Abstract
Chronic constipation is a common health condition representing a substantial proportion of primary care visits and referrals to specialist providers. Chronic constipation can have a significant negative effect on health-related quality of life and has been associated with psychological distress in severely affected patients. It has the potential to cause patients to curtail work, school, and social activities. While different pathophysiological mechanisms have been implicated in the development of chronic constipation, in some instances, the causes of chronic constipation are not easily determined. Expenditures for the evaluation and management of chronic constipation represent a significant burden on patients and payers, and it is important for clinicians to have a clear understanding of the different pathophysiological mechanisms associated with constipation, understand the different testing modalities and treatments that are available including their appropriateness and limitations, and tailor that knowledge to the management of individual patients.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Suares N, Ford A. Prevalence of, and risk factors for, chronic idiopathic constipation in the community: systematic review and meta-analysis. Am J Gastroenterol. 2011;106(9):1582–91.
McCrea G, Miaskowski C, Stotts N, et al. A review of the literature on gender and age differences in the prevalence and characteristics of constipation in North America. J Pain Symptom Manag. 2009;37(4):737–45.
Mugie S, Benninga M, Di Lorenzo C. Epidemiology of constipation in children and adults: a systematic review. Best Pract Res Clin Gastroenterol. 2011;25(1):3–18.
Dennison C, Prasad M, Lloyd A, et al. The health-related quality of life and economic burden of constipation. PharmacoEconomics. 2005;23(5):461–76.
Sanchez MI, Bercik P. Epidemiology and burden of chronic constipation. Can J Gastroenterol. 2011;25(Suppl B):11B–5B.
Basilisco G, Coletta M. Chronic constipation: a critical review. Dig Liver Dis. 2013;45(11):886–93.
Bharucha A, Pemberton J, Locke G. American Gastroenterological Association technical review on constipation. Gastroenterology. 2013;144(1):218–38. A valuable comprehensive review of chronic constipation.
Herz M, Kahan E, Zalevski S, et al. Constipation: a different entity for patients and doctors. Fam Pract. 1996;13(2):156–9.
Longstreth G, Thompson W, Chey W, et al. Functional bowel disorders. Gastroenterology. 2006;130(5):1480–91.
Gallagher P, O'Mahony D. Constipation in old age. Best Pract Res Clin Gastroenterol. 2009;23(6):875–87.
Andromanakos NP, Pinis SI, Al K. Chronic severe constipation: current pathophysiological aspects, new diagnostic approaches, and therapeutic options. Eur J Gastroenterol Hepatol. 2015;27(3):204–14.
Xu L, WY W, Jiang J, et al. Clinical benefits after soluble dietary fiber supplementation: a randomized clinical trial in adults with slow-transit constipation. Zhonghua Yi Xue Za Zhi. 2014;94(48):3813–6.
Voderholzer W, Schatke W, Mühldorfer B, et al. Clinical response to dietary fiber treatment of chronic constipation. Am J Gastroenterol. 1997;92(1):95–8.
Hammer J, Phillips S. Fluid loading of the human colon: effects on segmental transit and stool composition. Gastroenterology. 1993;105(4):988–98.
Stephen A, Wiggins H, Cummings J. Effect of changing transit time on colonic microbial metabolism in man. Gut. 1987;28(5):601–9.
Penning C, Steens J, van der Schaar P, et al. Motor and sensory function of the rectum in different subtypes of constipation. Scand J Gastroenterol. 2001;36(1):32–8.
Rao S, Seaton K, Miller M, et al. Psychological profiles and quality of life differ between patients with dyssynergia and those with slow transit constipation. J Psychosom Res. 2007;63(4):441–9.
Lembo A, Camilleri M. Chronic constipation. N Engl J Med. 2003;349(14):1360–8.
Mertz H, Naliboff B, Mayer E. Physiology of refractory chronic constipation. Am J Gastroenterol. 1999;94:609–15.
Preston D, Lennard-Jones J. Severe chronic constipation of young women: 'idiopathic slow transit constipation'. Gut. 1986;27(1):41–8.
