level of the system, from the patients to local staff, institutions, and physicians to supply chain partners to staff at the headquarter. Global supply chain was disrupted due to airport closures and aircraft cancellations, refusal to accept imported shipments, and severe delay in the import permit approval process. This disruption put the CML patient community at high risk of experiencing in-country stock shortages, expiration of the medicines, and ultimately premature deaths of patients.
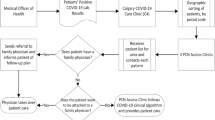
To determine how COVID-19 affected the care of CML patients, an online survey was developed and sent via email to 527 partner physicians who had active patients under their care in July 2020. The survey asked questions about the disruption of health services with multiple-choice answers or a five-point ordinal scale. Survey responses were received from 111 physicians (21%) from 46 countries in Latin America (32%), South Asia (24%), Africa and the Middle East (19%), Asia Pacific (17%), and Eastern Europe and Central Asia (8%), between June and August 2020. These 46 countries had 27,678 patients (92% of our total patient population) as of June 1, 2020. Survey responses were highest from India (19%), Philippines (14%), and Argentina (7%). In addition to the physician survey, we analyzed data from The Max Foundation’s Patient Access Tracking System (PATS®) to evaluate program performance in 2020 compared with 2019.
Out of the 111 respondents (527 invited), 48% of the participating physicians responded that someone on their team had contracted COVID-19. A total of 95 (85%) physicians reported at least some disruption of services to patients due to COVID-19, with 29 (26%) reporting frequent or complete disruption. Almost all physicians in the South Asia and Asia Pacific regions reported disruption (96% and 95%, respectively), compared with three quarters of physicians in Latin America.
Nearly two thirds of the participating physicians reported that governmental and public transportation lockdowns hindered access to health facilities and led to occasional to complete disruptions. Other commonly reported causes of disruption included closure of health care facilities, in-patient services, and diagnostic facilities for non-COVID-19 cases that led to occasional to complete disruption of the services. Figure 2 shows the (number or percentage) extent of disruptions across five different geographic regions. The causes of treatment disruptions are shown in Table 1. The most common causes of disruption of services reported were government or public transport lockdowns hindering access to health facilities (85%) and decrease in patient volume due to cancellation of appointments (82%).
Some adverse impact was observed in 2020 compared with 2019 including decreased number of patient cases approved in all regions (2902 patient cases in 2019 vs. 2604 patient cases in 2020); increased average time between drug order placement and delivery in two regions, Latin America (41 days in 2019 vs. 64 days in 2020) and South Asia (27 days in 2019 vs. 31 days in 2020); and increased average time between drug order placement and delivery in two regions (Fig. 3), Latin America (41 days in 2019 vs. 64 days in 2020) and South Asia (27 days in 2019 vs. 31 days in 2020). Two thirds of physicians expect that service levels would return to normal within 1–3 months post-pandemic.
The global supply chain of the CML medicines was substantially affected by the pandemic. Among the physicians who are routinely involved in the importation process of the medications, airport closure was reported commonly (45.0%) to have led to occasional to complete disruptions during the pandemic. Delays in securing import permits (40%) and custom clearance (41.3%) were also common challenges reported.
Surprisingly, “stockout” of the medications was reported infrequently as the cause of disrupted services. This generally occurred because of country-specific lockdowns of air and ground shipping. In other countries, administrative offices charged with controlling importation were closed. In Africa, there appeared to be a reluctance from patients to come to centers to pick up medicines in fear of contracting COVID-19. At the ground level, the communities of patients and local staff in the countries participating in our program adopted adaptive and effective local solutions during this pandemic. A survey with physicians showed that their institutions tried to overcome challenges using a variety of solutions including telemedicine (60%), electronic prescriptions (45%), home delivery via courier services (31%), government workers (9.0%), and dispensation coordination with regional hospitals (14%).
Examples of General and Local Solutions to the COVID-19 Challenge
Many institutions utilized novel approaches (Fig. 3) to overcome service disruptions to (Fig. 4) including telemedicine (60%), electronic prescriptions (50%), and home delivery via courier services (34%). COVID-19 educational materials (67%) were frequently selected as support needed to overcome disruption of services due to COVID-19. At the local level, many countries and communities implemented strict lockdowns in which people were ordered to stay home or limit travel frequencies and distance. Some hospitals could not receive any patients other than those with COVID-19. Some health care professionals, including our local partners, passed away due to COVID-19, which was devastating given the extremely low numbers of health care professionals even under normal circumstances in these countries. Those barriers and restrictions threatened the lifeline for our patients.
