Abstract
Purpose of Review
Gastroparesis remains a difficult-to-treat disease with limited therapeutic options. Though patients often have a common syndrome of stereotypic symptoms, the underlying pathophysiology is heterogeneous, often leading to variable treatment responses. Due to limitations in medical and surgical therapies, endoscopic options have been increasingly explored. These options can be broadly categorized into pyloric-directed therapy, non-pyloric-directed therapy, and nutritional support. In this review, we will highlight current and emerging endoscopic options, such as gastric per-oral endoscopic myotomy (G-POEM).
Recent Findings
Early retrospective studies on G-POEM offer encouraging results up to one year out, with an acceptable safety profile. Other pyloric-directed therapies, such as pyloric dilation and stenting, have also been explored.
Summary
While emerging endoscopic therapeutic options are encouraging, efficacy will likely depend on a better characterization of underlying pathophysiology and improved patient selection. Future prospective, controlled studies are needed.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Wang YR, Fisher RS, Parkman HP. Gastroparesis-related hospitalizations in the United States: trends, characteristics, and outcomes, 1995–2004. Am J Gastroenterol. 2008;103(2):313–22. https://doi.org/10.1111/j.1572-0241.2007.01658.x.
Wadhwa V, Mehta D, Jobanputra Y, Lopez R, Thota PN, Sanaka MR. Healthcare utilization and costs associated with gastroparesis. World J Gastroenterol. 2017;23(24):4428–36. https://doi.org/10.3748/wjg.v23.i24.4428.
Lacy BE, Crowell MD, Mathis C, Bauer D, Heinberg LJ. Gastroparesis: quality of life and health care utilization. J Clin Gastroenterol. 2018;52(1):20–4. https://doi.org/10.1097/MCG.0000000000000728.
Parkman HP, McCallum RW. Gastroparesis: pathophysiology, presentation and treatment. 2012.
Kashyap P, Farrugia G. Diabetic gastroparesis: what we have learned and had to unlearn in the past 5 years. Gut. 2010;59(12):1716–26. https://doi.org/10.1136/gut.2009.199703.
Feldman M, Friedman LS, Brandt LJ. Sleisenger and Fordtran’s gastrointestinal and liver disease: pathophysiology/diagnosis/management. 2016.
Sarnelli G, Caenepeel P, Geypens B, Janssens J, Tack J. Symptoms associated with impaired gastric emptying of solids and liquids in functional dyspepsia. Am J Gastroenterol. 2003;98(4):783–8. https://doi.org/10.1111/j.1572-0241.2003.07389.x.
Parkman HP, Camilleri M, Farrugia G, McCallum RW, Bharucha AE, Mayer EA, et al. Gastroparesis and functional dyspepsia: excerpts from the AGA/ANMS meeting. Neurogastroenterol Motil. 2010;22(2):113–33. https://doi.org/10.1111/j.1365-2982.2009.01434.x.
Talley NJ, Ford AC. Functional dyspepsia. N Engl J Med. 2015;373(19):1853–63. https://doi.org/10.1056/NEJMra1501505.
Pasricha PJ, Yates KP, Nguyen L, Clarke J, Abell TL, Farrugia G, et al. Outcomes and factors associated with reduced symptoms in patients with gastroparesis. Gastroenterology. 2015;149(7):1762–1774 e4. https://doi.org/10.1053/j.gastro.2015.08.008.
Olausson EA, Storsrud S, Grundin H, Isaksson M, Attvall S, Simren M. A small particle size diet reduces upper gastrointestinal symptoms in patients with diabetic gastroparesis: a randomized controlled trial. Am J Gastroenterol. 2014;109(3):375–85. https://doi.org/10.1038/ajg.2013.453.
Wytiaz V, Homko C, Duffy F, Schey R, Parkman HP. Foods provoking and alleviating symptoms in gastroparesis: patient experiences. Dig Dis Sci. 2015;60(4):1052–8. https://doi.org/10.1007/s10620-015-3651-7.
Homko CJ, Duffy F, Friedenberg FK, Boden G, Parkman HP. Effect of dietary fat and food consistency on gastroparesis symptoms in patients with gastroparesis. Neurogastroenterol Motil. 2015;27(4):501–8. https://doi.org/10.1111/nmo.12519.
Parkman HP, Yates KP, Hasler WL, Nguyan L, Pasricha PJ, Snape WJ, et al. Dietary intake and nutritional deficiencies in patients with diabetic or idiopathic gastroparesis. Gastroenterology. 2011;141(2):486–98, 98 e1–7. https://doi.org/10.1053/j.gastro.2011.04.045.
