Abstract
Purpose of Review
Despite mounting interest in the non-operative management (NOM, also known as watchful waiting) of rectal adenocarcinoma, limited guidance exists regarding appropriate patient selection and procedures. In this literature review targeting patients with operable adenocarcinoma of the rectum, we sought to evaluate NOM in terms of patient selection, management approaches, and outcomes with regard to both quality of life (QoL) and oncologic outcomes.
Recent Findings
Despite a lack of randomized evidence comparing NOM (performed via active surveillance following neoadjuvant chemotherapy and radiation) to neoadjuvant therapy followed by planned surgery, given that the vast majority of local, regional, and distant recurrences occur early in follow-up, the available evidence points to similar oncologic outcomes and possible QoL improvement. Due to the high chance of surgical salvage in the case of locoregional recurrence, close multidisciplinary follow-up is essential.
Conclusions
Under the care of an experienced multidisciplinary lower gastrointestinal team, NOM is feasible, is safe, and has the potential for improved QoL. A potential algorithm for clinically implementing NOM is described within this review.


Similar content being viewed by others
Abbreviations
- 5-FU:
-
Fluorouracil
- ADC:
-
Apparent diffusion coefficient
- CAPOX:
-
Capecitabine and oxaliplatin
- CEA:
-
Carcinogenic embryonic antigen
- cCR:
-
Complete clinical response
- CRT:
-
Chemoradiation
- CT:
-
Computed tomography
- CTV:
-
Clinical target volume
- CXB:
-
Contact brachytherapy
- DRE:
-
Digital rectal exam
- DWI:
-
Diffusion-weighted imaging
- EMVI:
-
Extramural vascular invasion
- FOLFOX:
-
Folinic acid, 5-FU, oxaliplatin
- GTV:
-
Gross tumor volume
- HDR:
-
High-dose rate
- LE:
-
Local excision
- LCRT:
-
Long-course chemoradiation
- MRI:
-
Magnetic resonance imaging
- NOM:
-
Non-operative management
- pCR:
-
Pathologic complete response
- PICOS:
-
Population, Intervention, Comparator, Outcome, and Study design
- PRISMA-S:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Literature Search Extension
- PRO:
-
Patient-reported outcome
- PTV:
-
Planning target volume
- QoL:
-
Quality of life
- RT:
-
Radiation therapy
- RCT:
-
Randomized controlled trial
- TEM:
-
Transanal endoscopic microsurgery
- TME:
-
Total mesorectal excision
- TNT:
-
Total neoadjuvant therapy
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004;351:1731–40.
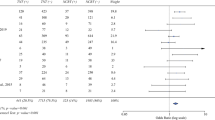
Dossa F, Chesney TR, Acuna SA, Baxter NN. A watch-and-wait approach for locally advanced rectal cancer after a clinical complete response following neoadjuvant chemoradiation: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2017;2:501–13 Meta-analysis comparing oncologic outcomes for NOM vs. patients who either had a cCR before surgery or pCR at time of surgery, with findings including no differences in non-regrowth recurrences or cancer-specific mortality between groups.
Ruppert R, Kube R, Strassburg J, et al. Avoidance of overtreatment of rectal cancer by selective chemoradiotherapy: results of the optimized surgery and MRI-based multimodal therapy trial. J Am Coll Surg. 2020. https://doi.org/10.1016/j.jamcollsurg.2020.06.023.
Battersby NJ, How P, Moran B, Stelzner S, West NP, Branagan G, et al. Prospective validation of a low rectal cancer magnetic resonance imaging staging system and development of a local recurrence risk stratification model: the MERCURY II study. Ann Surg. 2016;263:751–60.
Wrenn SM, Cepeda-Benito A, Ramos-Valadez DI, Cataldo PA. Patient perceptions and quality of life after colon and rectal surgery: what do patients really want? Dis Colon Rectum. 2018;61:971–8.
Couwenberg AM, Intven MPW, Burbach JPM, Emaus MJ, van Grevenstein WMU, Verkooijen HM. Utility scores and preferences for surgical and organ-sparing approaches for treatment of intermediate and high-risk rectal cancer. Dis Colon Rectum. 2018;61:911–9.
2017 European Society of Coloproctology (ESCP) collaborating group. Evaluating the incidence of pathological complete response in current international rectal cancer practice: the barriers to widespread safe deferral of surgery. Color Dis. 2018;20(Suppl 6):58–68.
Habr-Gama A, Perez RO, Nadalin W, Sabbaga J, Ribeiro U, Silva e Sousa AH, et al. Operative versus nonoperative treatment for stage 0 distal rectal cancer following chemoradiation therapy: long-term results. Ann Surg. 2004;240:711–7 discussion 717-718.
Crawford A, Firtell J, Caycedo-Marulanda A. How is rectal cancer managed: a survey exploring current practice patterns in Canada. J Gastrointest Cancer. 2019;50:260–8.