Peer Support Systems
The COVID-19 pandemic demonstrated the importance of the existing peer support systems that The Max Foundation has supported over the past two decades in responding to unforeseen events to mitigate disruptions in treatment and care. In the Philippines, strict community lockdown started in March 2020 with only the police and selective official authorities allowed to travel. This meant that there were (1) no local couriers who could deliver medicine to patients, (2) no public/private transport available, and (3) no “border” crossing across neighborhoods allowed. Thus, peer support from the patient community was essential for the distribution of medicines. Patients worked together to pick up and deliver medicines — from Manila to Pampanga, Batangas, or Laguna — which required finding someone with an authorized vehicle and driving directly to the CML patient (~ 200 km in some cases). The local Max staff connected these patients with each other by phone and coordinating with drug dispensers. Other countries developed other creative solutions. In India, patients were wary of traveling and courier services were not available. Therefore, support from essential units like the Police and Firemen were pressed into service to deliver medicine to patients. In Kerala, family, friends, patient leaders, and other community members volunteered to do TKI deliveries. Commercial outlets in the marketplace, banks, and stationery shops offered to help print documents Max would send to the patients’ smart phones.
Use of Technologies
Max offices in Africa and South Asia offices favorably reported technological solutions. Rwanda implemented strict lockdown as of March 22, and even after the regulation was relaxed on May 4, between-province travels were not permitted. As Rwanda is a geographically small country, patients benefited from the new implementation of medication delivery by drone. Telemedicine was also utilized, though not between patients and physicians as most patients lack the technology to use telemedicine. Instead, telemedicine was used among remote physicians (e.g., rural general practitioners to specialists). Physician from rural clinics consulted with specialists in specialized centers, and if necessary, doctors in rural clinics ordered labs and communicated results via WhatsApp or email to patients. Doctors in rural clinic made necessary orders through the on-demand Zipline delivery system, and within 40 min, the medications were dispensed to the clinics.
There were many benefits of these use of technologies in care. Patients did not need to travel outside of their regions and the burden on the specialized centers were reduced. Similar use of technologies was seen in some format in other African countries like Ethiopia, Malawi, and Tanzania during the pandemic, and their continued implementation potentially may significantly advance health care infrastructure in these countries. Indeed, uses of these technologies were essential for Max to reach each other, partners, and patients. In places like India where there was a strict lockdown, the team were able to stay in touch with over 14,500 patients via their phones, sending text messages that enumerated necessary precautions and hygiene tips to stay safe and making sure they could reach out to them any time of the day.
Another technological challenge revolved around diagnostic testing and monitoring. The diagnosis of CML requires technical and expensive tools (cytogenetics, FISH, and RT-PCR of the BCR-ABL fusion). This means bone marrow aspirate/biopsy needles, microscopes, culture equipment, and thermocyclers, and highly trained personnel. This is obviously challenging in LMICs, even prior to the pandemic. Over the years, solutions for testing has greatly increased access, including the invention and wide distribution of automated, cartridge-based systems developed by Cepheid [8]. The widespread availability of the Cepheid BCR-ABL1 test was primed by WHO support of Cepheid’s infectious disease assays (e.g., TB, HIV) in LMICs, placing machines in many centers across the globe (there are currently over 25,000 machines in use). Since multiple cartridges can be run simultaneously, assays for BCR-ABL1, TB, and HIV can be performed simultaneously. Another option for CML diagnosis is shipping samples to specialized centers with laboratory capacity for testing. Shipping fresh blood is inefficient and expensive, so a technique was recently developed to perform BCR-ABL1 testing using dried blood spots [9•], which are stable at room temperature for weeks, and thus can be batched and shipped by slower, cheaper methods.
Testing during the pandemic obviously suffered, simply because access to centers, and thus, access to venipuncture, was so compromised. Efforts are underway to develop point-of-care methods to collect blood in a minimally invasive fashion, using collection devices that can draw blood through muscle and can be self-applied by the patient. In addition, non-electrical methods to perform testing are being developed, which use isothermal amplification methods, and read out via lateral flow devices [10]. Think of a “pregnancy test” for CML. These advances could be utilized to perform home testing, even perhaps delivered to the patients dwelling via drones.
Outcome Measurements
Despite widely reported disruption of health services due to COVID-19, The Max Foundation reported overall growth in delivery and support programs, including an increase in the total number of patients supported from 2019 to 2020 and an expansion of treatments into new countries. However, some impact was observed in 2020 compared with 2019 including decreased number of patient cases approved in all regions (2902 patient cases in 2019 vs. 2604 patient cases in 2020) and increased average time between drug order placement and delivery in two regions, Latin America (41 days in 2019 vs. 64 days in 2020) and South Asia (27 days in 2019 vs. 31 days in 2020). During the pandemic, The Max Foundation supported physicians during health service disruptions through increased patient contact (a 50% increase in patient calls and messages), and boosted advocacy on behalf of patients (e.g., electronic prescriptions, permission to visit hospital, pick up drug supply, or have home delivery of medicines).
Conclusion
The local CML communities’ response to the challenges imposed by the COVID-19 pandemic was phenomenal. Numerous diverse, unique, and successful solutions were developed and implemented to mitigate the disruption of services. Problems faced by these global communities could not have been solved by a single solution. Alas, this is not the last of pandemics, either from a resurgence of COVID-19 or the emergence of a new actor. There are some clear lessons that bring a call to action. First, even after the current pandemic recedes, governments, businesses, and global health communities need to build much more resilient global supply chain networks for essential goods like medicines during pandemics. Secondly, we should seize this opportunity to further advance telemedicine and use of other technologies in LMIC health care systems. The implementation of technological solutions during this pandemic will likely have lasting effects in these resource-limited settings. Governments and donors need to take this opportunity to consider expanding the use of these technologies and strengthen their health care systems. The successful cases of our global communities’ response demonstrate the importance of collaborative preparation for and response to disruptive events in the future.