Camilleri M, Parkman HP, Shafi MA, Abell TL, Gerson L, American College of G. Clinical guideline: management of gastroparesis. Am J Gastroenterol. 2013;108(1):18–37; quiz 8. https://doi.org/10.1038/ajg.2012.373.
Lata PF, Pigarelli DL. Chronic metoclopramide therapy for diabetic gastroparesis. Ann Pharmacother. 2003;37(1):122–6. https://doi.org/10.1345/aph.1C118.
Rao AS, Camilleri M. Review article: metoclopramide and tardive dyskinesia. Aliment Pharmacol Ther. 2010;31(1):11–9. https://doi.org/10.1111/j.1365-2036.2009.04189.x.
Schey R, Saadi M, Midani D, Roberts AC, Parupalli R, Parkman HP. Domperidone to treat symptoms of gastroparesis: benefits and side effects from a large single-center cohort. Dig Dis Sci. 2016;61(12):3545–51. https://doi.org/10.1007/s10620-016-4272-5.
Heckert J, Parkman HP. Therapeutic response to domperidone in gastroparesis: a prospective study using the GCSI-daily diary. Neurogastroenterol Motil. 2018;30(1) https://doi.org/10.1111/nmo.13246.
Buffery PJ, Strother RM. Domperidone safety: a mini-review of the science of QT prolongation and clinical implications of recent global regulatory recommendations. N Z Med J. 2015;128(1416):66–74.
Ortiz A, Cooper CJ, Alvarez A, Gomez Y, Sarosiek I, McCallum RW. Cardiovascular safety profile and clinical experience with high-dose domperidone therapy for nausea and vomiting. Am J Med Sci. 2015;349(5):421–4. https://doi.org/10.1097/MAJ.0000000000000439.
Richards RD, Davenport K, McCallum RW. The treatment of idiopathic and diabetic gastroparesis with acute intravenous and chronic oral erythromycin. Am J Gastroenterol. 1993;88(2):203–7.
Guo D, Cai Y, Chai D, Liang B, Bai N, Wang R. The cardiotoxicity of macrolides: a systematic review. Pharmazie. 2010;65(9):631–40.
Fan LC, Lu HW, Wei P, Ji XB, Liang S, Xu JF. Effects of long-term use of macrolides in patients with non-cystic fibrosis bronchiectasis: a meta-analysis of randomized controlled trials. BMC Infect Dis. 2015;15:160. https://doi.org/10.1186/s12879-015-0872-5.
Larson JM, Tavakkoli A, Drane WE, Toskes PP, Moshiree B. Advantages of azithromycin over erythromycin in improving the gastric emptying half-time in adult patients with gastroparesis. J Neurogastroenterol Motil. 2010;16(4):407–13. https://doi.org/10.5056/jnm.2010.16.4.407.
Pasricha PJ, Yates KP, Sarosiek I, McCallum RW, Abell TL, Koch KL, et al. Aprepitant has mixed effects on nausea and reduces other symptoms in patients with gastroparesis and related disorders. Gastroenterology. 2018;154(1):65–76 e11. https://doi.org/10.1053/j.gastro.2017.08.033.
Hellstrom PM, Tack J, Johnson LV, Hacquoil K, Barton ME, Richards DB, et al. The pharmacodynamics, safety and pharmacokinetics of single doses of the motilin agonist, camicinal, in type 1 diabetes mellitus with slow gastric emptying. Br J Pharmacol. 2016;173(11):1768–77. https://doi.org/10.1111/bph.13475.
Manini ML, Camilleri M, Goldberg M, Sweetser S, McKinzie S, Burton D, et al. Effects of Velusetrag (TD-5108) on gastrointestinal transit and bowel function in health and pharmacokinetics in health and constipation. Neurogastroenterol Motil. 2010;22(1):42–9, e7–8. https://doi.org/10.1111/j.1365-2982.2009.01378.x.
Camilleri M, McCallum RW, Tack J, Spence SC, Gottesdiener K, Fiedorek FT. Efficacy and safety of Relamorelin in diabetics with symptoms of gastroparesis: a randomized, placebo-controlled study. Gastroenterology. 2017;153(5):1240–50 e2. https://doi.org/10.1053/j.gastro.2017.07.035.
Omer A, Quigley EMM. An update on prucalopride in the treatment of chronic constipation. Therap Adv Gastroenterol. 2017;10(11):877–87. https://doi.org/10.1177/1756283X17734809.
Sarosiek I, Bashashati M, McCallum RW. Safety of treatment for gastroparesis. Expert Opin Drug Saf. 2016;15(7):937–45. https://doi.org/10.1517/14740338.2016.1173204.
Bouras EP, Camilleri M, Burton DD, Thomforde G, McKinzie S, Zinsmeister AR. Prucalopride accelerates gastrointestinal and colonic transit in patients with constipation without a rectal evacuation disorder. Gastroenterology. 2001;120(2):354–60.