National Comprehensive Care Network. Rectal Carcinoma (Version 6.2020). https://www.nccn.org/professionals/physician_gls/pdf/rectal_blocks.pdf. All right reserved Accessed September 7, 2020.
Yahya J, Herzig D, Farrell M, Degnin C, Chen Y, Holland J, et al. Survey results of US radiation oncology providers’ contextual engagement of watch-and-wait beliefs after a complete clinical response to chemoradiation in patients with local rectal cancer. J Gastrointest Oncol. 2018;9:1127–32.
Kennedy ED, Borowiec AM, Schmocker S, Cho C, Brierley J, Li S, et al. Patient and physician preferences for nonoperative management for low rectal cancer: is it a reasonable treatment option? Dis Colon Rectum. 2018;61:1281–9.
Dattani M, Heald RJ, Goussous G, Broadhurst J, Sao Juliao GP, Habr-Gama A, et al. Oncological and survival outcomes in watch and wait patients with a clinical complete response after neoadjuvant chemoradiotherapy for rectal cancer: a systematic review and pooled analysis. Ann Surg. 2018;268:955–67 Meta-analysis noting frequency of cCR and the timing and frequency of the various patterns-of-failure including rectal tumor regrowth, nonregrowth pelvic recurrences, and distant metastases. An 82% R0 surgical salvage rate was noted.
Fiorica F, Trovo M, Anania G, Marcello D, Di Benedetto F, Marzola M, et al. Is it possible a conservative approach after radiochemotherapy in locally advanced rectal Cancer (LARC)? A systematic review of the literature and meta-analysis. J Gastrointest Cancer. 2019;50:98–108.
Huh JW, Maeda K, Liu Z, Wang X, Roslani AC, Lee WY. Current status of “watch-and-wait” rectal cancer treatment in Asia-Pacific countries. Ann Coloproctol. 2020;36:70–7.
Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, Page MJ, Koffel JB; PRISMA-S Group. PRISMA-S: an extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Syst Rev. 2021;26:1–39.
Chadi SA, Malcomson L, Ensor J, et al. Factors affecting local regrowth after watch and wait for patients with a clinical complete response following chemoradiotherapy in rectal cancer (InterCoRe consortium): an individual participant data meta-analysis. Lancet Gastroenterol Hepatol. 2018;3:825–36 Individual patient data meta-analysis showing that among 20 core variables across 11 data sets, a higher T-stage was the only factor associated with a risk of increased rectal tumor regrowth.
Smith JJ, Strombom P, Chow OS, Roxburgh CS, Lynn P, Eaton A, et al. Assessment of a watch-and-wait strategy for rectal cancer in patients with a complete response after neoadjuvant therapy. JAMA Oncol. 2019;5:e185896.
van der Valk MJM, Hilling DE, Bastiaannet E, Meershoek-Klein Kranenbarg E, Beets GL, Figueiredo NL, et al. Long-term outcomes of clinical complete responders after neoadjuvant treatment for rectal cancer in the International Watch & Wait Database (IWWD): an international multicentre registry study. Lancet. 2018;391:2537–45.
Renehan AG, Malcomson L, Emsley R, Gollins S, Maw A, Myint AS, et al. Watch-and-wait approach versus surgical resection after chemoradiotherapy for patients with rectal cancer (the OnCoRe project): a propensity-score matched cohort analysis. Lancet Oncol. 2016;17:174–83.
Habr-Gama A, Sabbaga J, Gama-Rodrigues J, São Julião GP, Proscurshim I, Bailão Aguilar P, et al. Watch and wait approach following extended neoadjuvant chemoradiation for distal rectal cancer: are we getting closer to anal cancer management? Dis Colon Rectum. 2013;56:1109–17.
Habr-Gama A, Gama-Rodrigues J, São Julião GP, Proscurshim I, Sabbagh C, Lynn PB, et al. Local recurrence after complete clinical response and watch and wait in rectal cancer after neoadjuvant chemoradiation: impact of salvage therapy on local disease control. Int J Radiat Oncol Biol Phys. 2014;88:822–8.
Martens MH, Maas M, Heijnen LA, Lambregts DMJ, Leijtens JWA, Stassen LPS, et al. Long-term outcome of an organ preservation program after neoadjuvant treatment for rectal cancer. J Natl Cancer Inst. 2016;108:djw171. https://doi.org/10.1093/jnci/djw171.
van der Sande ME, Figueiredo N, Beets GL. Management and outcome of local regrowths in a watch-and-wait prospective cohort for complete responses in rectal cancer. Ann Surg. 2020. https://doi.org/10.1097/SLA.0000000000003738.
Roxburgh CSD, Strombom P, Lynn P, Gonen M, Paty PB, Guillem JG, et al. Role of the interval from completion of neoadjuvant therapy to surgery in postoperative morbidity in patients with locally advanced rectal cancer. Ann Surg Oncol. 2019;26:2019–27.
