Abstract
Purpose of Review
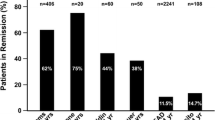
Type 2 diabetes (T2D) and obesity are comorbidities that generally progress with time even when non-invasive therapies are prescribed. Indeed, weight loss that is achieved with behavioral modification alone is generally inconsistent and often short-lived. In contrast, although patients do experience weight regain with metabolic surgery, they still benefit from a significant net decrease in weight. As a result, T2D remission can be achieved in up to 60% of patients within 2 years after surgery. However, it is unknown if the positive effects of metabolic surgery extend to macrovascular disease risk reduction.
Recent Findings
As noted in four randomized controlled trials (RCTs), Roux-en-Y gastric bypass (RYGB) facilitates partial remission of T2D in about 30% of volunteers 5 years after surgery. Of the four RCTs, only one investigated the effects of sleeve gastrectomy (SG) at 5 years; that study found that the rate of partial relapse was slightly lower with SG (23%). However, observational studies indicate that the gap between RYGB and SG may be larger than that observed in RCTs. In contrast, the rate of full remission is noted infrequently 5 years after SG or RYGB. Metabolic surgery also mitigates macrovascular disease risk as indicated by multiple observational studies.
Summary
The effects of metabolic surgery on cardiometabolic parameters are clinically meaningful. The weight loss that is facilitated by metabolic surgery reduces the metabolic and inflammatory stress caused by T2D and obesity. In turn, metabolic surgery likely mitigates macrovascular disease risk. Additional evidence from RCTs is needed to substantiate the effects of metabolic surgery on macrovascular disease risk.
Similar content being viewed by others
References
Nathan D, Barrett-Connor E, Crandall J, Edelstein S, Goldberg R, Horton E, et al. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the diabetes prevention program outcomes study. Lancet Diabetes Endocrinol. 2015;3(11):866–75.
Schauer P, Bhatt D, Kirwan J, Wolski K, Aminian A, Brethauer S, et al. Bariatric surgery versus intensive medical therapy for diabetes - 5-year outcomes. N Engl J Med. 2017;376(7):641–51.
Wing R, Bolin P, Brancati F, Bray G, Clark J, Coday M, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med. 2013;369(2):145–54.
Gregg E, Jakicic J, Blackburn G, Bloomquist P, Bray G, Clark J, et al. Association of the magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: a post-hoc analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol. 2016;4(11):913–21.
Ikramuddin S, Korner J, Lee W, Thomas A, Connett J, Bantle J, et al. Lifestyle intervention and medical management with vs without Roux-en-Y gastric bypass and control of hemoglobin A1c, LDL cholesterol, and systolic blood pressure at 5 years in the diabetes surgery study. JAMA. 2018;19(3):266–78.
Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Nanni G, et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2015;386(9997):964–73.
Courcoulas A, Gallagher J, Neiberg R, Eagleton E, DeLany J, Lang W, et al. Bariatric surgery vs lifestyle intervention for diabetes treatment: 5-year outcomes from a randomized trial. J Clin Endocrinol Metab. 2020;105(3):1–11.
Gnatiuc L, Herrington W, Halsey J, Tuomilehto J, Fang X, Kim H, et al. Sex-specific relevance of diabetes to occlusive vascular and other mortality: a collaborative meta-analysis of individual data from 980 793 adults from 68 prospective studies. Lancet Diabetes Endocrinol. 2018;6(7):538–46.
Aljofan M, Ding H. High glucose increases expression of cyclooxygenase-2, increases oxidative stress and decreases the generation of nitric oxide in mouse microvessel endothelial cells. J Cell Physiol. 2010;222(3):669–75.
Beisswenger P, Howell S, O'Dell R, Wood M, Touchette A, Szwergold B. Alpha-dicarbonyls increase in the postprandial period and reflect the degree of hyperglycemia. Diabetes Care. 2001;24(4):726–32.
Guimarães E, Empsen C, Geerts A, van Grunsven L. Advanced glycation end products induce production of reactive oxygen species via the activation of NADPH oxidase in murine hepatic stellate cells. J Hepatol. 2010;52(3):389–97.
Kheniser K, Kashyap S, Kasumov T. A systematic review: the appraisal of the effects of metformin on lipoprotein modification and function. Obes Sci Pract. 2018;5(1):36–45.
