Abstract
Purpose of the Review
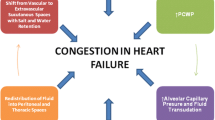
Progressive intravascular, interstitial, and alveolar fluid overload underlies the transition from compensated to acutely decompensated heart failure and loop diuretics are the mainstay of treatment. Adverse effects and resistance to loop diuretics received much attention while the contribution of a depressed cardiac output to diuretic resistance was downplayed.
Recent Findings
Analysis of experience with positive inotropic agents, especially dobutamine, indicates that enhancement of cardiac output is not consistently associated with increased renal blood flow. However, urinary output and renal sodium excretion increase likely due to dobutamine-mediated decrease in renal and systemic reduced activation of sympathetic nervous- and renin–angiotensin–aldosterone system. Mechanical circulatory support with left ventricular assist devices ascertained the contribution of low cardiac output to diuretic resistance and the pathogenesis and progression of kidney disease in acutely decompensated heart failure.
Summary
Diuretic resistance commonly occurs in acutely decompensated heart failure. However, failure to resolve fluid overload despite high doses of loop diuretics should alert to the presence of a low cardiac output state.

Similar content being viewed by others
Abbreviations
- ACE:
-
Angiotensin converting enzyme
- ADHF:
-
Acute decompensated heart failure
- AF:
-
Atrial fibrillation
- BMI:
-
Body mass index
- BNP:
-
B-type natriuretic peptide
- BUN:
-
Blood urea nitrogen
- CI:
-
Cardiac index
- CO:
-
Cardiac output
- CRT:
-
Cardiac resynchronization therapy
- DLCO:
-
Diffusion capacity of carbon monoxide
- eGFR:
-
Estimated glomerular filtration rate
- FEV1:
-
Forced expiratory volume over the first second
- FVC:
-
Forced vital capacity
- HF:
-
Heart failure
- HFrEF:
-
Heart failure with reduced ejection fraction
- LA:
-
Left atrial
- LV:
-
Left ventricular
- LVAD:
-
Left ventricular assist device
- LVDD:
-
Left ventricular diastolic dysfunction
- LVOT:
-
Left ventricular outflow tract
- LVSD:
-
Left ventricular systolic dysfunction
- NGAL:
-
Neutrophil gelatinase–associated lipocalin
- OSA:
-
Obstructive sleep apnea
- PAC:
-
Pulmonary artery catheterization
- PAP:
-
Pulmonary artery pressure
- PAWP:
-
Pulmonary artery wedge pressure
- Pcap:
-
Pulmonary capillary pressure
- PH:
-
Pulmonary hypertension
- RBF:
-
Renal blood flow
- RV:
-
Right ventricle
- SGLT2:
-
Sodium glucose co-transporter 2
- SIRS:
-
Systemic inflammatory response syndrome
- WRF:
-
Worsening renal function
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Shah N, Madanieh R, Alkan M, Dogar MU, Kosmas CE, Vittorio TJ. A perspective on diuretic resistance in chronic congestive heart failure. Ther Adv Cardiovasc Dis. 2017;11(10):271–8. https://doi.org/10.1177/1753944717718717.
Ter Maaten JM, Rao VS, Hanberg JS, Perry Wilson F, Bellumkonda L, Assefa M, et al. Renal tubular resistance is the primary driver for loop diuretic resistance in acute heart failure. Eur J Heart Fail. 2017;19(8):1014–22. https://doi.org/10.1002/ejhf.757.
Verbrugge FH, Mullens W, Tang WH. Management of cardio-renal syndrome and diuretic resistance. Curr Treat Options Cardiovasc Med. 2016;18(2):11. https://doi.org/10.1007/s11936-015-0436-4.
Ramchandra R, Xing DT, Matear M, Lambert G, Allen AM, May CN. Neurohumoral interactions contributing to renal vasoconstriction and decreased renal blood flow in heart failure. Am J Physiol Regul Integr Comp Physiol. 2019;317(3):R386–96. https://doi.org/10.1152/ajpregu.00026.2019.
Kazancioğlu R. Risk factors for chronic kidney disease: an update. Kidney Int Suppl (2011). 2013;3(4):368–71. https://doi.org/10.1038/kisup.2013.79
Mullens W, Damman K, Testani JM, Martens P, Mueller C, Lassus J, et al. Evaluation of kidney function throughout the heart failure trajectory - a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2020;22(4):584–603. https://doi.org/10.1002/ejhf.1697. This position statement from the European Heart Failure Association describes the current models for understanding the development of CKD in the setting of heart failure, covering effects of heart failure and treatments on eGFR, sodium handling, and response to treatment.
