Abstract
Purpose of Review
Recognition and treatment of sleep apnea is an important but easily overlooked aspect of care in the heart failure patient. This review summarizes the data behind the recommendations in current practice guidelines and highlights recent developments in treatment options.
Recent Findings
Neuromodulation using hypoglossal nerve stimulation has been increasingly used for treatment of OSA; however, it has not been studied in the heart failure population. Alternatively, phrenic nerve stimulation for treatment of CSA is effective for heart failure patients, and cardiac resynchronization therapy can be effective in improving CSA in pacing-induced cardiomyopathy.
Summary
In patients suspected to have sleep apnea, polysomnography is recommended to better understand the prognosis and treatment options. Positive airway pressure is the standard treatment for sleep apnea; however, neurostimulation can be especially effective in those with predominantly central events. Understanding the pathophysiology of sleep apnea can guide further management decisions.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Javaheri S. Sleep disorders in systolic heart failure: a prospective study of 100 male patients. The final report. Int J Cardiol. 2006;106(1):21–8. https://doi.org/10.1016/j.ijcard.2004.12.068.
• Javaheri S, Brown LK, Abraham WT, Khayat R. Apneas of heart failure and phenotype-guided treatments: part one: OSA. Chest. 2020;157(2):394–402. https://doi.org/10.1016/j.chest.2019.02.407. This review was written by leaders in the field, clearly explaining a phenotypic approach to management of OSA in heart failure patients.
Wang H, Parker JD, Newton GE, Floras JS, Mak S, Chiu KL, et al. Influence of obstructive sleep apnea on mortality in patients with heart failure. J Am Coll Cardiol. 2007;49(15):1625–31. https://doi.org/10.1016/j.jacc.2006.12.046.
Lanfranchi PA, Braghiroli A, Bosimini E, Mazzuero G, Colombo R, Donner CF, et al. Prognostic value of nocturnal Cheyne-Stokes respiration in chronic heart failure. Circulation. 1999;99(11):1435–40. https://doi.org/10.1161/01.cir.99.11.1435.
Hanly PJ, Zuberi-Khokhar NS. Increased mortality associated with Cheyne-Stokes respiration in patients with congestive heart failure. Am J Respir Crit Care Med. 1996;153(1):272–6. https://doi.org/10.1164/ajrccm.153.1.8542128.
Brack T, Thuer I, Clarenbach CF, Senn O, Noll G, Russi EW, et al. Daytime Cheyne-Stokes respiration in ambulatory patients with severe congestive heart failure is associated with increased mortality. Chest. 2007;132(5):1463–71. https://doi.org/10.1378/chest.07-0121.
Khayat R, Abraham W, Patt B, Brinkman V, Wannemacher J, Porter K, et al. Central sleep apnea is a predictor of cardiac readmission in hospitalized patients with systolic heart failure. J Card Fail. 2012;18(7):534–40. https://doi.org/10.1016/j.cardfail.2012.05.003.
Khayat R, Jarjoura D, Porter K, Sow A, Wannemacher J, Dohar R, et al. Sleep disordered breathing and post-discharge mortality in patients with acute heart failure. Eur Heart J. 2015;36(23):1463–9. https://doi.org/10.1093/eurheartj/ehu522.
Aurora RN, Caffo B, Crainiceanu C, Punjabi NM. Correlating subjective and objective sleepiness: revisiting the association using survival analysis. Sleep. 2011;34(12):1707–14. https://doi.org/10.5665/sleep.1442.
Arzt M, Young T, Finn L, Skatrud JB, Ryan CM, Newton GE, et al. Sleepiness and sleep in patients with both systolic heart failure and obstructive sleep apnea. Arch Intern Med. 2006;166(16):1716–22. https://doi.org/10.1001/archinte.166.16.1716.
Mehra R, Wang L, Andrews N, Tang WHW, Young JB, Javaheri S, et al. Dissociation of objective and subjective daytime sleepiness and biomarkers of systemic inflammation in sleep-disordered breathing and systolic heart failure. J Clin Sleep Med. 2017;13(12):1411–22. https://doi.org/10.5664/jcsm.6836.