He C, Burgart L, Wang L, et al. Decreased interstitial cell of Cajal volume in patients with slow-transit constipation. Gastroenterology. 2000;118(1):14–21.
Wedel T, Spiegler J, Soellner S, et al. Enteric nerves and interstitial cells of Cajal are altered in patients with slow-transit constipation and megacolon. Gastroenterology. 2002;123(5):1459–67.
Tzavella K, Riepl R, Klauser A, et al. Decreased substance P levels in rectal biopsies from patients with slow transit constipation. Eur J Gastroenterol Hepatol. 1996;8(12):1207–11.
Cortesini C, Cianchi F, Infantino A, et al. Nitric oxide synthase and VIP distribution in enteric nervous system in idiopathic chronic constipation. Dig Dis Sci. 1995;40(11):2450–5.
Vierhout ME, Schreuder HW, Veen HF. Severe slow-transit constipation following radical hysterectomy. Gynecol Oncol. 1993;51:401–3.
MacDonald A, Baxter J, Bessent R, et al. Gastric emptying in patients with constipation following childbirth and due to idiopathic slow transit. Br J Surg. 1997;84(8):1141–3.
Barnes P, Lennard-Jones J, Hawley P, et al. Hirschsprung's disease and idiopathic megacolon in adults and adolescents. Gut. 1986;27(5):534–41.
Tack J, Müller-Lissner S, Stanghellini V, et al. Diagnosis and treatment of chronic constipation—a European perspective. Neurogastroenterol Motil. 2011;23(8):697–710.
Bharucha AE, Wald A, Enck P, et al. Functional anorectal disorders. Gastroenterology. 2006;130(5):1510–8.
Chiarioni G, Whitehead WE, Pezza V, et al. Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology. 2006;130:657–64.
Rao S, Seaton K, Miller M, et al. Randomized controlled trial of biofeedback, sham feedback, and standard therapy for dyssynergic defecation. Clin Gastroenterol Hepatol. 2007;5(3):331–8.
Heymen S, Scarlett Y, Jones K, et al. Randomized, controlled trial shows biofeedback to be superior to alternative treatments for patients with pelvic floor dyssynergia-type constipation. Dis Colon Rectum. 2007;50(4):428–41.
Henderson P, DiPalma J. Diagnosing irritable bowel syndrome: a changing clinical paradigm. South Med J. 2011;104(3):195–9.
Lewis S, Heaton K. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997;32(9):920–4.
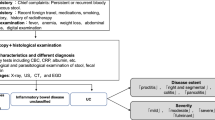
Rao S, Meduri K. What is necessary to diagnose constipation? Best Pract Res Clin Gastroenterol. 2011;25(1):127–40.
Tantiphlachiva K, Rao P, Attaluri A, et al. Digital rectal examination is a useful tool for identifying patients with dyssynergia. Clin Gastroenterol Hepatol. 2010;8(11):955–60.
Rao S, Ozturk R, Laine L. Clinical utility of diagnostic tests for constipation in adults: a systematic review. Am J Gastroenterol. 2005;100(7):1605–15.
American College of Gastroenterology Chronic Constipation Task Force. An evidence-based approach to the management of chronic constipation in North America. Am J Gastroenterol. 2005;100 suppl 1:S1–4.
Cash BD, Acosta RD, Chandrasekhara V, et al. The role of endoscopy in the management of constipation. Gastrointest Endosc. 2014;80(4):563–5.
Gupta M, Holub J, Knigge K, et al. Constipation is not associated with an increased rate of findings on colonoscopy: results from a national endoscopy consortium. Endoscopy. 2010;42(03):208–12.
Remes-Troche J, Rao S. Diagnostic testing in patients with chronic constipation. Curr Gastroenterol Rep. 2006;8(5):416–24.
Shorvon P, McHugh S, Diamant N, et al. Defecography in normal volunteers: results and implications. Gut. 1989;30(12):1737–49.
