Abstract
Purpose of Review
This article provides an updated review on the role of diet in the risk of developing Crohn’s disease (CD) and CD management, areas of ongoing study.
Recent Findings
Higher intake of dietary fiber (fruit fiber) has been associated with a reduced risk for CD. The exclusive enteral nutrition (EEN) diet remains the most validated nutritional recommendation for inducing remission in CD. The specific carbohydrate diet (SCD) has demonstrated reductions in CD severity scores in conjunction with medical therapies, and larger trials on its efficacy are ongoing. Several new exclusion diets modeled after EEN and SCD have shown potential efficacy in smaller studies that warrant replication. There is a paucity of clear dietary recommendations for the reduction in risk of CD clinical relapse.
Summary
There are various components of diet that likely impact risk for CD development and contribute to its disease course; however, studies are often limited in their size or ability to demonstrate mechanistic causation. Further studies including diets that aim to expand on the restrictive nature of EEN may lead to stronger evidence for a diet-based approach to CD management.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Lichtenstein GR, Loftus EV, Isaacs KL, Regueiro MD, Gerson LB, Sands BE. ACG clinical guideline: management of crohnʼs disease in adults. Am J Gastroenterol. 2018;113(4):481–517.
•• Limketkai BN, Iheozor-Ejiofor Z, Gjuladin-Hellon T, Parian A, Matarese LE, Bracewell K, et al. Dietary interventions for induction and maintenance of remission in inflammatory bowel disease. Cochrane Database Syst Rev. 2019;2:CD012839 Recently updated comprehensive review of RCTs assessing diet interventions for induction or maintenance of remission in people with IBD.
Limdi JK, Aggarwal D, McLaughlin JT. Dietary practices and beliefs in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2016;22:164–70.
Casanova MJ, Chaparro M, Molina B, Merino O, Batanero R, Duenas-Sadornil C, et al. Prevalence of malnutrition and nutritional characteristics of patients with inflammatory bowel disease. J Crohns Colitis. 2017;11:1430–9.
Holt DQ, Strauss BJ, Moore GT. Patients with inflammatory bowel disease and their treating clinicians have different views regarding diet. J Hum Nutr Diet. 2017;30:66–72.
Pfeffer-Gik T, Levine A. Dietary clues to the pathogenesis of Crohn’s disease. Dig Dis. 2014;32:389–94.
Martinez-Medina M, Denizot J, Dreux N, Robin F, Billard E, Bonnet R, et al. Western diet induces dysbiosis with increased e coli in ceabac10 mice, alters host barrier function favouring AIEC colonisation. Gut. 2014;63:116–24.
Agus A, Denizot J, Thévenot J, Martinez-Medina M, Massier S, Sauvanet P, et al. Western diet induces a shift in microbiota composition enhancing susceptibility to Adherent-Invasive E. coli infection and intestinal inflammation. Sci Rep. 2016;6:19032.
Ananthakrishnan AN, Khalili H, Song M, Higuchi LM, Richter JM, Nimptsch K, et al. High school diet and risk of crohn’s disease and ulcerative colitis. Inflamm Bowel Dis. 2015;21:2311–9.
Niewiadomski O, Studd C, Wilson J, Williams J, Hair C, Knight R, et al. Influence of food and lifestyle on the risk of developing inflammatory bowel disease. Intern Med J. 2016;46:669–76. https://doi.org/10.1111/imj.13094.
Chan SS, Luben R, van Schaik F, Oldenburg B, Bueno-de-Mesquita HB, Hallmans G, et al. Carbohydrate intake in the etiology of Crohn’s disease and ulcerative colitis. Inflamm Bowel Dis. 2014;20:2013–21.
Khalili H, Hakansson N, Chan SS, et al. No association between consumption of sweetened beverages and risk of later-onset Crohn's disease or ulcerative colitis. Clin Gastroenterol Hepatol. 2019;17:123–9.
Eswaran S, Muir J, Chey WD. Fiber and functional gastrointestinal disorders. Am J Gastroenterol. 2013;108:718–27.
Zeng L, Hu S, Chen P, et al. Macronutrient intake and risk of Crohn's disease: systematic review and dose-response meta-analysis of epidemiological studies. Nutrients. 2017;9:500.