Saremi A, Howell S, Schwenke D, Bahn G, Beisswenger P, Reaven P. Advanced glycation end products, oxidation products, and the extent of atherosclerosis during the VA diabetes trial and follow-up study. Diabetes Care. 2017;40(4):591–8.
Sarwar N, Gao P, Seshasai S, Gobin R, Kaptoge S, Di Angelantonio E, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375(9733):2215–22.
Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Leccesi L, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366(17):1577–85.
Nannipieri M, Mari A, Anselmino M, Baldi S, Barsotti E, Guarino D, et al. The role of beta-cell function and insulin sensitivity in the remission of type 2 diabetes after gastric bypass surgery. J Clin Endocrinol Metab. 2011;96(9):E1372–E9.
Xiaosong W, Chongyu S, Xuqi S, Peiwu Y, Yongliang Z. Risk factors for relapse of hyperglycemia after laparoscopic Roux-en-Y gastric bypass in T2DM obese patients: a 5-year follow-up of 24 cases. Obes Surg. 2019;29(4):1164–8.
Miras A, Ravindra S, Humphreys A, Lascaratos G, Quartey K, Ahmed A, et al. Metabolic changes and diabetes microvascular complications 5 years after obesity surgery. Obes Surg. 2019;29(12):3907–11.
Adams T, Davidson L, Litwin S, Kim J, Kolotkin R, Nanjee M, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377(12):1143–55.
Malin S, Bena J, Abood B, Pothier C, Bhatt D, Nissen S, et al. Attenuated improvements in adiponectin and fat loss characterize type 2 diabetes non-remission status after bariatric surgery. Diabetes Obes Metab. 2014;16(12):1230–8.
Aminian A, Vidal J, Salminen P, Still C, Hanipah Z, Sharma G, et al. Late relapse of diabetes after bariatric surgery: not rare, but not a failure. Daibetes Care. 2020;43(3):534–40.
Hsu C, Almulaifi A, Chen J, Ser K, Chen S, Hsu K, et al. Effect of bariatric surgery vs medical treatment on type 2 diabetes in patients with body mass index lower than 35: five-year outcomes. JAMA Surg. 2015;150(12):1117–24.
Rubio-Almanza M, Hervás-Marín D, Cámara-Gómez R, Caudet-Esteban J, Merino-Torres J. Does metabolic surgery lead to diabetes remission in patients with BMI < 30 kg/m2?: a meta-analysis. Obes Surg. 2019;29(4):1105–16.
Kashyap S, Daud S, Kelly K, Gastaldelli A, Win H, Brethauer S, et al. Acute effects of gastric bypass versus gastric restrictive surgery on beta-cell function and insulinotropic hormones in severely obese patients with type 2 diabetes. Int J Obes. 2010;34(3):462–71.
Pérez-Pevida B, Escalada J, Miras A, Frühbeck G. Mechanisms underlying type 2 diabetes remission after metabolic surgery. Front Endocrinol. 2019;10:1–9.
Simonson D, Vernon A, Foster K, Halperin F, Patti M, Goldfine A. Adjustable gastric band surgery or medical management in patients with type 2 diabetes and obesity: three-year results of a randomized trial. Surg Obes Relat Dis. 2019;15(12):2052–9.
Courcoulas A, Belle S, Neiberg R, Pierson S, Eagleton J, Kalarchian M, et al. Three-year outcomes of bariatric surgery vs lifestyle intervention for type 2 diabetes mellitus treatment: a randomized clinical trial. JAMA Surg. 2015;150(10):931–40.
Simonson D, Halperin F, Foster K, Vernon A, Goldfine A. Clinical and patient-centered outcomes in obese patients with type 2 diabetes 3 years after randomization to Roux-en-Y gastric bypass surgery versus intensive lifestyle management: the SLIMM-T2D study. Diabetes Care. 2018;41(4):670–9.
McTigue K, Wellman R, Nauman E, Anau J, Coley R, Odor A, et al. Comparing the 5-year diabetes outcomes of sleeve gastrectomy and gastric bypass: the national patient-centered clinical research network (PCORNet) bariatric study. JAMA Surg. 2020;155(5):E1–E12. https://doi.org/10.1001/jamasurg.2020.0087.