Gladman M, Aziz Q, Scott S, et al. Rectal hyposensitivity: pathophysiological mechanisms. Neurogastroenterol Motil. 2009;21(5), 508-e5.
Rao S. Dyssynergic defecation. Gastroenterol Clin N Am. 2001;30(1):97–114.
Rao S, Singh S. Clinical utility of colonic and anorectal manometry in chronic constipation. J Clin Gastroenterol. 2010;44(9):597–609. A superb review of colonic and anorectal manometry with detailed explanation on the technical aspects of the tests.
Deen K, Premaratna R, Fonseka M, et al. The recto-anal inhibitory reflex: abnormal response in diabetics suggests an intrinsic neuroenteropathy. J Gastroenterol Hepatol. 1998;13(11):1107–10.
Vorobyov G, Achkasov S, Biryukov O. Clinical features, diagnostics and treatment of Hirschsprung’s disease in adults. Color Dis. 2010;12(12):1242–8.
Lin H, Prather C, Fisher R, et al. Measurement of gastrointestinal transit. Dig Dis Sci. 2005;50(6):989–1004.
Rao S, Welcher K, Leistikow J. Obstructive defecation: a failure of rectoanal coordination. Am J Gastroenterol. 1998;93(7):1042–50.
Johanson J, Kralstein J. Chronic constipation: a survey of the patient perspective. Aliment Pharmacol Ther. 2007;25(5):599–608.
Müller-Lissner S, Tack J, Feng Y, et al. Levels of satisfaction with current chronic constipation treatment options in Europe—an internet survey. Aliment Pharmacol Ther. 2012;37(1):137–45.
Sahin M, Dogan I, Cengiz M, et al. The impact of anorectal biofeedback therapy on the quality of life of patients with dyssynergic defecation. Turk J Gastroenterol. 2015;26(2):140–4.
Lee H, Boo S, Jung K, et al. Long-term efficacy of biofeedback therapy in patients with dyssynergic defecation: results of a median 44 months follow-up. Neurogastroenterol Motil. 2015. A trial assessing the long-term efficacy of biofeedback therapy in a large group of patients with dyssynergic defecation, concluding that biofeedback therapy is durable and efficacy was maintained for more than 2 years in a sizable proportion of constipated patients with dyssynergic defecation.
Muller-Lissner S, Kamm M, Scarpignato C, et al. Myths and misconceptions about chronic constipation. Am J Gastroenterol. 2005;100(1):232–42.
Lacy B, Hussain Z, Mearin F. Treatment for constipation: new and old pharmacological strategies. Neurogastroenterol Motil. 2014;26(6):749–63.
Dukas L. Association between physical activity, fiber intake, and other lifestyle variables and constipation in a study of women. Am J Gastroenterol. 2003;98(8):1790–6.
DiPalma JA. Current treatment options for chronic constipation. Rev Gastroenterol Disord. 2004;4 Suppl 2:S34–42.
Tack J. Current and future therapies for chronic constipation. Best Pract Res Clin Gastroenterol. 2011;25(1):151–8.
Tack J, Müller–Lissner S. Treatment of chronic constipation: current pharmacologic approaches and future directions. Clin Gastroenterol Hepatol. 2009;7(5):502–8.
Cash BD, Lacy BE. Systematic review: FDA-approved prescription medications for adults with constipation. Gastroenterol Hepatol. 2006;2(10):736–49.
DiPalma J, Cleveland M, McGowan J, et al. A randomized, multicenter, placebo-controlled trial of polyethylene glycol laxative for chronic treatment of chronic constipation. Am J Gastroenterol. 2007;102(7):1436–41.
DiPalma J, Cleveland M, McGowan J, et al. A comparison of polyethylene glycol laxative and placebo for relief of constipation from constipating medications. South Med J. 2007;100(11):1085–90.
Di Palma J, Smith J, Cleveland M. Overnight efficacy of polyethylene glycol laxative. Am J Gastroenterol. 2002;97(7):1776–9.