Kessing BF, Smout AJ, Bennink RJ, Kraaijpoel N, Oors JM, Bredenoord AJ. Prucalopride decreases esophageal acid exposure and accelerates gastric emptying in healthy subjects. Neurogastroenterol Motil. 2014;26(8):1079–86. https://doi.org/10.1111/nmo.12359.
Carbone F, Rotondo A, Andrews CN, Holvoet L, Van Oudenhove L, Vanuytsel T, et al. 1077 a controlled cross-over trial shows benefit of Prucalopride for symptom control and gastric emptying enhancement in idiopathic gastroparesis. Gastroenterology. 2015;150(4):S213–S4. https://doi.org/10.1016/S0016-5085(16)30792-2.
Vigone B, Caronni M, Severino A, Bellocchi C, Baldassarri AR, Fraquelli M, et al. Preliminary safety and efficacy profile of prucalopride in the treatment of systemic sclerosis (SSc)-related intestinal involvement: results from the open label cross-over PROGASS study. Arthritis Res Ther. 2017;19(1):145. https://doi.org/10.1186/s13075-017-1340-y.
Dragstedt LR. Vagotomy for gastroduodenal ulcer. Ann Surg. 1945;122:973–89.
Kim DK, Hindenburg AA, Sharma SK, Suk CH, Gress FG, Staszewski H, et al. Is pylorospasm a cause of delayed gastric emptying after pylorus-preserving pancreaticoduodenectomy? Ann Surg Oncol. 2005;12(3):222–7. https://doi.org/10.1245/ASO.2005.03.078.
Ejskjaer NT, Bradley JL, Buxton-Thomas MS, Edmonds ME, Howard ER, Purewal T, et al. Novel surgical treatment and gastric pathology in diabetic gastroparesis. Diabet Med. 1999;16(6):488–95.
Watkins PJ, Buxton-Thomas MS, Howard ER. Long-term outcome after gastrectomy for intractable diabetic gastroparesis. Diabet Med. 2003;20(1):58–63.
Bhayani NH, Sharata AM, Dunst CM, Kurian AA, Reavis KM, Swanstrom LL. End of the road for a dysfunctional end organ: laparoscopic gastrectomy for refractory gastroparesis. J Gastrointest Surg. 2015;19(3):411–7. https://doi.org/10.1007/s11605-014-2609-y.
Zehetner J, Ravari F, Ayazi S, Skibba A, Darehzereshki A, Pelipad D, et al. Minimally invasive surgical approach for the treatment of gastroparesis. Surg Endosc. 2013;27(1):61–6. https://doi.org/10.1007/s00464-012-2407-0.
Jones MP, Maganti K. A systematic review of surgical therapy for gastroparesis. Am J Gastroenterol. 2003;98(10):2122–9. https://doi.org/10.1111/j.1572-0241.2003.07721.x.
Hibbard ML, Dunst CM, Swanstrom LL. Laparoscopic and endoscopic pyloroplasty for gastroparesis results in sustained symptom improvement. J Gastrointest Surg. 2011;15(9):1513–9. https://doi.org/10.1007/s11605-011-1607-6.
Mancini SA, Angelo JL, Peckler Z, Philp FH, Farah KF. Pyloroplasty for refractory gastroparesis. Am Surg. 2015;81(7):738–46.
Toro JP, Lytle NW, Patel AD, Davis SS Jr, Christie JA, Waring JP, et al. Efficacy of laparoscopic pyloroplasty for the treatment of gastroparesis. J Am Coll Surg. 2014;218(4):652–60. https://doi.org/10.1016/j.jamcollsurg.2013.12.024.
Sarosiek I, Forster J, Lin Z, Cherry S, Sarosiek J, McCallum R. The addition of pyloroplasty as a new surgical approach to enhance effectiveness of gastric electrical stimulation therapy in patients with gastroparesis. Neurogastroenterol Motil. 2013;25(2):134–e80. https://doi.org/10.1111/nmo.12032.
• Shada AL, Dunst CM, Pescarus R, Speer EA, Cassera M, Reavis KM, et al. Laparoscopic pyloroplasty is a safe and effective first-line surgical therapy for refractory gastroparesis. Surg Endosc. 2016;30(4):1326–32. https://doi.org/10.1007/s00464-015-4385-5. The largest study to date looking at laparoscopic pyloroplasty in gastroparesis. Showed a mean composite symptom severity score improvement at one month and six months post-operatively
Humanitarian device exemption for Enterra device. Federal Registry. p. 78495–78496.