George LK, Koshy SKG, Molnar MZ, Thomas F, Lu JL, Kalantar-Zadeh K et al. Heart failure increases the risk of adverse renal outcomes in patients with normal kidney function. Circ Heart Fail. 2017;10(8). https://doi.org/10.1161/CIRCHEARTFAILURE.116.003825
Damman K, Masson S, Lucci D, Gorini M, Urso R, Maggioni AP, et al. Progression of renal impairment and chronic kidney disease in chronic heart failure: an analysis from GISSI-HF. J Card Fail. 2017;23(1):2–9. https://doi.org/10.1016/j.cardfail.2016.09.006.
Lapman PG, Golduber GN, Le Jemtel TH. Heart failure treatment and renal function. Am Heart J. 2004;147(2):193–4. https://doi.org/10.1016/j.ahj.2003.10.003.
Elijovich F, Weinberger MH, Anderson CA, Appel LJ, Bursztyn M, Cook NR, et al. Salt sensitivity of blood pressure: a scientific statement from the American Heart Association. Hypertension. 2016;68(3):e7–46. https://doi.org/10.1161/HYP.0000000000000047.
Heer M, Baisch F, Kropp J, Gerzer R, Drummer C. High dietary sodium chloride consumption may not induce body fluid retention in humans. Am J Physiol Renal Physiol. 2000;278(4):F585–95. https://doi.org/10.1152/ajprenal.2000.278.4.F585.
Njoroge JN, Teerlink JR. Pathophysiology and therapeutic approaches to acute decompensated heart failure. Circ Res. 2021;128(10):1468–86. https://doi.org/10.1161/CIRCRESAHA.121.318186.
Binanay C, Califf RM, Hasselblad V, O’Connor CM, Shah MR, Sopko G, et al. Evaluation study of congestive heart failure and pulmonary artery catheterization effectiveness: the ESCAPE trial. JAMA. 2005;294(13):1625–33. https://doi.org/10.1001/jama.294.13.1625.
Hanberg JS, Sury K, Wilson FP, Brisco MA, Ahmad T, Ter Maaten JM, et al. Reduced cardiac index is not the dominant driver of renal dysfunction in heart failure. J Am Coll Cardiol. 2016;67(19):2199–208. https://doi.org/10.1016/j.jacc.2016.02.058.
Cody RJ, Ljungman S, Covit AB, Kubo SH, Sealey JE, Pondolfino K, et al. Regulation of glomerular filtration rate in chronic congestive heart failure patients. Kidney Int. 1988;34(3):361–7. https://doi.org/10.1038/ki.1988.189.
Stetz CW, Miller RG, Kelly GE, Raffin TA. Reliability of the thermodilution method in the determination of cardiac output in clinical practice. Am Rev Respir Dis. 1982;126(6):1001–4. https://doi.org/10.1164/arrd.1982.126.6.1001.
Bobbio E, Bollano E, Polte CL, Ekelund J, Rådegran G, Lundgren J, et al. Association between central haemodynamics and renal function in advanced heart failure: a nationwide study from Sweden. ESC Heart Fail. 2022. https://doi.org/10.1002/ehf2.13990.
Zelis R, Flaim SF, Liedtke AJ, Nellis SH. Cardiocirculatory dynamics in the normal and failing heart. Annu Rev Physiol. 1981;43:455–76. https://doi.org/10.1146/annurev.ph.43.030181.002323.
Zelis R, Flaim SF. Alterations in vasomotor tone in congestive heart failure. Prog Cardiovasc Dis. 1982;24(6):437–59. https://doi.org/10.1016/0033-0620(82)90012-3.
Ramchandra R, Xing DT, Matear M, Lambert G, Allen AM, May CN. Neurohumoral interactions contributing to renal vasoconstriction and decreased renal blood flow in heart failure. Am J Physiol Regul Integr Comp Physiol. 2019;317(3):R386–96. https://doi.org/10.1152/ajpregu.00026.2019.
Afkarian M, Zelnick LR, Hall YN, Heagerty PJ, Tuttle K, Weiss NS, et al. Clinical manifestations of kidney disease among US adults with diabetes, 1988–2014. JAMA. 2016;316(6):602–10. https://doi.org/10.1001/jama.2016.10924.
