Abstract
Purpose of the Review
Preparative fasting orders arose out of a purported need to enhance imaging studies, reduce interference of food with intended medical/surgical interventions, and protect the patient from vomiting and aspiration pneumonia. This review discusses the frequency, appropriateness, and efficacy of fasting orders in meeting those needs and whether their use should be modified in the future.
Recent Findings
Nil per os (NPO) orders are overused, as they are often inappropriate, typically excessive, and routinely create barriers which may increase risk for patients. Fasting orders are used more often for medical procedures than for surgical operations or imaging studies. One fourth of NPO orders are inappropriate, and the intended procedure or study is canceled 20% of the time usually for a change in plans or scheduling error and rarely because of patient eating. Nausea/vomiting associated with contrast media or imaging studies is rare, self-limited, and not linked to preparatory fluid or food ingestion. Prolonged fasting reduces patient cooperation and satisfaction, and may contribute to a higher rate of complications.
Summary
Each institution should review and revise preparative fasting orders. Drinking of fluids should be allowed without restriction. Truncated periods of solid food restriction may be required due to technical reasons related to specific imaging studies, and for procedures or surgical operations which require sedation or general anesthesia. Inappropriate and prolonged fasting should be avoided, as they create barriers to adequate nutritional therapy and impose added risk with regard to patient outcomes.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Li X, Liu H, Zhao L, Liu J, et al. The effect of preparative solid food status on the occurrence of nausea, vomiting, and aspiration symptoms in enhanced CT examination: prospective observational study. Brit J Radiol. 2018;91:20180198. This key study highlights the impact of prolonged fasting caused by inappropriate NPO orders.
McClave SA, Lowen CC, Martindale RG. The 2016 ESPEN Arvid Wretlind lecture: the gut in stress. Clin Nutr. 2018;37:19–36.
•• Barbosa PN, Bitencourt AG, Tyng CJ, Cunha R, et al. Preparative fasting for contrast-enhanced CT in a cancer center: a new approach. Amer J Radiol. 2018;210:941–7. This large trial shows how symptoms vary minimally between fasting and non-fasting groups prior to a contrast-enhanced CT scan.
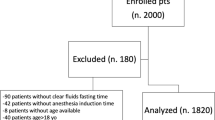
•• Sorita A, Thongprayoon C, Ahmed A, Bates RE, et al. Frequency and appropriateness of fasting orders in the hospital. Mayo Clin Proc. 2015;90(9):1225–32. As one of two trials done by Sorita, this study highlights the duration and appropriateness of NPO orders at an academic US medical center.
•• Neeman Z, Ata MA, Touma E, Saliba W, et al. Is fasting still necessary prior to contrast-enhanced computed tomography? A randomized clinical study. Eur Radiol. 2021;31:1451–9. This important paper reports a randomized controlled trial showing the low frequency of nausea, vomiting, and aspiration with imaging studies.
Lee BY, Ok JJ, Elsayed AA, Kim Y, Han DH. Preparative fasting for contrast-enhanced CT: reconsideration. Radiology. 2012;263(2):444–50.
•• Sorita A, Thongprayoon C, Ratelle JT, Bates RE, et al. Characteristics and outcomes of fasting orders among medical inpatients. J Hosp Pract. 2017;12(1):36–9. This second trial by Sorita shows differences in the indication for NPO orders and whether the intended study or intervention was ultimately completed.
Franklin GA, McClave SA, Lowen CC, Hurt RT, et al. Physician-delivered malnutrition: why do patients remain NPO or on clear liquids in a university hospital setting? JPEN J Parenter Enteral Nutr. 2011;35(3):337–42.
Lamb S, Close A, Bonnin C, Ferrie S. “Nil per mouth” – are we starving our patients? ESPEN. 2010;5(2):e90–2.
Tsushima Y, Seki Y, Nakajima T, Hirasawa H, et al. The effect of abolishing instructions too fast prior to contrast enhanced CT only incidents of acute adverse reactions. Insights Imaging. 2020;11:113–9.
Wagner HJ, Evers JP, Hoppe M, Klose KJ. Must the patient fast before intravascular injection of a non-ionic contrast medium? Results of a controlled study. Rofo. 1997;166(5):370–93.
American Society of Anesthesiologists. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures–a report by the American Society of Anesthesiologists Task Force on preoperative fasting. Anesthesiology. 1999;90:896–905.
Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures an updated report by the American Society of Anesthesiologists Committee on standards and practice parameters. Anesthesiology. 2011;114:495–511.
Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Task Force on preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology. 2017;126:376–93.
McLeod R, Fitzgerald W, Sarr M, et al. Canadian Association of General Surgeons and American College of surgeons evidence based reviews in surgery. Preoperative fasting for adults to prevent perioperative complications. Can J Surg. 2005 Oct;48(5):409–11.
European Society of Urogenital Radiology. ESUR guidelines on contrast media ver. 10.0. http://www.esur.org/fileadmin/content/2019/ESUR_Guidelines_10.0_Final_Version.pdf.
Kim YS, Yoon SH, Choi YH, Park CM, Lee W, Goo JM. Nausea and vomiting after exposure to non-ionic contrast media: incidence and risk factors focusing on preparatory fasting. Br J Radiol. 2018;91:20180107.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Nutrition and Obesity
Rights and permissions
About this article
Cite this article
McClave, S.A., Marsano-Obando, L.S. Preparative Fasting Orders for Medical/Surgical Interventions and Imaging Studies: Time to Review and Revise!. Curr Gastroenterol Rep 24, 37–41 (2022). https://doi.org/10.1007/s11894-022-00841-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11894-022-00841-w