Laugsand LE, Strand LB, Platou C, Vatten LJ, Janszky I. Insomnia and the risk of incident heart failure: a population study. Eur Heart J. 2014;35(21):1382–93. https://doi.org/10.1093/eurheartj/eht019.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):E147–239. https://doi.org/10.1016/j.jacc.2013.05.019.
Richard B, Berry SFQ, Abreu AR. Marietta L. Bibbs, Lourdes DelRosso, Susan M. Harding, Molly-Min Mao, David T. Plante, Mark R Pressman, Matthew M.Troester, Bradley V. Vaughn. The AASM manual for the scoring of sleep and associated events. Rules, terminology and technical specifications. Darien, Illinois: American Academy of. Sleep Med. 2020.
Aurora RN, Patil SP, Punjabi NM. Portable sleep monitoring for diagnosing sleep apnea in hospitalized patients with heart failure. Chest. 2018;154(1):91–8. https://doi.org/10.1016/j.chest.2018.04.008.
Kauta SR, Keenan BT, Goldberg L, Schwab RJ. Diagnosis and treatment of sleep disordered breathing in hospitalized cardiac patients: a reduction in 30-day hospital readmission rates. J Clin Sleep Med. 2014;10(10):1051–9. https://doi.org/10.5664/jcsm.4096.
Bucca CB, Brussino L, Battisti A, Mutani R, Rolla G, Mangiardi L, et al. Diuretics in obstructive sleep apnea with diastolic heart failure. Chest. 2007;132(2):440–6. https://doi.org/10.1378/chest.07-0311.
Javaheri S, Barbe F, Campos-Rodriguez F, Dempsey JA, Khayat R, Javaheri S, et al. Sleep apnea: types, mechanisms, and clinical cardiovascular consequences. J Am Coll Cardiol. 2017;69(7):841–58. https://doi.org/10.1016/j.jacc.2016.11.069.
Costanzo MR. Central sleep apnea in patients with heart failure—how to screen, how to treat. Curr Heart Fail Rep. 2020;17(5):277–87. https://doi.org/10.1007/s11897-020-00472-0.
Hanly P, Zuberi N, Gray R. Pathogenesis of Cheyne-Stokes respiration in patients with congestive heart failure. Relationship to arterial PCO2. Chest. 1993;104(4):1079–84. https://doi.org/10.1378/chest.104.4.1079.
Naughton M, Benard D, Tam A, Rutherford R, Bradley TD. Role of hyperventilation in the pathogenesis of central sleep apneas in patients with congestive heart failure. Am Rev Respir Dis. 1993;148(2):330–8. https://doi.org/10.1164/ajrccm/148.2.330.
Spaak J, Egri ZJ, Kubo T, Yu E, Ando SI, Kaneko Y, et al. Muscle sympathetic nerve activity during wakefulness in heart failure patients with and without sleep apnea. Hypertension. 2005;46(6):1327–32. https://doi.org/10.1161/01.HYP.0000193497.45200.66.
Naughton MT, Rahman MA, Hara K, Floras JS, Bradley TD. Effect of continuous positive airway pressure on intrathoracic and left ventricular transmural pressures in patients with congestive heart failure. Circulation. 1995;91(6):1725–31. https://doi.org/10.1161/01.cir.91.6.1725.
Kasai T, Floras JS, Bradley TD. Sleep apnea and cardiovascular disease: a bidirectional relationship. Circulation. 2012;126(12):1495–510. https://doi.org/10.1161/CIRCULATIONAHA.111.070813.
• Javaheri S, Brown LK, Khayat RN. Update on apneas of heart failure with reduced ejection fraction: emphasis on the physiology of treatment: Part 2: Central Sleep Apnea. Chest. 2020;157(6):1637–46. https://doi.org/10.1016/j.chest.2019.12.020. This review was written by leaders in the field, clearly explaining a phenotypic approach to management of CSA in heart failure patients.
Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263–76.
Giles TL, Lasserson TJ, Smith BH, White J, Wright J, Cates CJ. Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev. 2006;3:CD001106. https://doi.org/10.1002/14651858.CD001106.pub3.
Engleman HM, Martin SE, Deary IJ, Douglas NJ. Effect of continuous positive airway pressure treatment on daytime function in sleep apnoea/hypopnoea syndrome. Lancet. 1994;343(8897):572–5. https://doi.org/10.1016/s0140-6736(94)91522-9.
Egea CJ, Aizpuru F, Pinto JA, Ayuela JM, Ballester E, Zamarron C, et al. Cardiac function after CPAP therapy in patients with chronic heart failure and sleep apnea: a multicenter study. Sleep Med. 2008;9(6):660–6. https://doi.org/10.1016/j.sleep.2007.06.018.
Kaneko Y, Floras JS, Usui K, Plante J, Tkacova R, Kubo T, et al. Cardiovascular effects of continuous positive airway pressure in patients with heart failure and obstructive sleep apnea. N Engl J Med. 2003;348(13):1233–41. https://doi.org/10.1056/NEJMoa022479.
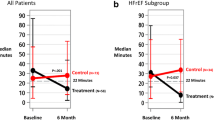
Bradley TD, Logan AG, Kimoff RJ, Series F, Morrison D, Ferguson K, et al. Continuous positive airway pressure for central sleep apnea and heart failure. N Engl J Med. 2005;353(19):2025–33. https://doi.org/10.1056/NEJMoa051001.
Arzt M, Floras JS, Logan AG, Kimoff RJ, Series F, Morrison D, et al. Suppression of central sleep apnea by continuous positive airway pressure and transplant-free survival in heart failure: a post hoc analysis of the Canadian Continuous Positive Airway Pressure for Patients with Central Sleep Apnea and Heart Failure Trial (CANPAP). Circulation. 2007;115(25):3173–80. https://doi.org/10.1161/CIRCULATIONAHA.106.683482.
Javaheri S. Effects of continuous positive airway pressure on sleep apnea and ventricular irritability in patients with heart failure. Circulation. 2000;101(4):392–7. https://doi.org/10.1161/01.cir.101.4.392.
Teschler H, Dohring J, Wang YM, Berthon-Jones M. Adaptive pressure support servo-ventilation: a novel treatment for Cheyne-Stokes respiration in heart failure. Am J Respir Crit Care Med. 2001;164(4):614–9. https://doi.org/10.1164/ajrccm.164.4.9908114.
Javaheri S, Brown LK, Randerath WJ. Positive airway pressure therapy with adaptive servoventilation: part 1: operational algorithms. Chest. 2014;146(2):514–23. https://doi.org/10.1378/chest.13-1776.
Sharma BK, Bakker JP, McSharry DG, Desai AS, Javaheri S, Malhotra A. Adaptive servoventilation for treatment of sleep-disordered breathing in heart failure: a systematic review and meta-analysis. Chest. 2012;142(5):1211–21. https://doi.org/10.1378/chest.12-0815.
Cowie MR, Woehrle H, Wegscheider K, Angermann C, d'Ortho MP, Erdmann E, et al. Adaptive servo-ventilation for central sleep apnea in systolic heart failure. N Engl J Med. 2015;373(12):1095–105. https://doi.org/10.1056/NEJMoa1506459.
Medicine AAoS. Special Safety Notice: ASV therapy for central sleep apnea patients with heart failure. 2015.
Willson GN, Wilcox I, Piper AJ, Flynn WE, Norman M, Grunstein RR, et al. Noninvasive pressure preset ventilation for the treatment of Cheyne-Stokes respiration during sleep. Eur Respir J. 2001;17(6):1250–7. https://doi.org/10.1183/09031936.01.99086101.
Kasai T, Narui K, Dohi T, Ishiwata S, Yoshimura K, Nishiyama S, et al. Efficacy of nasal bi-level positive airway pressure in congestive heart failure patients with cheyne-stokes respiration and central sleep apnea. Circ J. 2005;69(8):913–21. https://doi.org/10.1253/circj.69.913.