Lal N, Livemore S, Dunne D, Khan I. Gastric electrical stimulation with the Enterra system: a systematic review. Gastroenterol Res Pract. 2015;2015:762972. https://doi.org/10.1155/2015/762972.
Abell T, McCallum R, Hocking M, Koch K, Abrahamsson H, Leblanc I, et al. Gastric electrical stimulation for medically refractory gastroparesis. Gastroenterology. 2003;125(2):421–8.
McCallum RW, Snape W, Brody F, Wo J, Parkman HP, Nowak T. Gastric electrical stimulation with Enterra therapy improves symptoms from diabetic gastroparesis in a prospective study. Clin Gastroenterol Hepatol. 2010;8(11):947–54; quiz e116. https://doi.org/10.1016/j.cgh.2010.05.020.
McCallum RW, Sarosiek I, Parkman HP, Snape W, Brody F, Wo J, et al. Gastric electrical stimulation with Enterra therapy improves symptoms of idiopathic gastroparesis. Neurogastroenterol Motil. 2013;25(10):815–e636. https://doi.org/10.1111/nmo.12185.
Maranki JL, Lytes V, Meilahn JE, Harbison S, Friedenberg FK, Fisher RS, et al. Predictive factors for clinical improvement with Enterra gastric electric stimulation treatment for refractory gastroparesis. Dig Dis Sci. 2008;53(8):2072–8. https://doi.org/10.1007/s10620-007-0124-7.
Musunuru S, Beverstein G, Gould J. Preoperative predictors of significant symptomatic response after 1 year of gastric electrical stimulation for gastroparesis. World J Surg. 2010;34(8):1853–8. https://doi.org/10.1007/s00268-010-0586-1.
Clarke JO, Snape WJ Jr. Pyloric sphincter therapy: botulinum toxin, stents, and pyloromyotomy. Gastroenterol Clin North Am. 2015;44(1):127–36. https://doi.org/10.1016/j.gtc.2014.11.010.
Mearin F, Camilleri M, Malagelada JR. Pyloric dysfunction in diabetics with recurrent nausea and vomiting. Gastroenterology. 1986;90(6):1919–25.
Desipio J, Friedenberg FK, Korimilli A, Richter JE, Parkman HP, Fisher RS. High-resolution solid-state manometry of the antropyloroduodenal region. Neurogastroenterol Motil. 2007;19(3):188–95. https://doi.org/10.1111/j.1365-2982.2006.00866.x.
Hirano I, Pandolfino JE, Boeckxstaens GE. Functional lumen imaging probe for the management of esophageal disorders: expert review from the clinical practice updates committee of the AGA Institute. Clin Gastroenterol Hepatol. 2017;15(3):325–34. https://doi.org/10.1016/j.cgh.2016.10.022.
• Gourcerol G, Tissier F, Melchior C, Touchais JY, Huet E, Prevost G, et al. Impaired fasting pyloric compliance in gastroparesis and the therapeutic response to pyloric dilatation. Aliment Pharmacol Ther. 2015;41(4):360–7. https://doi.org/10.1111/apt.13053. This is an interesting study for two reasons, the first being its ability to identify the pylorus as a high-pressure zone using EndoFLIP with decreased fasting pyloric compliance in gastroparesis patients. The second was their use of empiric pyloric balloon dilation showing symptom and QOL improvement 10 days afterwards.
• Snape WJ, Lin MS, Agarwal N, Shaw RE. Evaluation of the pylorus with concurrent intraluminal pressure and EndoFLIP in patients with nausea and vomiting. Neurogastroenterol Motil. 2016;28(5):758–64. https://doi.org/10.1111/nmo.12772. This is a more recent study showing a significant decrease in pyloric compliance in patients with nausea, vomiting, and delayed gastric emptying.
• Malik Z, Sankineni A, Parkman HP. Assessing pyloric sphincter pathophysiology using EndoFLIP in patients with gastroparesis. Neurogastroenterol Motil. 2015;27(4):524–31. https://doi.org/10.1111/nmo.12522. This study performed EndoFLIP in 54 gastroparesis patients showing an ability to identify the pylorus with an inverse correlation between certain metrics (diameter and cross-sectional area) and symptoms of early satiety.
Wiesel PH, Schneider R, Dorta G, Blum AL, Gillet M, Michetti P. Botulinum toxin for refractory postoperative pyloric spasm. Endoscopy. 1997;29(2):132. https://doi.org/10.1055/s-2007-1004091.
Miller LS, Szych GA, Kantor SB, Bromer MQ, Knight LC, Maurer AH, et al. Treatment of idiopathic gastroparesis with injection of botulinum toxin into the pyloric sphincter muscle. Am J Gastroenterol. 2002;97(7):1653–60. https://doi.org/10.1111/j.1572-0241.2002.05823.x.