Mueller-Lissner S, Kamm M, Wald A, et al. Multicenter, 4-week, double-blind, randomized, placebo-controlled trial of sodium picosulfate in patients with chronic constipation. Am J Gastroenterol. 2010;105(4):897–903.
Kamm M, Mueller–Lissner S, Wald A, et al. Oral bisacodyl is effective and well-tolerated in patients with chronic constipation. Clin Gastroenterol Hepatol. 2011;9(7):577–83.
Schiffhauer E, Vij N, Kovbasnjuk O, et al. Dual activation of CFTR and CLCN2 by lubiprostone in murine nasal epithelia. Am J Physiol Lung Cell Mol Physiol. 2013;304(5):L324–31.
Wilson N, Schey R. Lubiprostone in constipation: clinical evidence and place in therapy. Ther Adv Chronic Dis. 2015;6(2):40–50.
Johanson J, Morton D, Geenen J, et al. Multicenter, 4-week, double-blind, randomized, placebo-controlled trial of lubiprostone, a locally-acting type-2 chloride channel activator, in patients with chronic constipation. Am J Gastroenterol. 2008;103(1):170–7.
Fukudo S, Hongo M, Kaneko H, et al. Lubiprostone increases spontaneous bowel movement frequency and quality of life in patients with chronic idiopathic constipation. Clin Gastroenterol Hepatol. 2015;13(2):294–301. e5.
Barish C, Drossman D, Johanson J, et al. Efficacy and safety of lubiprostone in patients with chronic constipation. Dig Dis Sci. 2009;55(4):1090–7. This study assessed the efficacy and safety of lubiprostone in patients with chronic constipation. The authors concluded that lubiprostone produced a bowel movement in the majority of individuals within 24 h of initial dosing, with sustained improvement in frequency and other constipation symptoms over 4 weeks.
Drossman D, Chey W, Johanson J, et al. Clinical trial: lubiprostone in patients with constipation-associated irritable bowel syndrome—results of two randomized, placebo-controlled studies. Aliment Pharmacol Ther. 2009;29(3):329–41.
Cryer B, Katz S, Vallejo R, et al. A randomized study of lubiprostone for opioid-induced constipation in patients with chronic noncancer pain. Pain Med. 2014;15(11):1825–34. In this study, the authors assessed the efficacy and safety of lubiprostone 24 mg twice daily for the treatment of OIC in adult patients with non-cancer pain. The results confirmed superior efficacy of lubiprostone compared to placebo in terms of increasing SBM frequency, improvement in abdominal discomfort, straining, constipation severity, stool consistency, and patient satisfaction. In addition, lubiprostone was well-tolerated with no serious lubiprostone-related adverse events.
Love B, Johnson A, Smith L. Linaclotide: a novel agent for chronic constipation and irritable bowel syndrome. Am J Health Syst Pharm. 2014;71(13):1081–91.
Lembo A, Schneier H, Shiff S, et al. Two randomized trials of linaclotide for chronic constipation. N Engl J Med. 2011;365(6):527–36.
Johnston J, Kurtz C, Drossman D, et al. Pilot study on the effect of linaclotide in patients with chronic constipation. Am J Gastroenterol. 2009;104(1):125–32.
Lembo A, Kurtz C, MacDougall J, et al. Efficacy of linaclotide for patients with chronic constipation. Gastroenterology. 2010;138(3):886–95. e1.
Johnston J, Kurtz C, MacDougall J, et al. Linaclotide improves abdominal pain and bowel habits in a phase IIb study of patients with irritable bowel syndrome with constipation. Gastroenterology. 2010;139(6):1877–86. e2.
Rao S, Lembo A, Shiff S, et al. A 12-week, randomized, controlled trial with a 4-week randomized withdrawal period to evaluate the efficacy and safety of linaclotide in irritable bowel syndrome with constipation. Am J Gastroenterol. 2012;107(11):1714–24.
Chey W, Lembo A, Lavins B, et al. Linaclotide for irritable bowel syndrome with constipation: a 26-week, randomized, double-blind, placebo-controlled trial to evaluate efficacy and safety. Am J Gastroenterol. 2012;107(11):1702–12.