Li F, Liu X, Wang W, Zhang D. Consumption of vegetables and fruit and the risk of inflammatory bowel disease: a meta-analysis. Eur J Gastroenterol Hepatol. 2015;27:623–30.
Ananthakrishnan AN, Khalili H, Konijeti GG, et al. A prospective study of long-term intake of dietary fiber and risk of Crohn’s disease and ulcerative colitis. Gastroenterology. 2013;145(5):970–7.
Shoda R, Matsueda K, Yamato S, Umeda N. Epidemiologic analysis of Crohn disease in Japan: increased dietary intake of n-6 polyunsaturated fatty acids and animal protein relates to the increased incidence of Crohn disease in Japan. Am J Clin Nutr. 1996;63:741–5.
Ananthakrishnan AN, Khalili H, Konijeti GG, Higuchi LM, de Silva P, Fuchs CS, et al. Long-term intake of dietary fat and risk of ulcerative colitis and Crohn’s disease. Gut. 2014;63:776–84.
Jantchou P, Morois S, Clavel-Chapelon F, Boutron-Ruault MC, Carbonnel F. Animal protein intake and risk of inflammatory bowel disease: the E3N prospective study. Am J Gastroenterol. 2010;105:2195–210.
Opstelten JL, Leenders M, Dik VK, Chan SS, van Schaik FD, Khaw KT, et al. Dairy products, dietary calcium, and risk of inflammatory bowel disease: results from a european prospective cohort investigation. Inflamm Bowel Dis. 2016;22:1403–11.
Roberts CL, Rushworth SL, Richman E, Rhodes JM. Hypothesis: increased consumption of emulsifiers as an explanation for the rising incidence of Crohn's disease. J Crohns Colitis. 2013;7:338–41.
Chassaing B, Koren O, Goodrich JK, Poole AC, Srinivasan S, Ley RE, et al. Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome. Nature. 2015;519:92–6.
Chassaing B, Van de Wiele T, De Bodt J, Marzorati M, Gewirtz AT. Dietary emulsifiers directly alter human microbiota composition and gene expression ex vivo potentiating intestinal inflammation. Gut. 2017;66:1414–27.
Sakamoto N, et al. Dietary risk factors for inflammatory bowel disease: a multicenter case-control study in Japan. Inflamm Bowel Dis. 2005;11:154–63.
Rodriguez-Palacios A, Harding A, Menghini P, Himmelman C, Retuerto M, Nickerson KP, et al. The artificial sweetener splenda promotes gut proteobacteria, dysbiosis, and myeloperoxidase reactivity in Crohn’s disease-like ileitis. Inflamm Bowel Dis. 2018;24:1005–20.
•• Narula N, Dhillon A, Zhang D, Sherlock ME, Tondeur M, Zachos M. Enteral nutritional therapy for induction of remission in Crohn’s disease. Cochrane Database Syst Rev. 2018;4:CD000542 Updated meta-analysis of RCTs comparing EEN to steroids for induction of remission in CD, noting potential differing effects of induction therapies based on age.
•• Cohen-Dolev N, Sladek M, Hussey S, Turner D, Veres G, Koletzko S, et al. Differences in outcomes over time with exclusive enteral nutrition compared with steroids in children with mild to moderate Crohn’s disease: Results from the growth cd study. J Crohn's Colitis. 2018;12:306–12 Large international prospective study showing some evidence for superiority of EEN over steroids as induction for mild-moderate CD in pediatric patients.
Yamamoto T, Nakahigashi M, Umegae S, Matsumoto K. Enteral nutrition for the maintenance of remission in Crohn's disease: a systematic review. Eur J Gastroenterol Hepatol. 2010;22(1):1–8.
Johnson T, Macdonald S, Hill SM, Thomas A, Murphy MS. Treatment of active Crohn's disease in children using partial enteral nutrition with liquid formula: a randomised controlled trial. Gut. 2006;55:356–36.
Lee D, Baldassano RN, Otley AR, Albenberg L, Griffiths AM, Compher C, et al. Comparative effectiveness of nutritional and biological therapy in north American children with active crohn’s disease. Inflamm Bowel Dis. 2015;21:1786–93.