Lacy BE, Zayat EN, Crowell MD, Schuster MM. Botulinum toxin for the treatment of gastroparesis: a preliminary report. Am J Gastroenterol. 2002;97(6):1548–52. https://doi.org/10.1111/j.1572-0241.2002.05741.x.
Arts J, van Gool S, Caenepeel P, Verbeke K, Janssens J, Tack J. Influence of intrapyloric botulinum toxin injection on gastric emptying and meal-related symptoms in gastroparesis patients. Aliment Pharmacol Ther. 2006;24(4):661–7. https://doi.org/10.1111/j.1365-2036.2006.03019.x.
Bromer MQ, Friedenberg F, Miller LS, Fisher RS, Swartz K, Parkman HP. Endoscopic pyloric injection of botulinum toxin A for the treatment of refractory gastroparesis. Gastrointest Endosc. 2005;61(7):833–9.
Gupta P, Rao SS. Attenuation of isolated pyloric pressure waves in gastroparesis in response to botulinum toxin injection: a case report. Gastrointest Endosc. 2002;56(5):770–2. https://doi.org/10.1067/mge.2002.129213.
Arts J, Holvoet L, Caenepeel P, Bisschops R, Sifrim D, Verbeke K, et al. Clinical trial: a randomized-controlled crossover study of intrapyloric injection of botulinum toxin in gastroparesis. Aliment Pharmacol Ther. 2007;26(9):1251–8. https://doi.org/10.1111/j.1365-2036.2007.03467.x.
Friedenberg FK, Palit A, Parkman HP, Hanlon A, Nelson DB. Botulinum toxin A for the treatment of delayed gastric emptying. Am J Gastroenterol. 2008;103(2):416–23. https://doi.org/10.1111/j.1572-0241.2007.01676.x.
Coleski R, Anderson MA, Hasler WL. Factors associated with symptom response to pyloric injection of botulinum toxin in a large series of gastroparesis patients. Dig Dis Sci. 2009;54(12):2634–42. https://doi.org/10.1007/s10620-008-0660-9.
• Wellington J, Scott B, Kundu S, Stuart P, Koch KL. Effect of endoscopic pyloric therapies for patients with nausea and vomiting and functional obstructive gastroparesis. Auton Neurosci. 2017;202:56–61. https://doi.org/10.1016/j.autneu.2016.07.004. A prospective evaluation on patients with proven normal gastromyoelectrical activity on electrogastrography. They hypothesized that these patients were likely to have pylorospasm as the underlying pathophysiology and showed 78% with symptom improvement after intrapyloric BT injections.
Clarke JO, Sharaiha RZ, Kord Valeshabad A, Lee LA, Kalloo AN, Khashab MA. Through-the-scope transpyloric stent placement improves symptoms and gastric emptying in patients with gastroparesis. Endoscopy. 2013;45(Suppl 2 UCTN):E189–90. https://doi.org/10.1055/s-0032-1326400.
Khashab MA, Besharati S, Ngamruengphong S, Kumbhari V, El Zein M, Stein EM, et al. Refractory gastroparesis can be successfully managed with endoscopic transpyloric stent placement and fixation (with video). Gastrointest Endosc. 2015;82(6):1106–9. https://doi.org/10.1016/j.gie.2015.06.051.
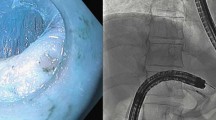
Khashab MA, Stein E, Clarke JO, Saxena P, Kumbhari V, Chander Roland B, et al. Gastric peroral endoscopic myotomy for refractory gastroparesis: first human endoscopic pyloromyotomy (with video). Gastrointest Endosc. 2013;78(5):764–8. https://doi.org/10.1016/j.gie.2013.07.019.
Chaves DM, de Moura EG, Mestieri LH, Artifon EL, Sakai P. Endoscopic pyloromyotomy via a gastric submucosal tunnel dissection for the treatment of gastroparesis after surgical vagal lesion. Gastrointest Endosc. 2014;80(1):164. https://doi.org/10.1016/j.gie.2014.03.045.
Chung H, Dallemagne B, Perretta S, Lee SK, Shin SK, Park JC, et al. Endoscopic pyloromyotomy for postesophagectomy gastric outlet obstruction. Endoscopy. 2014;46(Suppl 1 UCTN):E345–6. https://doi.org/10.1055/s-0034-1377599.
Gonzalez JM, Vanbiervliet G, Vitton V, Benezech A, Lestelle V, Grimaud JC, et al. First European human gastric peroral endoscopic myotomy, for treatment of refractory gastroparesis. Endoscopy. 2015;47(Suppl 1 UCTN):E135–6. https://doi.org/10.1055/s-0034-1391821.