Yska J, van Roon E, de Boer A, Leufkens H, Wilffert B, de Heide L, et al. Remission of type 2 diabetes mellitus in patients after different types of bariatric surgery: a population-based cohort study in the United Kingdom. JAMA Surg. 2015;150(12):1126–33.
Aminian A, Brethauer S, Andalib A, Nowacki A, Jimenez A, Corcelles R, et al. Individualized metabolic surgery score: procedure selection based on diabetes severity. Ann Surg. 2017;266(4):650–7.
Buse J, Caprio S, Cefalu W, Ceriello A, Del Prato S, Inzucchi S, et al. How do we define cure of diabetes? Diabetes Care. 2009;32(11):2133–5.
Kheniser K, Kashyap S. Diabetes management before, during, and after bariatric and metabolic surgery. J Diabetes Complicat. 2018;32(9):870–5.
Kashyap S, Kheniser K, Aminian A, Schauer P, Le Roux C, Burguera B. Double-blinded, randomized, and controlled study on the effects of canagliflozin after bariatric surgery: a pilot study. Obes Sci Pract. 2020;6(3):1–9.
Suliman M, Buckley A, Al Tikriti A, Tan T, le Roux C, Lessan N, et al. Routine clinical use of liraglutide 3 mg for the treatment of obesity: outcomes in non-surgical and bariatric surgery patients. Diabetes Obes Metab. 2019;21(6):1498–501. https://doi.org/10.1111/dom.13672.
Gorgojo-Martínez J, Feo-Ortega G, Serrano-Moreno C. Effectiveness and tolerability of liraglutide in patients with type 2 diabetes mellitus and obesity after bariatric surgery. Surg Obes Relat Dis. 2016;12(10):1856–63.
Rye P, Modi R, Cawsey S, Sharma A. Efficacy of high-dose liraglutide as an adjunct for weight loss in patients with prior bariatric surgery. Obes Surg. 2018;28(11):3553–8.
Shah A, Levesque K, Pierini E, Rojas B, Ahlers M, Stano S, et al. Effect of sitagliptin on glucose control in type 2 diabetes mellitus after Roux-en-Y gastric bypass surgery. Diabetes Obes Metab. 2018;20(4):1018–23.
Kheniser K, Kashyap S. Canagliflozin versus placebo for post-bariatric surgery patients with persistent type II diabetes: a randomized controlled trial (CARAT). Diabetes Obes Metab. 2017;19(4):609–10.
Neal B, Perkovic V, Mahaffey K, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57.
Zinman B, Wanner C, Lachin J, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28.
Marso S, Daniels G, Brown-Frandsen K, Kristensen P, Mann J, Nauck M, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311–22.
Marso S, Bain S, Consoli A, Eliaschewitz F, Jódar E, Leiter L, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375(19):1834–44.
Gerstein H, Colhoun H, Dagenais G, Diaz R, Lakshmanan M, Pais P, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 2019;394(10193):121–30.
Coleman K, Haneuse S, Johnson E, Bogart A, Fisher D, O'Connor P, et al. Long-term microvascular disease outcomes in patients with type 2 diabetes after bariatric surgery: evidence for the legacy effect of surgery. Daibetes Care. 2016;39(8):1400–7.
Bhatt D, Aminian A, Kashyap S, Kirwan J, Wolski K, Brethauer S, et al. Cardiovascular biomarkers after metabolic surgery versus medical therapy for diabetes. J Am Coll Cardiol. 2019;74(2):261–3.
O'Brien P, Hindle A, Brennan L, Skinner S, Burton P, Smith A, et al. Long-term outcomes after bariatric surgery: a systematic review and meta-analysis of weight loss at 10 or more years for all bariatric procedures and a single-centre review of 20-year outcomes after adjustable gastric banding. Obes Surg. 2019;29(1):3–14.
Lorkowski S, Brubaker G, Rotroff D, Kashyap S, Bhatt D, Nissen S, et al. Bariatric surgery improves HDL function examined by ApoA1 exchange rate and cholesterol efflux capacity in patients with obesity and type 2 diabetes. Biomolecules. 2020;10(4):1–13.
Kheniser K, Osme A, Kim C, Ilchenko S, Kasumov T, Kashyap S. Temporal dynamics of high-density lipoprotein proteome in diet-controlled subjects with type 2 diabetes. Biomolecules. 2020;10(4):1–16.