Dohi T, Kasai T, Narui K, Ishiwata S, Ohno M, Yamaguchi T, et al. Bi-level positive airway pressure ventilation for treating heart failure with central sleep apnea that is unresponsive to continuous positive airway pressure. Circ J. 2008;72(7):1100–5.
Kohnlein T, Welte T, Tan LB, Elliott MW. Assisted ventilation for heart failure patients with Cheyne-Stokes respiration. Eur Respir J. 2002;20(4):934–41. https://doi.org/10.1183/09031936.00.02622001.
Aurora RN, Chowdhuri S, Ramar K, Bista SR, Casey KR, Lamm CI, et al. The treatment of central sleep apnea syndromes in adults: practice parameters with an evidence-based literature review and meta-analyses. Sleep. 2012;35(1):17–40. https://doi.org/10.5665/sleep.1580.
Ramar K, Dort LC, Katz SG, Lettieri CJ, Harrod CG, Thomas SM, et al. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med. 2015;11(7):773–827. https://doi.org/10.5664/jcsm.4858.
Clark GT, Blumenfeld I, Yoffe N, Peled E, Lavie P. A crossover study comparing the efficacy of continuous positive airway pressure with anterior mandibular positioning devices on patients with obstructive sleep apnea. Chest. 1996;109(6):1477–83. https://doi.org/10.1378/chest.109.6.1477.
Eskafi M. Sleep apnoea in patients with stable congestive heart failure an intervention study with a mandibular advancement device. Swed Dent J Suppl. 2004;168:1–56.
Eskafi M, Cline C, Israelsson B, Nilner M. A mandibular advancement device reduces sleep disordered breathing in patients with congestive heart failure. Swed Dent J. 2004;28(4):155–63.
Cartwright RD. Effect of sleep position on sleep apnea severity. Sleep. 1984;7(2):110–4. https://doi.org/10.1093/sleep/7.2.110.
Permut I, Diaz-Abad M, Chatila W, Crocetti J, Gaughan JP, D'Alonzo GE, et al. Comparison of positional therapy to CPAP in patients with positional obstructive sleep apnea. J Clin Sleep Med. 2010;6(3):238–43.
Szollosi I, Roebuck T, Thompson B, Naughton MT. Lateral sleeping position reduces severity of central sleep apnea/Cheyne-Stokes respiration. Sleep. 2006;29(8):1045–51. https://doi.org/10.1093/sleep/29.8.1045.
Pinna GD, Robbi E, La Rovere MT, Taurino AE, Bruschi C, Guazzotti G, et al. Differential impact of body position on the severity of disordered breathing in heart failure patients with obstructive vs. central sleep apnoea. Eur J Heart Fail. 2015;17(12):1302–9. https://doi.org/10.1002/ejhf.410.
Joho S, Oda Y, Hirai T, Inoue H. Impact of sleeping position on central sleep apnea/Cheyne-Stokes respiration in patients with heart failure. Sleep Med. 2010;11(2):143–8. https://doi.org/10.1016/j.sleep.2009.05.014.
Strollo PJ Jr, Soose RJ, Maurer JT, de Vries N, Cornelius J, Froymovich O, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014;370(2):139–49. https://doi.org/10.1056/NEJMoa1308659.
FDA. Inspire® Upper Airway Stimulation – P130008/S039. 2020.
Yamauchi M, Satoh M, Kitahara T, Ota I, Strohl K. Nerve stimulation for the treatment of obstructive sleep apnea. Sleep Biol Rhythms. 2020;18(2):77–87. https://doi.org/10.1007/s41105-020-00252-2.
Abraham WT, Jagielski D, Oldenburg O, Augostini R, Krueger S, Kolodziej A, et al. Phrenic nerve stimulation for the treatment of central sleep apnea. Jacc-Heart Fail. 2015;3(5):360–9. https://doi.org/10.1016/j.jchf.2014.12.013.