Sigall-Boneh R, Pfeffer-Gik T, Segal I, Zangen T, Boaz M, Levine A. Partial enteral nutrition with a Crohn’s disease exclusion diet is effective for induction of remission in children and young adults with Crohn’s disease. Inflamm Bowel Dis. 2014;20:1353–60.
Sigall BR, Sarbagili SC, Yanai H, Chermesh I, Ben AS, Boaz M, et al. Dietary therapy with the Crohn’s disease exclusion diet is a successful strategy for induction of remission in children and adults failing biological therapy. J Crohn's Colitis. 2017;11:1205–12.
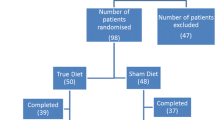
•• Levine A, Wine E, Assa A, et al. Crohn’s disease exclusion diet plus partial enteral nutrition induces sustained remission in a randomized controlled trial. Gastroenterology. 2019;5085(19):36714–9 First RCT comparing oral diet CDED + PEN to standard EEN demonstrating efficacy in inducing remission and improved tolerance with CDED+PEN.
•• Svolos V, Hansen R, Nichols B, Quince C, Ijaz UZ, Papadopoulou RT, et al. Treatment of active crohn’s disease with an ordinary food-based diet that replicates exclusive enteral nutrition. Gastroenterology. 2019;56:1354–67 RCT of tolerability of CD-TREAT, a novel oral diet replicating EEN that will be the subject of ongoing study as a dietary approach for inducing CD remission.
Laudisi F, Di Fusco D, Dinallo V, Stolfi C, Di Grazia A, Marafini I, et al. The food additive maltodextrin promotes endoplasmic reticulum stress-driven mucus depletion and exacerbates intestinal inflammation. Cell Mol Gastroenterol Hepatol. 2019;7:457–73.
Obih C, Wahbeh G, Lee D, Braly K, Giefer M, Shaffer ML, et al. Specific carbohydrate diet for pediatric inflammatory bowel disease in clinical practice within an academic ibd center. Nutrition. 2016;32:418–25.
Cohen SA, Gold BD, Oliva S, Lewis J, Stallworth A, Koch B, et al. Clinical and mucosal improvement with specific carbohydrate diet in pediatric Crohn disease. J Pediatr Gastroenterol Nutr. 2014;59:516–21.
Suskind DL, Cohen SA, Brittnacher MJ, Wahbeh G, Lee D, Shaffer ML, et al. Clinical and fecal microbial changes with diet therapy in active inflammatory bowel disease. J Clin Gastroenterol. 2018;52:155–63.
Suskind DL, Wahbeh G, Gregory N, Vendettuoli H, Christie D. Nutritional therapy in pediatric Crohn disease: the specific carbohydrate diet. J Pediatr Gastroenterol Nutr. 2014;58:87–91.
Wahbeh GT, Ward BT, Lee DY, Giefer MJ, Suskind DL. Lack of mucosal healing from modified specific carbohydrate diet in pediatric patients with Crohn disease. J Pediatr Gastroenterol Nutr. 2017;65(03):289–92.
Eswaran S, Chey WD, Jackson K, Pillai S, Chey SW, Han-Markey T. A diet low in fermentable oligo-, di-, and monosaccharides and polyols improves quality of life and reduces activity impairment in patients with irritable bowel syndrome and diarrhea. Clin Gastroenterol Hepatol. 2017;15:1890–9.
Major G, Pritchard S, Murray K, Alappadan JP, Hoad CL, Marciani L, et al. Colon hypersensitivity to distension, rather than excessive gas production, produces carbohydrate-related symptoms in individuals with irritable bowel syndrome. Gastroenterology. 2017;152:124–33.
Prince AC, Myers CE, Joyce T, Irving P, Lomer M, Whelan K. Fermentable carbohydrate restriction (low FODMAP diet) in clinical practice improves functional gastrointestinal symptoms in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2016;22:1129–36.
Maagaard L, Ankersen DV, Végh Z, Burisch J, Jensen L, Pedersen N, et al. Follow-up of patients with functional bowel symptoms treated with a low FODMAP diet. World J Gastroenterol. 2016;22(15):4009–19.