Shlomovitz E, Pescarus R, Cassera MA, Sharata AM, Reavis KM, Dunst CM, et al. Early human experience with per-oral endoscopic pyloromyotomy (POP). Surg Endosc. 2015;29(3):543–51. https://doi.org/10.1007/s00464-014-3720-6.
Mekaroonkamol P, Li LY, Dacha S, Xu Y, Keilin SD, Willingham FF, et al. Gastric peroral endoscopic pyloromyotomy (G-POEM) as a salvage therapy for refractory gastroparesis: a case series of different subtypes. Neurogastroenterol Motil. 2016;28(8):1272–7. https://doi.org/10.1111/nmo.12854.
Gonzalez JM, Lestelle V, Benezech A, Cohen J, Vitton V, Grimaud JC, et al. Gastric per-oral endoscopic myotomy with antropyloromyotomy in the treatment of refractory gastroparesis: clinical experience with follow-up and scintigraphic evaluation (with video). Gastrointest Endosc. 2017;85(1):132–9. https://doi.org/10.1016/j.gie.2016.07.050.
• Dacha S, Mekaroonkamol P, Li L, Shahnavaz N, Sakaria S, Keilin S, et al. Outcomes and quality-of-life assessment after gastric per-oral endoscopic pyloromyotomy (with video). Gastrointest Endosc. 2017;86(2):282–9. https://doi.org/10.1016/j.gie.2017.01.031. Single-center study providing the longest term outcomes in GPOEM. Results from 16 patients showed 81% of patients with significant improvements in mean GCSI scores at 1 month. At 12 months, the 6 patients with follow-up continued to have improved mean GCSI scores.
• Khashab MA, Ngamruengphong S, Carr-Locke D, Bapaye A, Benias PC, Serouya S, et al. Gastric per-oral endoscopic myotomy for refractory gastroparesis: results from the first multicenter study on endoscopic pyloromyotomy (with video). Gastrointest Endosc. 2017;85(1):123–8. https://doi.org/10.1016/j.gie.2016.06.048. A multicenter study involving 30 refractory gastroparesis patients (11 diabetic, 12 post-surgical, 7 idiopathic) who underwent G-POEM. Clinical response was seen in 86% of patients with a median follow-up of 5.5 months.
• Rodriguez JH, Haskins IN, Strong AT, Plescia RL, Allemang MT, Butler RS, et al. Per oral endoscopic pyloromyotomy for refractory gastroparesis: initial results from a single institution. Surg Endosc. 2017;31(12):5381–8. https://doi.org/10.1007/s00464-017-5619-5. Single-center experience with G-POEM in 47 patients using a validated outcome measure, GCSI, and showing a mean improvement in scores from 4.6 to 3.3 at 3 months.
• Gonzalez JM, Benezech A, Vitton V, Barthet M. G-POEM with antro-pyloromyotomy for the treatment of refractory gastroparesis: mid-term follow-up and factors predicting outcome. Aliment Pharmacol Ther. 2017;46(3):364–70. https://doi.org/10.1111/apt.14132. Single-center experience with G-POEM in 29 patients showing a clinical success rate of 79% at 3 months and 69% at 6 months with significant reductions in GCSI (3.3 pre-operatively, 1.0 at 3 months, 1.1 at 6 months). Diabetic gastroparesis and female gender were predictive of failure.
Janssen P, Harris MS, Jones M, Masaoka T, Farre R, Tornblom H, et al. The relation between symptom improvement and gastric emptying in the treatment of diabetic and idiopathic gastroparesis. Am J Gastroenterol. 2013;108(9):1382–91. https://doi.org/10.1038/ajg.2013.118.
Herman LL, Hoskins WJ, Shike M. Percutaneous endoscopic gastrostomy for decompression of the stomach and small bowel. Gastrointest Endosc. 1992;38(3):314–8.
Laval G, Arvieux C, Stefani L, Villard ML, Mestrallet JP, Cardin N. Protocol for the treatment of malignant inoperable bowel obstruction: a prospective study of 80 cases at Grenoble University Hospital Center. J Pain Symptom Manag. 2006;31(6):502–12. https://doi.org/10.1016/j.jpainsymman.2005.10.009.
Committee ASoP, Fukami N, Anderson MA, Khan K, Harrison ME, Appalaneni V, et al. The role of endoscopy in gastroduodenal obstruction and gastroparesis. Gastrointest Endosc. 2011;74(1):13–21. https://doi.org/10.1016/j.gie.2010.12.003.
Pitt HA, Mann LL, Berquist WE, Ament ME, Fonkalsrud EW, DenBesten L. Chronic intestinal pseudo-obstruction. Management with total parenteral nutrition and a venting enterostomy. Arch Surg. 1985;120(5):614–8.
