Abstract
Childhood chronic myelogenous leukemia (CML) is a rare malignancy, and experience with optimal treatment is very limited. Traditionally, allogeneic hematopoietic stem cell transplantation was considered the only curative treatment. Imatinib, a small-molecule inhibitor of the BCR-ABL tyrosine kinase (TKI), has been proven highly successful in adults with CML, resulting in prolonged molecular response with limited drug toxicity. This drug is now included as front-line therapy for CML in pediatrics as well, though valid concerns about serious late sequelae remain unresolved. Specific pediatric treatment guidelines have not yet been formulated, and most algorithms are derived from experience in adult CML. This overview attempts to summarize pediatric studies on issues such as dose, duration, adverse effects, and steering criteria for TKI treatment, adapting guidelines developed in adult medicine to pediatrics. Most importantly, pediatric patients with CML receiving TKI treatment should be enrolled into formal trials.
Similar content being viewed by others
References
Recently particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ries LAG, Smith MA, Gurney JG, et al. Cancer incidence and survival among children and adolescents: United States SEER Program 1975–1995. SEER Pediatr Monogr. 1999;99:46–9.
Gratwohl A, Heim D. Current role of stem cell transplantation in chronic myeloid leukaemia. Review. Best Pract Res Clin Haematol. 2009;22:431–43.
Cwynarski K, Roberts IA, Iacobelli S, et al. Stem cell transplantation for chronic myeloid leukemia in children. Blood. 2003;102:1224–31.
• Suttorp M, Claviez A, Bader P, et al. Allogeneic stem cell transplantation for pediatric and adolescent patients with CML: results from the prospective trial CML-paed I. Klin Padiatr. 2009;221:351–7. This paper reports data compiled during the “pre-imatinib era” on the outcome of related and unrelated allogeneic stem cell transplantation in 174 German pediatric patients with CML enrolled into the prospectively conducted controlled trial CML-paed I.
Druker BJ, Guilhot F, O’Brien SG, et al. IRIS Investigators. Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med. 2006;355:2408–17.
Goldman JM, How I. treat chronic myeloid leukemia in the imatinib era. Review. Blood. 2007;110:2828–37.
Millot F, Traore P, Guilhot J, et al. Clinical and biological features at diagnosis in 40 children with chronic myeloid leukemia. Pediatrics. 2005;116:140–3.
•• Suttorp M, Millot F. Treatment of pediatric chronic myeloid leukemia in the year, use of tyrosine kinase inhibitors and stem cell transplantation. Review. Hematology Am Soc Hematol Educ Program. 2010;2010:368–76. This review of available data describes the role of imatinib in children with CML, addressing (1) the starting dose; (2) pharmacokinetics in childhood; (3) possible adverse effects, with a focus on the still-growing skeleton; (4) early monitoring of treatment efficacy in an attempt to avoid failure; (5) the timing of allogeneic HSCT in children; and (6) treatment of CML relapse after HSCT.
Cortes J, Kantarjian HM, Giralt S, Talpaz M. Natural history and staging of chronic myelogenous leukaemia. Baillieres Clin Haematol. 1997;10:277–90.
Hughes T, Deininger M, Hochhaus A, et al. Monitoring CML patients responding to treatment with tyrosine kinase inhibitors: review and recommendations for harmonizing current methodology for detecting BCR-ABL transcripts and kinase domain mutations and for expressing results. Blood. 2006;108:28–37.
Fabarius A, Leitner A, Hochhaus A, et al. Impact of ACA at diagnosis on prognosis of CML: long-term observation from 1151 patients of the randomized CML Study IV. Blood 2011, Oct 28 (Epub ahead of print).
Weisdorf DJ, Anasetti C, Antin JH, et al. Allogeneic bone marrow transplantation for chronic myelogenous leukemia: comparative analysis of unrelated versus matched sibling donor transplantation. Blood. 2002;99:1971–7.
•• Pavlu J, Szydlo RM, Goldman JM, Apperley JF. Three decades of transplantation for chronic myeloid leukemia: What have we learned? Blood. 2011;117:755–63. This is an in-depth review of the knowledge gained from transplantation in CML that furthered the understanding of this leukemia, improved awareness of stem cell biology and immunotherapeutics, and initiated the concept of molecular monitoring and management of minimal residual disease.