Pedersen N, Ankersen DV, Felding M, Wachmann H, Vegh Z, Molzen L, et al. Low-FODMAP diet reduces irritable bowel symptoms in patients with inflammatory bowel disease. World J Gastroenterol. 2017;23:3356–66.
Zhan YL, Zhan YA, Dai SX. Is a low FODMAP diet beneficial for patients with inflammatory bowel disease? A meta-analysis and systematic review. Clin Nutr. 2018;37:123–9.
Herfarth HH, Martin CF, Sandler RS, Kappelman MD, Long MD. Prevalence of a gluten-free diet and improvement of clinical symptoms in patients with inflammatory bowel diseases. Inflamm Bowel Dis. 2014;20:1194–7.
Schreiner P, Yilmaz B, Rossel J-B, Franc Y, Misselwitz B, Scharl M, et al. Vegetarian or gluten-free diets in patients with inflammatory bowel disease are associated with lower psychological well-being and a different gut microbiota, but no beneficial effects on the course of the disease. United European Gastroenterol J. 2019;7(6):767–81.
Konijeti GG, Kim N, Lewis JD, et al. Efficacy of the autoimmune protocol diet for inflammatory bowel disease. Inflamm Bowel Dis. 2017;23:2054–60.
Hung TV, Suzuki T. Dietary fermentable fiber reduces intestinal barrier defects and inflammation in colitic mice. J Nutr. 2016;146:1970–9.
Wang H, Shi P, Zuo L, Dong J, Zhao J, Liu Q, et al. Dietary non-digestible polysaccharides ameliorate intestinal epithelial barrier dysfunction in il-10 knockout mice. J Crohn's Colitis. 2016;10:1076–86.
Silveira ALM, Ferreira AVM, de Oliveira MC, Rachid MA, da Cunha Sousa LF, Dos Santos Martins F, et al. Preventive rather than therapeutic treatment with high fiber diet attenuates clinical and inflammatory markers of acute and chronic dss-induced colitis in mice. Eur J Nutr. 2017;56:179–91.
Wedlake L, Slack N, Andreyev HJ, Whelan K. Fiber in the treatment and maintenance of inflammatory bowel disease: a systematic review of randomized controlled trials. Inflamm Bowel Dis. 2014;20:576–86.
Brotherton CS, Martin CA, Long MD, Kappelman MD, Sandler RS. Avoidance of fiber is associated with greater risk of Crohn’s disease flare in a 6-month period. Clin Gastroenterol Hepatol. 2016;14(08):1130–6.
•• Akobeng AK, Zhang D, Gordon M, MacDonald JK. Enteral nutrition for maintenance of remission in Crohn’s disease. Cochrane Database Syst Rev. 2018:CD005984 Comprehensive updated review of RCTs assessing efficacy of EEN in maintaining CD remission.
Sugita N, Watanabe K, Kamata N, Yukawa T, Otani K, Hosomi S, et al. Efficacy of a concomitant elemental diet to reduce the loss of response to adalimumab in patients with intractable Crohn's disease. J Gastroenterol Hepatol. 2018;33:631–7.
Kamata N, Oshitani N, Watanabe K, Watanabe K, Hosomi S, Noguchi A, et al. Efficacy of concomitant elemental diet therapy in scheduled infliximab therapy in patients with Crohn’s disease to prevent loss of response. Dig Dis Sci. 2015;60:1382–8.
Chiba M, Abe T, Tsuda H, Sugawara T, Tsuda S, Tozawa H, et al. Lifestyle-related disease in Crohn’s disease: relapse prevention by a semi-vegetarian diet. World J Gastroenterol. 2010;16:2484–95.
•• Albenberg L, Brensinger CM, Wu Q, Gilroy E, Kappelman MD, Sandler RS, et al. A diet low in red and processed meat does not reduce rate of crohn’s disease flares. Gastroenterology. 2019;157:128–36 RCT of impact of impact of low and high red/processed meat intake on CD relapse rates uniquely conducted with use of Internet-based cohort and online materials.