Wald A. Constipation. Curr Opin Gastroenterol. 2015;31(1):45–9.
Shailubhai K, Comiskey S, Foss J, et al. Plecanatide, an oral guanylate cyclase c agonist acting locally in the gastrointestinal tract, is safe and well-tolerated in single doses. Dig Dis Sci. 2013;58(9):2580–6.
Shailubhai K, Barrow L, Talluto C, et al. Plecanatide, a guanylate cyclase c agonist, improves bowel habits and symptoms associated with chronic constipation in a phase IIa clinical study. ACJ. 2011;11(S2):1174.
Simrén M, Bajor A, Gillberg P, et al. Randomised clinical trial: the ileal bile acid transporter inhibitor A3309 vs. placebo in patients with chronic idiopathic constipation—a double-blind study. Aliment Pharmacol Ther. 2011;34(1):41–50.
Wong B, Camilleri M, McKinzie S, et al. Effects of A3309, an ileal bile acid transporter inhibitor, on colonic transit and symptoms in females with functional constipation. Am J Gastroenterol. 2011;106(12):2154–64.
Chey W, Camilleri M, Chang L, et al. A randomized placebo-controlled phase IIb trial of a3309, a bile acid transporter inhibitor, for chronic idiopathic constipation. Am J Gastroenterol. 2011;106(10):1803–12.
Rao A, Wong B, Camilleri M, et al. Chenodeoxycholate in females with irritable bowel syndrome-constipation: a pharmacodynamic and pharmacogenetic analysis. Gastroenterology. 2010;139(5):1549–58. e1.
Portenoy R, Thomas J, Moehl Boatwright M, et al. Subcutaneous methylnaltrexone for the treatment of opioid-induced constipation in patients with advanced illness: a double-blind, randomized, parallel group, dose-ranging study. J Pain Symptom Manag. 2008;35(5):458–68.
Thomas J, Karver S, Cooney GA, et al. Methylnaltrexone for opioid-induced constipation in advanced illness. N Engl J Med. 2008;358(22):2332–43.
Mackey A, Green L, Greene P, et al. Methylnaltrexone and gastrointestinal perforation. J Pain Symptom Manag. 2010;40(1):e1–3.
Ford A, Brenner D, Schoenfeld P. Efficacy of pharmacological therapies for the treatment of opioid-induced constipation: systematic review and meta-analysis. Am J Gastroenterol. 2013;108(10):1566–74.
Vaughan-Shaw P, Fecher I, Harris S, et al. A meta-analysis of the effectiveness of the opioid receptor antagonist alvimopan in reducing hospital length of stay and time to GI recovery in patients enrolled in a standardized accelerated recovery program after abdominal surgery. Dis Colon Rectum. 2012;55(5):611–20.
Corsetti M, Tack J. Naloxegol, a new drug for the treatment of opioid-induced constipation. Expert Opin Pharmacother. 2015;16(3):399–406.
Schey R, Cromwell J, Rao S. Medical and surgical management of pelvic floor disorders affecting defecation. Am J Gastroenterol. 2012;107(11):1624–33. An excellent review of the diagnosis and management of different pelvic floor disorders causing constipation.
Chiarioni G, Salandini L, Whitehead W. Biofeedback benefits only patients with outlet dysfunction, not patients with isolated slow transit constipation. Gastroenterology. 2005;129(1):86–97.
Compliance with Ethics Guidelines
Conflict of Interest
Hani Sbahi declares no conflict of interest.
Brooks D. Cash reports personal fees from Takeda, Actavis, Astra Zeneca, Ironwood, and Sucampo, outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Large Intestine
Rights and permissions
About this article
Cite this article
Sbahi, H., Cash, B.D. Chronic Constipation: a Review of Current Literature. Curr Gastroenterol Rep 17, 47 (2015). https://doi.org/10.1007/s11894-015-0471-z
Published:
DOI: https://doi.org/10.1007/s11894-015-0471-z