Kebriaei P, Detry MA, Giralt S, et al. Long-term follow-up of allogeneic hematopoietic stem-cell transplantation with reduced-intensity conditioning for patients with chronic myeloid leukemia. Blood. 2007;110:3456–62.
Simula MP, Marktel S, Fozza C, et al. Response to donor lymphocyte infusions for chronic myeloid leukemia is dose-dependent: the importance of escalating the cell dose to maximize therapeutic efficacy. Leukemia. 2007;21:943–8.
Klyuchnikov E, Kröger N, Brummendorf TH, et al. Current status and perspectives of tyrosine kinase inhibitor treatment in the posttransplant period in patients with chronic myelogenous leukemia (CML). Review. Biol Blood Marrow Transplant. 2010;16:301–10.
Passweg JR, Walker I, Sobocinski KA, et al. Validation and extension of the EBMT Risk Score for patients with chronic myeloid leukaemia (CML) receiving allogeneic haematopoietic stem cell transplants. Br J Haematol. 2004;125:613–20.
• Muramatsu H, Kojima S, Yoshimi A, et al. Outcome of 125 children with chronic myelogenous leukemia who received transplants from unrelated donors: the Japan Marrow Donor Program. Biol Blood Marrow Transplant. 2010;16:231–8. The outcomes of hematopoietic stem cell transplantation from unrelated donors in 125 Japanese children with Ph + CML are retrospectively analyzed, providing important information about assessing the indications for unrelated BMT for the treatment of pediatric CML and improving its outcome.
Muramatsu H, Takahashi Y, Sakaguchi H, et al. Excellent outcomes of children with CML treated with imatinib mesylate compared to that in pre-imatinib era. Int J Hematol. 2011;93:186–91.
Goldman JM, Majhail NS, Klein JP, et al. Relapse and late mortality in 5-year survivors of myeloablative allogeneic hematopoietic cell transplantation for chronic myeloid leukemia in first chronic phase. J Clin Oncol. 2010;28:1888–95.
Marin D, Milojkovic D, Olavarria E, et al. European LeukemiaNet criteria for failure or suboptimal response reliably identify patients with CML in early chronic phase treated with imatinib whose eventual outcome is poor. Blood. 2008;112:4437–44.
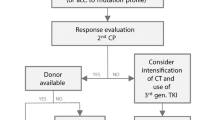
• Baccarani M, Cortes J, Pane F, et al. Chronic myeloid leukemia: an update of concepts and management recommendations of European LeukemiaNet. J Clin Oncol. 2009;27:6041–51. Aiming for 100% survival and a normal quality of life in adult patients with CML, the European LeukemiaNet has reviewed recent results of therapy, standard monitoring procedures, and definitions of responses. This publication presents the updated recommendations with the aim of contributing to optimization and standardization in the management of CML.
Suttorp M. Innovative approaches of targeted therapy for CML of childhood in combination with paediatric haematopoietic SCT. Review. Bone Marrow Transplant. 2008;42 Suppl 2:S40–46.
•• Millot F, Baruchel A, Guilhot J, et al. Imatinib is effective in children with previously untreated chronic myelogenous leukemia in early chronic phase: results of the French national phase IV trial. J Clin Oncol. 2011;29:2827–32. This paper reports the results of a prospective trial conducted in 44 French patients from 10 months to 17 years of age with newly diagnosed CML in CP, receiving imatinib 260 mg/m 2 daily. With a median follow-up time of 31 months (range, 11–64 months), the estimated progression-free survival rate at 36 months was 98%; at 12 months, the rate of complete cytogenetic response (CCyR) was 61%, and the rate of major molecular response (MMolR) was 31%. The most common adverse events were neutropenia and musculoskeletal events.
Hasford J, Baccarani M, Hoffmann V, et al. Predicting complete cytogenetic response and subsequent progression-free survival in 2060 patients with CML on imatinib treatment: the EUTOS score. Blood. 2011;118:686–92.