Weldegiorgis M, Woodward M. The impact of hypertension on chronic kidney disease and end-stage renal disease is greater in men than women: a systematic review and meta-analysis. BMC Nephrol. 2020;21(1):506. https://doi.org/10.1186/s12882-020-02151-7.
Navaneethan SD, Zoungas S, Caramori ML, Chan JCN, Heerspink HJL, Hurst C, et al. Diabetes management in chronic kidney disease: synopsis of the 2020 KDIGO clinical practice guideline. Ann Intern Med. 2021;174(3):385–94. https://doi.org/10.7326/M20-5938.
Somkearti P, Chattakul P, Khamsai S, Limpawattana P, Chindaprasirt J, Chotmongkol V, et al. Predictors of chronic kidney disease in obstructive sleep apnea patients. Multidiscip Respir Med. 2020;15(1):470. https://doi.org/10.4081/mrm.2020.470.
Rimke AN, Ahmed SB, Turin TC, Pendharkar SR, Raneri JK, Lynch EJ, et al. Effect of CPAP therapy on kidney function in patients with chronic kidney disease: a pilot randomized controlled trial. Chest. 2021;159(5):2008–19. https://doi.org/10.1016/j.chest.2020.11.052.
Hall JE, doCarmo JM, da Silva AA, Wang Z, Hall ME. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116(6):991–1006. https://doi.org/10.1161/CIRCRESAHA.116.305697.
D’Agati VD, Chagnac A, de Vries AP, Levi M, Porrini E, Herman-Edelstein M, et al. Obesity-related glomerulopathy: clinical and pathologic characteristics and pathogenesis. Nat Rev Nephrol. 2016;12(8):453–71. https://doi.org/10.1038/nrneph.2016.75.
Boorsma EM, Ter Maaten JM, Voors AA, van Veldhuisen DJ. Renal compression in heart failure: the renal tamponade hypothesis. JACC Heart Fail. 2022;10(3):175–83. https://doi.org/10.1016/j.jchf.2021.12.005.
Mullens W, Abrahams Z, Francis GS, Sokos G, Taylor DO, Starling RC, et al. Importance of venous congestion for worsening of renal function in advanced decompensated heart failure. J Am Coll Cardiol. 2009;53(7):589–96. https://doi.org/10.1016/j.jacc.2008.05.068.
Zhigalov K, Sá MPBO, Arjomandi Rad A, et al. The impact of obesity on left ventricular assist device outcomes. Medicina (Kaunas). 2020;56(11):556. Published 2020 Oct 23. https://doi.org/10.3390/medicina56110556.
Molina EJ, Shah P, Kiernan MS, Cornwell WK, Copeland H, Takeda K, et al. The Society of Thoracic Surgeons Intermacs 2020 annual report. Ann Thorac Surg. 2021;111(3):778–92. https://doi.org/10.1016/j.athoracsur.2020.12.038.
Butler J, Geisberg C, Howser R, Portner PM, Rogers JG, Deng MC, et al. Relationship between renal function and left ventricular assist device use. Ann Thorac Surg. 2006;81(5):1745–51. https://doi.org/10.1016/j.athoracsur.2005.11.061.
Ross DW, Stevens GR, Wanchoo R, Majure DT, Jauhar S, Fernandez HA, et al. Left ventricular assist devices and the kidney. Clin J Am Soc Nephrol. 2018;13(2):348–55. https://doi.org/10.2215/CJN.04670417.
Brisco MA, Kimmel SE, Coca SG, Putt ME, Jessup M, Tang WW, et al. Prevalence and prognostic importance of changes in renal function after mechanical circulatory support. Circ Heart Fail. 2014;7(1):68–75. https://doi.org/10.1161/CIRCHEARTFAILURE.113.000507.
Yalcin YC, Muslem R, Veen KM, Soliman OI, Hesselink DA, Constantinescu AA, et al. Impact of continuous flow left ventricular assist device therapy on chronic kidney disease: a longitudinal multicenter study. J Card Fail. 2020;26(4):333–41. https://doi.org/10.1016/j.cardfail.2020.01.010. A longitudinal study on LVAD recipients that demonstrated improved renal function in the early stages after initial placement of LVAD device and with eventual regression in later stages after LVAD placement.