Murr MM, Sarr MG, Camilleri M. The surgeon’s role in the treatment of chronic intestinal pseudoobstruction. Am J Gastroenterol. 1995;90(12):2147–51.
Kim CH, Nelson DK. Venting percutaneous gastrostomy in the treatment of refractory idiopathic gastroparesis. Gastrointest Endosc. 1998;47(1):67–70.
Bankhead RR, Fisher CA, Rolandelli RH. Gastrostomy tube placement outcomes: comparison of surgical, endoscopic, and laparoscopic methods. Nutr Clin Pract. 2005;20(6):607–12. https://doi.org/10.1177/0115426505020006607.
Ljungdahl M, Sundbom M. Complication rate lower after percutaneous endoscopic gastrostomy than after surgical gastrostomy: a prospective, randomized trial. Surg Endosc. 2006;20(8):1248–51. https://doi.org/10.1007/s00464-005-0757-6.
Silas AM, Pearce LF, Lestina LS, Grove MR, Tosteson A, Manganiello WD, et al. Percutaneous radiologic gastrostomy versus percutaneous endoscopic gastrostomy: a comparison of indications, complications and outcomes in 370 patients. Eur J Radiol. 2005;56(1):84–90. https://doi.org/10.1016/j.ejrad.2005.02.007.
Committee AT, Kwon RS, Banerjee S, Desilets D, Diehl DL, Farraye FA, et al. Enteral nutrition access devices. Gastrointest Endosc. 2010;72(2):236–48. https://doi.org/10.1016/j.gie.2010.02.008.
Committee AT, Enestvedt BK, Jorgensen J, Sedlack RE, Coyle WJ, Obstein KL, et al. Endoscopic approaches to enteral feeding and nutrition core curriculum. Gastrointest Endosc. 2014;80(1):34–41. https://doi.org/10.1016/j.gie.2014.02.011.
Byrne KR, Fang JC. Endoscopic placement of enteral feeding catheters. Curr Opin Gastroenterol. 2006;22(5):546–50. https://doi.org/10.1097/01.mog.0000239871.12081.7f.
Fontana RJ, Barnett JL. Jejunostomy tube placement in refractory diabetic gastroparesis: a retrospective review. Am J Gastroenterol. 1996;91(10):2174–8.
Smith D, Soucy P. Complications of long-term jejunostomy in children. J Pediatr Surg. 1996;31(6):787–90.
Myers JG, Page CP, Stewart RM, Schwesinger WH, Sirinek KR, Aust JB. Complications of needle catheter jejunostomy in 2,022 consecutive applications. Am J Surg. 1995;170(6):547–50. discussion 50-1
Maple JT, Petersen BT, Baron TH, Gostout CJ, Wong Kee Song LM, Buttar NS. Direct percutaneous endoscopic jejunostomy: outcomes in 307 consecutive attempts. Am J Gastroenterol. 2005;100(12):2681–8. https://doi.org/10.1111/j.1572-0241.2005.00334.x.
Fan AC, Baron TH, Rumalla A, Harewood GC. Comparison of direct percutaneous endoscopic jejunostomy and PEG with jejunal extension. Gastrointest Endosc. 2002;56(6):890–4. https://doi.org/10.1067/mge.2002.129607.
Fortunato JE, Darbari A, Mitchell SE, Thompson RE, Cuffari C. The limitations of gastro-jejunal (G-J) feeding tubes in children: a 9-year pediatric hospital database analysis. Am J Gastroenterol. 2005;100(1):186–9. https://doi.org/10.1111/j.1572-0241.2005.40893.x.
Zopf Y, Rabe C, Bruckmoser T, Maiss J, Hahn EG, Schwab D. Percutaneous endoscopic jejunostomy and jejunal extension tube through percutaneous endoscopic gastrostomy: a retrospective analysis of success, complications and outcome. Digestion. 2009;79(2):92–7. https://doi.org/10.1159/000207808.
Delegge M, Buck G, Fang J, Disario J, Lehman G, Ginsberg G, et al. Randomized prospective comparison of Direct Percutaneous Endoscopic Jejunostomy (DPEJ) feeding tube placement versus Percutaneous Endoscopic Gastrostomy Feeding Tube Placement with Jejunal Extension (PEG-J), for enteral feeding. Gastrointest Endosc. 2006;63(5):AB160. https://doi.org/10.1016/j.gie.2006.03.320.
Udorah MO, Fleischman MW, Bala V, Cai Q. Endoscopic clips prevent displacement of intestinal feeding tubes: a long-term follow-up study. Dig Dis Sci. 2010;55(2):371–4. https://doi.org/10.1007/s10620-009-0726-3.