• Smith CC, Shah NP. Tyrosine kinase inhibitor therapy for chronic myeloid leukemia: approach to patients with treatment naïve or refractory chronic-phase disease. (Review). Hematology Am Soc Hematol Educ Program, 2011:121–127. This review lists the most recent clinical trial results for approved and investigational tyrosine kinase inhibitors and provides recommendations on how to treat imatinib resistance and how to choose second-line treatment.
Suttorp M, Thiede C, Tauer JT, et al. Impact of the type of the BCR-ABL fusion transcript on the molecular response in pediatric patients with chronic myeloid leukemia. Haematologica. 2010;95:852–3.
Lucas CM, Harris RJ, Giannoudis A, et al. Chronic myeloid leukemia patients with the e13a2 BCR-ABL fusion transcript have inferior responses to imatinib compared to patients with the e14a2 transcript. Haematologica. 2009;94:1362–7.
Müller MC, Cross NC, Erben P, et al. Harmonization of molecular monitoring of CML therapy in Europe. Leukemia. 2009;23:1957–63.
Suttorp M, Thiede C, Tauer JT, et al. Chronic Myeloid Leukemia in Pediatrics—First Results from Study CML-PAED II. (ASH Abstract 342). Blood. 2009;114:145.
• Champagne MA, Fu CH, Chang M, et al. Higher dose imatinib for children with de novo chronic phase chronic myelogenous leukemia: a report from the Children’s Oncology Group. Pediatr Blood Cancer. 2011;57:56–62. This multicenter, phase II clinical trial explored the efficacy of higher-dose imatinib (340 mg/m 2 ) in 51 North American children with newly diagnosed CML-CP. The most common toxicities encountered were hematologic. Overall, 72% achieved CCyR at a median time of 5.6 months and a 27% rate of complete molecular response (>3 log reduction) was observed. At 3 years, progression-free survival was 72%, and overall survival was 92%.
Aplenc R, Blaney SM, Strauss LC, et al. Pediatric Phase I Trial and Pharmacokinetic Study of Dasatinib: A Report From the Children’s Oncology Group Phase I Consortium. J Clin Oncol. 2011;29:839–44.
Champagne MA, Capdeville R, Krailo M, et al. Imatinib mesylate (STI571) for treatment of children with Philadelphia chromosome-positive leukemia: results from a Children’s Oncology Group phase 1 study. Blood. 2004;104:2655–60.
Millot F, Guilhot J, Nelken B, et al. Imatinib mesylate is effective in children with chronic myelogenous leukemia in late chronic and advanced phase and in relapse after stem cell transplantation. Leukemia. 2006;20:187–92.
Belgaumi AF, Al-Shehri A, Ayas M, et al. Clinical characteristics and treatment outcome of pediatric patients with chronic myeloid leukemia. Haematologica. 2010;95:1211–5.
Geoerger B, Morland B, Ndiaye A, et al. Innovative Therapies for Children with Cancer European Consortium. Target-driven exploratory study of imatinib mesylate in children with solid malignancies by the Innovative Therapies for Children with Cancer (ITCC) European Consortium. Eur J Cancer. 2009;45:2342–51.
Hochhaus A. Educational session: managing chronic myeloid leukemia as a chronic disease. Review. Hematology Am Soc Hematol Educ Program, 2011:128–35.
•• Vandyke K, Fitter S, Dewar AL, et al. Dysregulation of bone remodelling by imatinib mesylate. Review Blood. 2010;115:766–74. This review highlights the current understanding of the mechanisms surrounding the effects of imatinib on the skeleton. In particular, it examines recent studies suggesting that imatinib has a direct effect on bone-resorbing osteoclasts and bone-forming osteoblasts through inhibition of c-fms, c-kit, carbonic anhydrase II, and the platelet-derived growth factor receptor, resulting in dysregulated bone remodelling as a possible side effect of imatinib treatment..
Mariani S, Giona F, Basciani S, et al. Low bone density and decreased inhibin-B/FSH ratio in a boy treated with imatinib during puberty. Lancet. 2008;372:111–2.
Kimoto T, Inoue M, Kawa K. Growth deceleration in a girl treated with imatinib. Int J Hematol. 2009;89:251–2.