Bartfay SE, Kolsrud O, Wessman P, Dellgren G, Karason K. The trajectory of renal function following mechanical circulatory support and subsequent heart transplantation. ESC Heart Fail. 2022. https://doi.org/10.1002/ehf2.13943.
Hasin T, Marmor Y, Kremers W, Topilsky Y, Severson CJ, Schirger JA, et al. Readmissions after implantation of axial flow left ventricular assist device. J Am Coll Cardiol. 2013;61(2):153–63. https://doi.org/10.1016/j.jacc.2012.09.041.
Farmakis D, Agostoni P, Baholli L, Bautin A, Comin-Colet J, Crespo-Leiro MG, et al. A pragmatic approach to the use of inotropes for the management of acute and advanced heart failure: an expert panel consensus. Int J Cardiol. 2019;297:83–90. https://doi.org/10.1016/j.ijcard.2019.09.005.
Obi Y, Kim T, Kovesdy CP, Amin AN, Kalantar-Zadeh K. Current and potential therapeutic strategies for hemodynamic cardiorenal syndrome. Cardiorenal Med. 2016;6(2):83–98. https://doi.org/10.1159/000441283.
Sarnak MJ. A patient with heart failure and worsening kidney function. Clin J Am Soc Nephrol. 2014;9(10):1790–8. https://doi.org/10.2215/CJN.11601113.
Leier CV, Heban PT, Huss P, Bush CA, Lewis RP. Comparative systemic and regional hemodynamic effects of dopamine and dobutamine in patients with cardiomyopathic heart failure. Circulation. 1978;58(3 Pt 1):466–75. https://doi.org/10.1161/01.cir.58.3.466.
Leier CV. Regional blood flow responses to vasodilators and inotropes in congestive heart failure. Am J Cardiol. 1988;62(8):86E-93E. https://doi.org/10.1016/s0002-9149(88)80019-5.
Sato Y, Matsuzawa H, Eguchi S. Comparative study of effects of adrenaline, dobutamine and dopamine on systemic hemodynamics and renal blood flow in patients following open heart surgery. Jpn Circ J. 1982;46(10):1059–72. https://doi.org/10.1253/jcj.46.1059.
Al-Hesayen A, Parker JD. The effects of dobutamine on renal sympathetic activity in human heart failure. J Cardiovasc Pharmacol. 2008;51(5):434–6. https://doi.org/10.1097/FJC.0b013e3181684026.
Ramchandra R, Xing DT, Matear M, Lambert G, Allen AM, May CN. Neurohumoral interactions contributing to renal vasoconstriction and decreased renal blood flow in heart failure. Am J Physiol Regul Integr Comp Physiol. 2019;317(3):R386–96. https://doi.org/10.1152/ajpregu.00026.2019.
Gilbert C, Cherney DZ, Parker AB, Mak S, Floras JS, Al-Hesayen A, et al. Hemodynamic and neurochemical determinates of renal function in chronic heart failure. Am J Physiol Regul Integr Comp Physiol. 2016;310(2):R167–75. https://doi.org/10.1152/ajpregu.00190.2015.
Mullens W, Verbrugge FH, Nijst P, Tang WHW. Renal sodium avidity in heart failure: from pathophysiology to treatment strategies. Eur Heart J. 2017;38(24):1872–82. https://doi.org/10.1093/eurheartj/ehx035.
Lytvyn Y, Burns KD, Testani JM, Lytvyn A, Ambinathan JPN, Osuntokun O, et al. Renal hemodynamics and renin-angiotensin-aldosterone system profiles in patients with heart failure. J Card Fail. 2022;28(3):385–93. https://doi.org/10.1016/j.cardfail.2021.08.015. This study obtained invasive measures of renal hemodynamics RAAS hormones in heart failure patients and followed responses to inotropic support, demonstrating increased RAAS activation in CHF that improved with inotropic support.
Lannemyr L, Ricksten SE, Rundqvist B, Andersson B, Bartfay SE, Ljungman C, et al. Differential effects of levosimendan and dobutamine on glomerular filtration rate in patients with heart failure and renal impairment:a randomized double-blind controlled trial. J Am Heart Assoc. 2018;7(16):e008455. https://doi.org/10.1161/JAHA.117.008455.
Klein L, Massie BM, Leimberger JD, O’Connor CM, Piña IL, Adams KF, et al. Admission or changes in renal function during hospitalization for worsening heart failure predict postdischarge survival: results from the Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure (OPTIME-CHF). Circ Heart Fail. 2008;1(1):25–33. https://doi.org/10.1161/CIRCHEARTFAILURE.107.746933.