Data availability
The data that support the findings of this study are available from the corresponding author or info@themaxfoundation.org upon reasonable request.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bower H, Björkholm M, Dickman PW, Höglund M, Lambert PC, Andersson TM-L. Life expectancy of patients with chronic myeloid leukemia approaches the life expectancy of the general population. J Clin Oncol. 2016;34:2851–7. https://doi.org/10.1200/JCO.2015.66.2866. Analysis of Swedish Cancer Registry in 1973–2013 demonstrating advancement in treatment options for CML has improved the life expectancy of patients with CML to a similar level in the general population.
Malhotra H, Radich J, Garcia-Gonzalez P. Meeting the needs of CML patients in resource-poor countries. Hematology 2014, the American Society of Hematology Education Program Book. 2019;2019(1):433–42. https://doi.org/10.1182/hematology.2019000050. A great overview of the myriad challenges and solutions of diagnosing and treating CML in low- and-middle income coutries.
Garcia-Gonzalez P, Boultbee P, Epstein D. Novel humanitarian aid program: the glivec international patient assistance program-lessons learned from providing access to breakthrough targeted oncology treatment in low- and middle-income countries. J Glob Oncol. 2015;1(1):37–45. https://doi.org/10.1200/JGO.2015.000570. The article describes the structure of the GIPAP program and lessons that have contributed to the success of the program.
The Max Foundation. Patient Access Tracking System. [cited 6 Jun 2022]. Available: https://www.maxaid.org/
Bottan N, Hoffmann B, Vera-Cossio D. The unequal impact of the coronavirus pandemic: evidence from seventeen developing countries. PLoS ONE. 2020;15:e0239797. https://doi.org/10.1371/journal.pone.0239797.
Levin AT, Owusu-Boaitey N, Pugh S, Fosdick BK, Zwi AB, Malani A, et al. Assessing the burden of COVID-19 in developing countries: systematic review, meta-analysis and public policy implications. BMJ Glob Health. 2022;7:e008477. https://doi.org/10.1136/bmjgh-2022-008477. Systematic review of serology studies showing higher burden of COVID-19 in LMICs towards the beginning of the pandemic due to challenges such as lack of access to health care.
Kumar D, Dey T. Treatment delays in oncology patients during COVID-19 pandemic: a perspective. J Glob Health. 2020;10:010367. https://doi.org/10.7189/jogh.10.010367.
Winn-Deen ES, Helton B, Van Atta R, Wong W, Peralta J, Wang J, et al. Development of an integrated assay for detection of BCR-ABL RNA. Clin Chem. 2007;53:1593–600. https://doi.org/10.1373/clinchem.2007.085472.
Sala Torra O, Beppu L, Smith JL, Welden L, Georgievski J, Gupta K, et al. Paper or plastic? BCR-ABL1 quantitation and mutation detection from dried blood spots. Blood. 2016;127:2773–4. https://doi.org/10.1182/blood-2015-12-689059. First example of using dried blood spots for BCR-ABL1 mRNA testing.
Sooknanan R, Malek L, Wang XH, Siebert T, Keating A. Detection and direct sequence identification of BCR-ABL mRNA in Ph+ chronic myeloid leukemia. Exp Hematol. 1993;21:1719–24.
Acknowledgements
We would like to thank the global CML patient communities, local physician partners, and the Max Foundation staff whose talent and commitment helped us tremendously as we navigated through the uncertainty the pandemic brought. We would also like to acknowledge the following individuals contributed stories of successful response during the pandemic: Inés García González, Mei Ching Ong, Viji Venkatesh, Catherina Scheepers, and Jean Paul Mukundiyukuri.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Annamalay reports grants from Novartis,grants from Bristol Myers Squibb, grants from Pfizer, grants from Takeda, and grants from Incyte, during the conduct of the study, and grants from Novartis, grants from Bristol Myers Squibb, grants from Pfizer, grants from Takeda, and grants from Incyte, outside the submitted work.
Dr. Radich reports other from Cepheid, outside the submitted work.
Dr. Matsuzaki’s contribution to this publication was as a member of the Board of Directors of The Max Foundation. This arrangement has been reviewed and approved by the Johns Hopkins University in accordance with its conflict of interest policies.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Chronic Myeloid Leukemias
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Matsuzaki, M., Annamalay, A., Garcia-Gonzalez, P. et al. CML Outcomes and Care Delivery During the COVID-19 Pandemic in Low- and Middle-Income Countries. Curr Hematol Malig Rep 18, 1–7 (2023). https://doi.org/10.1007/s11899-022-00686-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11899-022-00686-0