Narula N, Cooray M, Anglin R, Muqtadir Z, Narula A, Marshall JK. Impact of high-dose vitamin d3 supplementation in patients with Crohn’s disease in remission: a pilot randomized double-blind controlled study. Dig Dis Sci. 2017;62:448–55.
Sadeghian M, Saneei P, Siassi F, Esmaillzadeh A. Vitamin D status in relation to Crohn’s disease: meta-analysis of observational studies. Nutrition. 2016;32:505–14.
Ananthakrishnan AN, Cagan A, Gainer VS, Cheng S-C, Cai T, Szolovits P, et al. Higher plasma vitamin D is associated with reduced risk of Clostridium difficile infection in patients with inflammatory bowel diseases. Aliment Pharmacol Ther. 2014;39:1136–42.
Ananthakrishnan AN, Cheng SC, Cai T, Cagan A, Gainer VS, Szolovits P, et al. Association between reduced plasma 25-hydroxy vitamin D and increased risk of cancer in patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2014;12:821–7.
Jørgensen S, Agnholt J, Glerup H. Clinical trial: vitamin D3 treatment in Crohn’s disease—a randomized double-blind placebo-controlled study. Aliment Pharmacol Ther. 2010;32:377–83.
Lev-Tzion R, Griffiths AM, Leder O, Turner D. Omega 3 fatty acids (fish oil) for maintenance of remission in Crohn’s disease. Cochrane Database Syst Rev. 2014:CD006320.
Feagan BG, Sandborn WJ, Mittmann U, Bar-Meir S, D'Haens G, Bradette M, et al. Omega-3 free fatty acids for the maintenance of remission in Crohn disease. The EPIC randomized controlled trials. JAMA. 2008;299:1690–7.
Lang A, Salomon N, Wu JC, Kopylov U, Lahat A, Har-Noy O, et al. Curcumin in combination with mesalamine induces remission in patients with mild-to-moderate ulcerative colitis in a randomized controlled trial. Clin Gastroenterol Hepatol. 2015;13:1444–9.
Bommelaer G, Laharie D, Nancey S, Hebuterne X, Roblin X, Nachury M, et al. Oral Curcumin No More Effective Than Placebo in Preventing Recurrence of Crohn's Disease After Surgery in a Randomized Controlled Trial. Clin Gastroenterol Hepatol. 2019.
Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, et al. Expert consensus document. The international scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11(8):506–14.
Khanna S, Raffals LE. The microbiome in Crohn's disease: role in pathogenesis and role of microbiome replacement therapies. Gastroenterol Clin N Am. 2017;46:481–92.
Shen J, Zuo ZX, Mao AP. Effect of probiotics on inducing remission and maintaining therapy in ulcerative colitis, Crohn’s disease, and pouchitis: meta-analysis of randomized controlled trials. Inflamm Bowel Dis. 2014;20:21–35.
Ghouri YA, Richards DM, Rahimi EF, Krill JT, Jelinek KA, DuPont A. Systematic review of randomized controlled trials of probiotics, prebiotics, and synbiotics in inflammatory bowel disease. Clin Exp Gastroenterol. 2014;7:473–87.
Abraham BP, Quigley EM. Probiotics in inflammatory bowel disease. Gastroenterol Clin N Am. 2017;46:769–82.
•• Sigall-Boneh R, Levine A, Lomer M, Wierdsma N, Allan P, Fiorino G, et al. Research gaps in diet and nutrition in inflammatory bowel disease. A topical review by D-ECCO working group [Dietitians of ECCO]. J Crohns Colitis. 2017;11:1407–19 Comprehensive review from nutrition experts on nutrition and IBD with important discussion on remaining gaps in research and potential future directions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Grant Support
None.
Disclosures
None expressed.
Conflict of Interest
None with respect to the submitted work.
Writing Assistance
No support provided.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Small Intestine
Rights and permissions
About this article
Cite this article
Goens, D., Micic, D. Role of Diet in the Development and Management of Crohn’s Disease. Curr Gastroenterol Rep 22, 19 (2020). https://doi.org/10.1007/s11894-020-0755-9
Published:
DOI: https://doi.org/10.1007/s11894-020-0755-9