Schmid H, Jaeger B, Lohse J, et al. Longitudinal growth retardation in a prepubertal girl with chronic myeloid leukemia on long-term treatment with imatinib. Haematologica. 2009;94:1177–9.
Hobernicht SL, Schweiger B, Zeitler P, et al. Acquired growth hormone deficiency in a girl with chronic myelogenous leukemia treated with tyrosine kinase inhibitor therapy. Pediatr Blood Cancer. 2011;56:671–3.
Millot F, Baruchel A, Guilhot J, et al. Imatinib is efficient but has a negative impact on growth in children with previously untreated chronic myelogenous leukemia (CML) in early chronic phase (CP): Results of the French National Phase IV trial. (ASH Abstract 863). Blood. 2009;114:863.
• Shima H, Tokuyama M, Tanizawa A, et al. Distinct impact of imatinib on growth at prepubertal and pubertal ages of children with chronic myeloid leukemia. J Pediatr. 2011;159:676–81. A decrease in longitudinal height Z-score was observed during imatinib treatment in 73% of 48 Japanese children (median age, 9 years; range, 2–15 years) with chronic-phase CML. During a median follow-up time of 34 months (range, 10–88 months), growth impairment was seen predominantly in children who started imatinib before puberty, compared with those who started at a pubertal age. As they reached pubertal age, growth velocity tended to recuperate in prepubertal children with growth impairment, suggesting that imatinib had little impact on growth during puberty..
• Bansal D, Shava U, Varma N, et al. Imatinib has adverse effect on growth in children with chronic myeloid leukemia. Pediatr Blood Cancer 2011 Nov 2. (Epub ahead of print). In India, 20 children (median age, 10 years, range, 2–13 years; 13 prepubertal) with a diagnosis of CML were treated with imatinib in a single center for 61 months (range, 31–83 months). Regular growth assessment exhibited a highly significant reduction in the longitudinal height Z-score. Children who started imatinib therapy after the onset of puberty (n = 7) were not affected by this adverse effect.
Sanders JE: Growth and development after hematopoietic cell transplantation. In Thomas’ Hematopoietic Cell Transplantation. Edited by Appelbaum FR, Forman SJ, Negrin RS, Blume KG. Chichester: Wiley-Blackwell; 2009:1608–1610.
Couto-Silva AC, Trivin C, Esperou H, et al. Final height and gonad function after total body irradiation during childhood. Bone Marrow Transplant. 2006;38:427–32.
Rohon P, Porkka K, Mustjoki S. Immunoprofiling of patients with chronic myeloid leukemia at diagnosis and during tyrosine kinase inhibitor therapy. Eur J Haematol. 2010;85:387–98.
Apperley J. CML in pregnancy and childhood. Best Pract Res Clin Haematol. 2009;22:455–74.
• Mahon FX, Réa D, Guilhot J, et al. Discontinuation of imatinib in patients with chronic myeloid leukaemia who have maintained complete molecular remission for at least 2 years: the prospective, multicentre Stop Imatinib (STIM) trial. Lancet Oncol. 2010;11:1029–35. Imatinib was discontinued in 100 adult patients with CML who showed undetectable transcripts on quantitative RT-PCR (>5-log reduction in BCR–ABL/ABL ratio levels). During a median follow-up interval of 17 months (range 1–30 months), 69 patients relapsed (40 before 6 months, one patient at month 7, and one at month 19), but all patients who relapsed responded to reintroduction of imatinib. At 12 months, the probability of persistent complete molecular remission (CMolR) was 41%; a low Sokal score, male sex, and longer imatinib treatment duration were identified as factors predictive of CMolR maintenance after imatinib withdrawal.
Disclosure
Conflicts of Interest: M. Suttorp: His institution has received grants from Bristol-Myers Squibb and Novartis, as well as travel expenses from Pfizer; L. Eckardt: none; J.T. Tauer: none; F. Millot: none.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suttorp, M., Eckardt, L., Tauer, J.T. et al. Management of Chronic Myeloid Leukemia in Childhood. Curr Hematol Malig Rep 7, 116–124 (2012). https://doi.org/10.1007/s11899-012-0113-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11899-012-0113-6