Itkin M, DeLegge MH, Fang JC, McClave SA, Kundu S, d'Othee BJ, et al. Multidisciplinary practical guidelines for gastrointestinal access for enteral nutrition and decompression from the Society of Interventional Radiology and American Gastroenterological Association (AGA) Institute, with endorsement by Canadian Interventional Radiological Association (CIRA) and Cardiovascular and Interventional Radiological Society of Europe (CIRSE). Gastroenterology. 2011;141(2):742–65. https://doi.org/10.1053/j.gastro.2011.06.001.
Karamanolis G, Tack J. Nutrition and motility disorders. Best Pract Res Clin Gastroenterol. 2006;20(3):485–505. https://doi.org/10.1016/j.bpg.2006.01.005.
Choi YB. Laparoscopic gatrojejunostomy for palliation of gastric outlet obstruction in unresectable gastric cancer. Surg Endosc. 2002;16(11):1620–6. https://doi.org/10.1007/s00464-002-0010-5.
Chiu CC, Wang W, Huang MT, Wei PL, Chen TC, Lee WJ. Palliative gastrojejunostomy for advanced gastric antral cancer: double scope technique. J Laparoendosc Adv Surg Tech A. 2006;16(2):133–6. https://doi.org/10.1089/lap.2006.16.133.
Chen YI, Itoi T, Baron TH, Nieto J, Haito-Chavez Y, Grimm IS, et al. EUS-guided gastroenterostomy is comparable to enteral stenting with fewer re-interventions in malignant gastric outlet obstruction. Surg Endosc. 2017;31(7):2946–52. https://doi.org/10.1007/s00464-016-5311-1.
Khashab MA, Bukhari M, Baron TH, Nieto J, El Zein M, Chen YI, et al. International multicenter comparative trial of endoscopic ultrasonography-guided gastroenterostomy versus surgical gastrojejunostomy for the treatment of malignant gastric outlet obstruction. Endosc Int Open. 2017;5(4):E275–E81. https://doi.org/10.1055/s-0043-101695.
Pinson R, Pathirana I, Magulick J, Domanski J, Okoh E, Womeldorph C. Novel use of a uniquely designed, lumen-apposing, metal stent in benign gastric outlet obstruction in two patients. ACG Case Rep J. 2017;4:e20. https://doi.org/10.14309/crj.2017.20.
Tyberg A, Perez-Miranda M, Sanchez-Ocana R, Penas I, de la Serna C, Shah J, et al. Endoscopic ultrasound-guided gastrojejunostomy with a lumen-apposing metal stent: a multicenter, international experience. Endosc Int Open. 2016;4(3):E276–81. https://doi.org/10.1055/s-0042-101789.
Ayinala S, Batista O, Goyal A, Al-Juburi A, Abidi N, Familoni B, et al. Temporary gastric electrical stimulation with orally or PEG-placed electrodes in patients with drug refractory gastroparesis. Gastrointest Endosc. 2005;61(3):455–61.
Abell TL, Johnson WD, Kedar A, Runnels JM, Thompson J, Weeks ES, et al. A double-masked, randomized, placebo-controlled trial of temporary endoscopic mucosal gastric electrical stimulation for gastroparesis. Gastrointest Endosc. 2011;74(3):496–503 e3. https://doi.org/10.1016/j.gie.2011.05.022.
Deb S, Tang SJ, Abell TL, McLawhorn T, Huang WD, Lahr C, et al. Development of innovative techniques for the endoscopic implantation and securing of a novel, wireless, miniature gastrostimulator (with videos). Gastrointest Endosc. 2012;76(1):179–84. https://doi.org/10.1016/j.gie.2012.03.177.
Deb S, Tang SJ, Abell TL, Rao S, Huang WD, To SD, et al. An endoscopic wireless gastrostimulator (with video). Gastrointest Endosc. 2012;75(2):411–5, 5 e1. https://doi.org/10.1016/j.gie.2011.09.052.
Hajer J, Novak M. Development of an autonomous endoscopically implantable submucosal microdevice capable of neurostimulation in the gastrointestinal tract. Gastroenterol Res Pract. 2017;2017:8098067. https://doi.org/10.1155/2017/8098067.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Andrew Su, Jeffrey Conklin, and Alireza Sedarat declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Stomach and Duodenum.
Rights and permissions
About this article
Cite this article
Su, A., Conklin, J.L. & Sedarat, A. Endoscopic Therapies for Gastroparesis. Curr Gastroenterol Rep 20, 25 (2018). https://doi.org/10.1007/s11894-018-0630-0
Published:
DOI: https://doi.org/10.1007/s11894-018-0630-0