Hammond DA, Smith MN, Lee KC, Honein D, Quidley AM. Acute decompensated heart failure. J Intensive Care Med. 2018;33(8):456–66. https://doi.org/10.1177/0885066616669494.
Melenovsky V, Andersen MJ, Andress K, Reddy YN, Borlaug BA. Lung congestion in chronic heart failure: haemodynamic, clinical, and prognostic implications. Eur J Heart Fail. 2015;17(11):1161–71. https://doi.org/10.1002/ejhf.417.
Jain CC, Tschirren J, Reddy YNV, Melenovsky V, Redfield M, Borlaug BA. Subclinical pulmonary congestion and abnormal hemodynamics in heart failure with preserved ejection fraction. JACC Cardiovasc Imaging. 2022;15(4):629–37. https://doi.org/10.1016/j.jcmg.2021.09.017.
Dixon DL, De Pasquale CG, Lawrence MD, Cavallaro E, Rubino V, Bersten AD. Lung fluid clearance in chronic heart failure patients. Int J Cardiol. 2017;244:245–7. https://doi.org/10.1016/j.ijcard.2017.05.096.
Stewart GM, Johnson BD, Sprecher DL, Reddy YNV, Obokata M, Goldsmith S, et al. Targeting pulmonary capillary permeability to reduce lung congestion in heart failure: a randomized, controlled pilot trial. Eur J Heart Fail. 2020;22(9):1641–5. https://doi.org/10.1002/ejhf.1809.
Magnussen H, Canepa M, Zambito PE, Brusasco V, Meinertz T, Rosenkranz S. What can we learn from pulmonary function testing in heart failure? Eur J Heart Fail. 2017;19(10):1222–9. https://doi.org/10.1002/ejhf.946.
Kawakami R, Nakada Y, Hashimoto Y, Ueda T, Nakagawa H, Nishida T, et al. Prevalence and prognostic significance of pulmonary function test abnormalities in hospitalized patients with acute decompensated heart failure with preserved and reduced ejection fraction. Circ J. 2021;85(9):1426–34. https://doi.org/10.1253/circj.CJ-20-1069.
Cuttica MJ, Colangelo LA, Shah SJ, Lima J, Kishi S, Arynchyn A, et al. Loss of lung health from young adulthood and cardiac phenotypes in middle age. Am J Respir Crit Care Med. 2015;192(1):76–85. https://doi.org/10.1164/rccm.201501-0116OC.
Cundrle I, Olson LJ, Johnson BD. Pulmonary limitations in heart failure. Clin Chest Med. 2019;40(2):439–48. https://doi.org/10.1016/j.ccm.2019.02.010.
Dubé BP, Agostoni P, Laveneziana P. Exertional dyspnoea in chronic heart failure: the role of the lung and respiratory mechanical factors. Eur Respir Rev. 2016;25(141):317–32. https://doi.org/10.1183/16000617.0048-2016.
Obokata M, Olson TP, Reddy YNV, Melenovsky V, Kane GC, Borlaug BA. Haemodynamics, dyspnoea, and pulmonary reserve in heart failure with preserved ejection fraction. Eur Heart J. 2018;39(30):2810–21. https://doi.org/10.1093/eurheartj/ehy268.
Chase SC, Wheatley CM, Olson LJ, Beck KC, Wentz RJ, Snyder EM et al. Impact of chronic systolic heart failure on lung structure-function relationships in large airways. Physiol Rep. 2016;4(13). https://doi.org/10.14814/phy2.12867.
Chang HC, Huang WM, Yu WC, Cheng HM, Guo CY, Chiang CE, et al. Prognostic role of pulmonary function in patients with heart failure with reduced ejection fraction. J Am Heart Assoc. 2022;11(7):e023422. https://doi.org/10.1161/JAHA.121.023422.
Eckhardt CM, Balte PP, Barr RG, Bertoni AG, Bhatt SP, Cuttica M, et al. Lung function impairment and risk of incident heart failure: the NHLBI pooled cohorts study. Eur Heart J. 2022. https://doi.org/10.1093/eurheartj/ehac205.
Enriquez-Sarano M, Rossi A, Seward JB, Bailey KR, Tajik AJ. Determinants of pulmonary hypertension in left ventricular dysfunction. J Am Coll Cardiol. 1997;29(1):153–9. https://doi.org/10.1016/s0735-1097(96)00436-6.