Saleheen D, Scott R, Javad S, Zhao W, Rodrigues A, Picataggi A, et al. Association of HDL cholesterol efflux capacity with incident coronary heart disease events: a prospective case-control study. Lancet Diabetes Endocrinol. 2015;3(7):507–13.
Aminian A, Zajichek A, Arterburn D, Wolski K, Brethauer S, Schauer P, et al. Predicting 10-year risk of end-organ complications of type 2 diabetes with and without metabolic surgery: a machine learning approach. Diabetes Care. 2020;43(4):852–9.
Oliveira S, Neves J, Souteiro P, Pedro J, Magalhães D, Guerreiro V, et al. Impact of bariatric surgery on long-term cardiovascular risk: comparative effectiveness of different surgical procedures. Obes Surg. 2020;30(2):673–80.
Shimada Y, Tsugawa Y, Iso H, Brown D, Hasegawa K. Association between bariatric surgery and rate of hospitalisations for stable angina pectoris in obese adults. Heart. 2017;103(13):1009–14.
Xue X, Kim M, Gaudet M, Park Y, Heo M, Hollenbeck A, et al. A comparison of the polytomous logistic regression and joint cox proportional hazards models for evaluating multiple disease subtypes in prospective cohort studies. Cancer Epidemiol Biomark Prev. 2013;22(2):275–85.
Pontiroli A, Ceriani V, Sarro G, Micheletto G, Giovanelli A, Zakaria A, et al. Incidence of diabetes mellitus, cardiovascular diseases, and cancer in patients undergoing malabsorptive surgery (biliopancreatic diversion and biliointestinal bypass) vs medical treatment. Obes Surg. 2019;29(3):935–42.
Johnson B, Blackhurst D, Latham B, Cull D, Bour E, Oliver T, et al. Bariatric surgery is associated with a reduction in major macrovascular and microvascular complications in moderately to severely obese patients with type 2 diabetes mellitus. J Am Coll Surg. 2013;216(4):545–56.
Fisher D, Johnson E, Haneuse S, Arterburn D, Coleman K, O'Connor P, et al. Association between bariatric surgery and macrovascular disease outcomes in patients with type 2 diabetes and severe obesity. JAMA. 2018;320(15):1570–82.
Aminian A, Zajichek A, Arterburn D, Wolski K, Brethauer S, Schauer P, et al. Association of metabolic surgery with major adverse cardiovascular outcomes in patients with type 2 diabetes and obesity. JAMA. 2019;322(13):1271–82.
Sjöström L, Peltonen M, Jacobson P, Ahlin S, Andersson-Assarsson J, Anveden Å, et al. Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. JAMA. 2014;311(22):2297–304.
Romeo S, Maglio C, Burza M, Pirazzi C, Sjöholm K, Jacobson P, et al. Cardiovascular events after bariatric surgery in obese subjects with type 2 diabetes. Daibetes Care. 2012;35(12):2613–7.
Sjöström L, Peltonen M, Jacobson P, Sjöström C, Karason K, Wedel H, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307(1):56–65.
Adams T, Gress R, Smith S, Halverson R, Simper S, Rosamond W, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357(8):753–61.
Aminian A, Aleassa E, Bhatt D, Tu C, Khorgami Z, Schauer P, et al. Bariatric surgery is associated with a lower rate of death after myocardial infarction and stroke: a nationwide study. Diabetes Obes Metab. 2019;21(9):2058–67.
Dalmar A, Singh M, Pandey B, Stoming C, Heis Z, Ammar K, et al. The beneficial effect of weight reduction on adverse cardiovascular outcomes following bariatric surgery is attenuated in patients with obstructive sleep apnea. Sleep. 2018;41(5):1–11.
Author information
Authors and Affiliations
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Macrovascular Complications in Diabetes
Rights and permissions
About this article
Cite this article
Kheniser, K.G., Aminian, A. & Kashyap, S.R. A Review of the Current Evidence: Impact of Metabolic Surgery on Diabetes Outcomes and Obesity-Associated Macrovascular Complications. Curr Diab Rep 20, 57 (2020). https://doi.org/10.1007/s11892-020-01350-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s11892-020-01350-8