Jagielski D, Ponikowski P, Augostini R, Kolodziej A, Khayat R, Abraham WT. Transvenous stimulation of the phrenic nerve for the treatment of central sleep apnoea: 12 months' experience with the remede((R)) System. Eur J Heart Fail. 2016;18(11):1386–93. https://doi.org/10.1002/ejhf.593.
Fudim M, Spector AR, Costanzo MR, Pokorney SD, Mentz RJ, Jagielski D, et al. Phrenic nerve stimulation for the treatment of central sleep apnea: a pooled cohort analysis. J Clin Sleep Med. 2019;15(12):1747–55. https://doi.org/10.5664/jcsm.8076.
• Barbieri F, Adukauskaite A, Heidbreder A, Brandauer E, Bergmann M, Stefani A, et al. Central sleep apnea and pacing-induced cardiomyopathy. Am J Cardiol. 2020. https://doi.org/10.1016/j.amjcard.2020.09.027. UPGRADE study demonstrates efficacy of CRT in those with CSA and pacing induced myopathy.
Barbieri F, Adukauskaite A, Senoner T, Rubatscher A, Schgor W, Stuhlinger M, et al. Supplemental dataset on the influence of cardiac resynchronisation therapy in pacing-induced cardiomyopathy and concomitant central sleep Apnea. Data Brief. 2020;33:106461. https://doi.org/10.1016/j.dib.2020.106461.
Sasayama S, Izumi T, Seino Y, Ueshima K, Asanoi H, C-HS G. Effects of nocturnal oxygen therapy on outcome measures in patients with chronic heart failure and Cheyne-Stokes respiration. Circ J. 2006;70(1):1–7. https://doi.org/10.1253/circj.70.1.
Shigemitsu M, Nishio K, Kusuyama T, Itoh S, Konno N, Katagiri T. Nocturnal oxygen therapy prevents progress of congestive heart failure with central sleep apnea. Int J Cardiol. 2007;115(3):354–60. https://doi.org/10.1016/j.ijcard.2006.03.018.
Toyama T, Seki R, Kasama S, Isobe N, Sakurai S, Adachi H, et al. Effectiveness of nocturnal home oxygen therapy to improve exercise capacity, cardiac function and cardiac sympathetic nerve activity in patients with chronic heart failure and central sleep apnea. Circ J. 2009;73(2):299–304. https://doi.org/10.1253/circj.cj-07-0297.
Center NIoHC. The impact of low-flow oxygen therapy on hospital admissions and mortality in patients with heart filuare and central sleep apnea (LOFT-HF). 2019.
Javaheri S. Acetazolamide improves central sleep apnea in heart failure: a double-blind, prospective study. Am J Respir Crit Care Med. 2006;173(2):234–7. https://doi.org/10.1164/rccm.200507-1035OC.
• Schmickl CN, Landry SA, Orr JE, Chin K, Murase K, Verbraecken J, et al. Acetazolamide for OSA and central sleep apnea: a comprehensive systematic review and meta-analysis. Chest. 2020;158(6):2632–45. https://doi.org/10.1016/j.chest.2020.06.078. Systematic Review and Meta-Analysis of acetazolamide demonstrates benefit in CSA. This may be pivotal in increasing use of acetazolamide for CSA.
Javaheri S, Parker TJ, Wexler L, Liming JD, Lindower P, Roselle GA. Effect of theophylline on sleep-disordered breathing in heart failure. N Engl J Med. 1996;335(8):562–7. https://doi.org/10.1056/NEJM199608223350805.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part on the Topical Collection on Nonpharmacologic Therapy: Surgery, Ventricular Assist Devices, Biventricular Pacing, and Exercise
Rights and permissions
About this article
Cite this article
Holfinger, S., Chan, L. & Donald, R. All You Need Is Sleep: the Effects of Sleep Apnea and Treatment Benefits in the Heart Failure Patient. Curr Heart Fail Rep 18, 144–152 (2021). https://doi.org/10.1007/s11897-021-00506-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-021-00506-1