Vachiéry JL, Adir Y, Barberà JA, Champion H, Coghlan JG, Cottin V, et al. Pulmonary hypertension due to left heart diseases. J Am Coll Cardiol. 2013;62(25 Suppl):D100–8. https://doi.org/10.1016/j.jacc.2013.10.033.
Opitz CF, Hoeper MM, Gibbs JS, Kaemmerer H, Pepke-Zaba J, Coghlan JG, et al. Pre-capillary, combined, and post-capillary pulmonary hypertension: a pathophysiological continuum. J Am Coll Cardiol. 2016;68(4):368–78. https://doi.org/10.1016/j.jacc.2016.05.047.
Rosenkranz S, Gibbs JS, Wachter R, De Marco T, Vonk-Noordegraaf A, Vachiéry JL. Left ventricular heart failure and pulmonary hypertension. Eur Heart J. 2016;37(12):942–54. https://doi.org/10.1093/eurheartj/ehv512.
Verbrugge FH, Guazzi M, Testani JM, Borlaug BA. Altered hemodynamics and end-organ damage in heart failure: impact on the lung and kidney. Circulation. 2020;142(10):998–1012. https://doi.org/10.1161/CIRCULATIONAHA.119.045409.
Al-Omary MS, Sugito S, Boyle AJ, Sverdlov AL, Collins NJ. Pulmonary hypertension due to left heart disease: diagnosis, pathophysiology, and therapy. Hypertension. 2020;75(6):1397–408. https://doi.org/10.1161/HYPERTENSIONAHA.119.14330.
Maron BA, Kovacs G, Vaidya A, Bhatt DL, Nishimura RA, Mak S, et al. Cardiopulmonary hemodynamics in pulmonary hypertension and heart failure: JACC review topic of the week. J Am Coll Cardiol. 2020;76(22):2671–81. https://doi.org/10.1016/j.jacc.2020.10.007.
Reddy YNV, Borlaug BA. Pulmonary hypertension in left heart disease. Clin Chest Med. 2021;42(1):39–58. https://doi.org/10.1016/j.ccm.2020.11.002. This review summarizes contemporary understanding of pulmonary hypertension in left heart disease with a focus on improving the diagnosis of pre- and post-capillary pulmonary hypertension in left heart failure.
Lam CS, Roger VL, Rodeheffer RJ, Borlaug BA, Enders FT, Redfield MM. Pulmonary hypertension in heart failure with preserved ejection fraction: a community-based study. J Am Coll Cardiol. 2009;53(13):1119–26. https://doi.org/10.1016/j.jacc.2008.11.051.
Charalampopoulos A, Howard LS, Tzoulaki I, Gin-Sing W, Grapsa J, Wilkins MR, et al. Response to pulmonary arterial hypertension drug therapies in patients with pulmonary arterial hypertension and cardiovascular risk factors. Pulm Circ. 2014;4(4):669–78. https://doi.org/10.1086/678512.
Tedford RJ, Hassoun PM, Mathai SC, Girgis RE, Russell SD, Thiemann DR, et al. Pulmonary capillary wedge pressure augments right ventricular pulsatile loading. Circulation. 2012;125(2):289–97. https://doi.org/10.1161/CIRCULATIONAHA.111.051540.
Vachiéry JL, Tedford RJ, Rosenkranz S, Palazzini M, Lang I, Guazzi M et al. Pulmonary hypertension due to left heart disease. Eur Respir J. 2019;53(1). https://doi.org/10.1183/13993003.01897-2018.
Vonk Noordegraaf A, Westerhof BE, Westerhof N. The relationship between the right ventricle and its load in pulmonary hypertension. J Am Coll Cardiol. 2017;69(2):236–43. https://doi.org/10.1016/j.jacc.2016.10.047.
Chatterjee NA, Lewis GD. What is the prognostic significance of pulmonary hypertension in heart failure? Circ Heart Fail. 2011;4(5):541–5. https://doi.org/10.1161/CIRCHEARTFAILURE.111.963785.
Fayyaz AU, Edwards WD, Maleszewski JJ, Konik EA, DuBrock HM, Borlaug BA, et al. Global pulmonary vascular remodeling in pulmonary hypertension associated with heart failure and preserved or reduced ejection fraction. Circulation. 2018;137(17):1796–810. https://doi.org/10.1161/CIRCULATIONAHA.117.031608.
Cogliati C, Ceriani E, Gambassi G, De Matteis G, Perlini S, Perrone T, et al. Phenotyping congestion in patients with acutely decompensated heart failure with preserved and reduced ejection fraction: the decongestion during therapy for acute decompensated heart failure in HFpEF vs HFrEF- DRY-OFF study. Eur J Intern Med. 2022;97:69–77. https://doi.org/10.1016/j.ejim.2021.11.010.
Ander DS, Jaggi M, Rivers E, Rady MY, Levine TB, Levine AB, et al. Undetected cardiogenic shock in patients with congestive heart failure presenting to the emergency department. Am J Cardiol. 1998;82(7):888–91. https://doi.org/10.1016/s0002-9149(98)00497-4.
Tanawuttiwat T, Lande J, Smeets P, Gerritse B, Nazarian S, Guallar E, et al. Atrial fibrillation burden and subsequent heart failure events in patients with cardiac resynchronization therapy devices. J Cardiovasc Electrophysiol. 2020;31(6):1519–26. https://doi.org/10.1111/jce.14444.
Andriulli J, Coles J, Hettrick DA. Association between decreased intra-thoracic impedance and ventricular tachyarrhythmias. Int J Cardiol. 2008;123(3):333–4. https://doi.org/10.1016/j.ijcard.2006.11.153.
Drozd M, Garland E, Walker AMN, Slater TA, Koshy A, Straw S, Gierula J, Paton M, Lowry J, Sapsford R, Witte KK, Kearney MT, Cubbon RM. Infection-related hospitalization in heart failure with reduced ejection fraction: a prospective observational cohort study. Circ Heart Fail. 2020;13(5):e006746. https://doi.org/10.1161/CIRCHEARTFAILURE.119.006746.
Walker AMN, Drozd M, Hall M, Patel PA, Paton M, Lowry J, Gierula J, Byrom R, Kearney L, Sapsford RJ, Witte KK, Kearney MT, Cubbon RM. Prevalence and predictors of sepsis death in patients with chronic heart failure and reduced left ventricular ejection fraction. J Am Heart Assoc. 2018;7(20):e009684. https://doi.org/10.1161/JAHA.118.009684.
Njoroge JN, Teerlink JR. Pathophysiology and therapeutic approaches to acute decompensated heart failure. Circ Res. 2021;128(10):1468–86. https://doi.org/10.1161/CIRCRESAHA.121.318186.
Antonietta CM, Calvi E, Faggiano A, Maffeis C, Bosisio M, De Stefano M, et al. Impact of loop diuretic on outcomes in patients with heart failure and reduced ejection fraction. Curr Heart Fail Rep. 2022;19(1):15–25. https://doi.org/10.1007/s11897-021-00538-7.
Damman K, Kjekshus J, Wikstrand J, Cleland JG, Komajda M, Wedel H, et al. Loop diuretics, renal function and clinical outcome in patients with heart failure and reduced ejection fraction. Eur J Heart Fail. 2016;18(3):328–36. https://doi.org/10.1002/ejhf.462.
Ahmad T, Jackson K, Rao VS, Tang WHW, Brisco-Bacik MA, Chen HH, et al. Worsening renal function in patients with acute heart failure undergoing aggressive diuresis is not associated with tubular injury. Circulation. 2018;137(19):2016–28. https://doi.org/10.1161/CIRCULATIONAHA.117.030112.
Valente MA, Voors AA, Damman K, Van Veldhuisen DJ, Massie BM, O’Connor CM, et al. Diuretic response in acute heart failure: clinical characteristics and prognostic significance. Eur Heart J. 2014;35(19):1284–93. https://doi.org/10.1093/eurheartj/ehu065.
Emmens JE, Ter Maaten JM, Matsue Y, Figarska SM, Sama IE, Cotter G, et al. Worsening renal function in acute heart failure in the context of diuretic response. Eur J Heart Fail. 2022;24(2):365–74. https://doi.org/10.1002/ejhf.2384.
Chen JJ, Lee TH, Kuo G, Yen CL, Chen SW, Chu PH, et al. Acute kidney disease after acute decompensated heart failure. Kidney Int Rep. 2022;7(3):526–36. https://doi.org/10.1016/j.ekir.2021.12.033.
Horiuchi Y, Wettersten N, van Veldhuisen DJ, Mueller C, Filippatos G, Nowak R, et al. Decongestion, kidney injury and prognosis in patients with acute heart failure. Int J Cardiol. 2022;354:29–37. https://doi.org/10.1016/j.ijcard.2022.02.026. A retrospective study on diuretic response and renal tubular damage that shows kidney tubular damage in the setting of adequate decongestion was not associated with worse outcomes, while tubular damage in the absence of adequate decongestion is a bad prognostic sign.
Abraham WT, Stevenson LW, Bourge RC, Lindenfeld JA, Bauman JG, Adamson PB, et al. Sustained efficacy of pulmonary artery pressure to guide adjustment of chronic heart failure therapy: complete follow-up results from the CHAMPION randomised trial. Lancet. 2016;387(10017):453–61. https://doi.org/10.1016/S0140-6736(15)00723-0.
Angermann CE, Assmus B, Anker SD, Asselbergs FW, Brachmann J, Brett ME, et al. Pulmonary artery pressure-guided therapy in ambulatory patients with symptomatic heart failure: the CardioMEMS European Monitoring Study for Heart Failure (MEMS-HF). Eur J Heart Fail. 2020;22(10):1891–901. https://doi.org/10.1002/ejhf.1943.
Lindenfeld J, Zile MR, Desai AS, Bhatt K, Ducharme A, Horstmanshof D, et al. Haemodynamic-guided management of heart failure (GUIDE-HF): a randomised controlled trial. Lancet. 2021;398(10304):991–1001. https://doi.org/10.1016/S0140-6736(21)01754-2.
Adamson PB, Abraham WT, Stevenson LW, Desai AS, Lindenfeld J, Bourge RC, Bauman J. Pulmonary artery pressure-guided heart failure management reduces 30-day readmissions. Circ Heart Fail. 2016;9(6):e002600. https://doi.org/10.1161/CIRCHEARTFAILURE.115.002600.
Shavelle DM, Desai AS, Abraham WT, Bourge RC, Raval N, Rathman LD, et al. Lower rates of heart failure and all-cause hospitalizations during pulmonary artery pressure-guided therapy for ambulatory heart failure: one-year outcomes from the CardioMEMS post-approval study. Circ Heart Fail. 2020;13(8):e006863. https://doi.org/10.1161/CIRCHEARTFAILURE.119.006863.
Schrier RW. Role of diminished renal function in cardiovascular mortality: marker or pathogenetic factor? J Am Coll Cardiol. 2006;47(1):1–8. https://doi.org/10.1016/j.jacc.2005.07.067.
Bayliss J, Norell M, Canepa-Anson R, Sutton G, Poole-Wilson P. Untreated heart failure: clinical and neuroendocrine effects of introducing diuretics. Br Heart J. 1987;57(1):17–22. https://doi.org/10.1136/hrt.57.1.17.
Ceriani E, Casazza G, Peta J, Torzillo D, Furlotti S, Cogliati C. Residual congestion and long-term prognosis in acutely decompensated heart failure patients. Intern Emerg Med. 2020;15(4):719–24. https://doi.org/10.1007/s11739-020-02326-y.
Damman K, Beusekamp JC, Boorsma EM, Swart HP, Smilde TDJ, Elvan A, et al. Randomized, double-blind, placebo-controlled, multicentre pilot study on the effects of empagliflozin on clinical outcomes in patients with acute decompensated heart failure (EMPA-RESPONSE-AHF). Eur J Heart Fail. 2020;22(4):713–22. https://doi.org/10.1002/ejhf.1713.
Boorsma EM, Ter Maaten JM, Damman K, Dinh W, Gustafsson F, Goldsmith S, et al. Congestion in heart failure: a contemporary look at physiology, diagnosis and treatment. Nat Rev Cardiol. 2020;17(10):641–55. https://doi.org/10.1038/s41569-020-0379-7.
Mullens W, Martens P, Forouzan O, Dauw J, Vercammen J, Luwel E, et al. Effects of dapagliflozin on congestion assessed by remote pulmonary artery pressure monitoring. ESC Heart Fail. 2020;7(5):2071–3. https://doi.org/10.1002/ehf2.12850.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Decompensated Heart Failure.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stencel, J., Rajapreyar, I., Samson, R. et al. Comprehensive and Safe Decongestion in Acutely Decompensated Heart Failure. Curr Heart Fail Rep 19, 364–374 (2022). https://doi.org/10.1007/s11897-022-00573-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-022-00573-y