Couwenberg AM, JPM B, Berbee M, et al. Efficacy of dose-escalated chemoradiation on complete tumor response in patients with locally advanced rectal cancer (RECTAL-BOOST): a phase 2 randomized controlled trial. Int J Radiat Oncol Biol Phys. 2020. https://doi.org/10.1016/j.ijrobp.2020.06.013Phase II trial RCT that did not find improvement in the rate of pCR or sustained cCR through dose escalation, with the experimental arm receiving a further 5 × 3 Gy boost following the standard arm’s 25 × 2 Gy with concurrent capecitabine.
Sao Juliao GP, Habr-Gama A, Vailati BB, et al. Is neoadjuvant chemoradiation with dose-escalation and consolidation chemotherapy sufficient to increase surgery-free and distant metastases-free survival in baseline cT3 rectal cancer? Eur J Surg Oncol. 2018;44:93–9.
Habr-Gama A, Sao Juliao GP, Vailati BB, Sabbaga J, Aguilar PB, Fernandez LM, et al. Organ preservation in cT2N0 rectal cancer after neoadjuvant chemoradiation therapy: the impact of radiation therapy dose-escalation and consolidation chemotherapy. Ann Surg. 2019;269:102–7.
Socha J, Pietrzak L, Zawadzka A, Paciorkiewicz A, Krupa A, Bujko K. A systematic review and meta-analysis of pT2 rectal cancer spread and recurrence pattern: implications for target design in radiation therapy for organ preservation. Radiother Oncol. 2019;133:20–7.
van der Sande ME, Hupkens BJP, Berbee M, van Kuijk SMJ, Maas M, Melenhorst J, et al. Impact of radiotherapy on anorectal function in patients with rectal cancer following a watch and wait programme. Radiother Oncol. 2019;132:79–84.
Rombouts AJM, Hugen N, Verhoeven RHA, Elferink MAG, Poortmans PMP, Nagtegaal ID, et al. Tumor response after long interval comparing 5x5Gy radiation therapy with chemoradiation therapy in rectal cancer patients. Eur J Surg Oncol. 2018;44:1018–24.
Lorenzon L, Evrard S, Beets G, Gonzalez-Moreno S, Kovacs T, D’Ugo D, et al. Global variation in the long-term outcomes of ypT0 rectal cancers. Eur J Surg Oncol. 2020;46:420–8.
Smart CJ, Korsgen S, Hill J, Speake D, Levy B, Steward M, et al. Multicentre study of short-course radiotherapy and transanal endoscopic microsurgery for early rectal cancer. Br J Surg. 2016;103:1069–75.
Jones HJS, Al-Najami I, Cunningham C. Quality of life after rectal-preserving treatment of rectal cancer. Eur J Surg Oncol. 2020;46:2050–6. https://doi.org/10.1016/j.ejso.2020.07.018.
Latkauskas T, Pauzas H, Kairevice L, Petrauskas A, Saladzinskas Z, Janciauskiene R, et al. Preoperative conventional chemoradiotherapy versus short-course radiotherapy with delayed surgery for rectal cancer: results of a randomized controlled trial. BMC Cancer. 2016;16:927.
Ciseł B, Pietrzak L, Michalski W, Wyrwicz L, Rutkowski A, Kosakowska E, et al. Long-course preoperative chemoradiation versus 5 × 5 Gy and consolidation chemotherapy for clinical T4 and fixed clinical T3 rectal cancer: long-term results of the randomized Polish II study. Ann Oncol. 2019;30:1298–303.
van der Valk MJM, Marijnen CAM, van Etten B, Dijkstra EA, Hilling DE, Kranenbarg EMK, et al. Compliance and tolerability of short-course radiotherapy followed by preoperative chemotherapy and surgery for high-risk rectal cancer - results of the international randomized RAPIDO-trial. Radiother Oncol. 2020;147:75–83.
Appelt AL, Ploen J, Harling H, Jensen FS, Jensen LH, Jorgensen JCR, et al. High-dose chemoradiotherapy and watchful waiting for distal rectal cancer: a prospective observational study. Lancet Oncol. 2015;16:919–27.
Dizdarevic E, Frostrup Hansen T, Ploen J, Henrik Jensen L, Lindebjerg J, Rafaelsen S, et al. Long-term patient-reported outcomes after high-dose chemoradiation therapy for nonsurgical management of distal rectal cancer. Int J Radiat Oncol Biol Phys. 2020;106:556–63.
Gerard J-P, Barbet N, Gal J, et al. Planned organ preservation for early T2-3 rectal adenocarcinoma: a French, multicentre study. Eur J Cancer. 2019;108:1–16.
Sun Myint A, Smith FM, Gollins SW, et al. Dose escalation using contact X-ray brachytherapy (Papillon) for rectal cancer: does it improve the chance of organ preservation? Br J Radiol. 2017;90:20170175.
Breugom AJ, Swets M, Bosset J-F, Collette L, Sainato A, Cionini L, et al. Adjuvant chemotherapy after preoperative (chemo)radiotherapy and surgery for patients with rectal cancer: a systematic review and meta-analysis of individual patient data. Lancet Oncol. 2015;16:200–7.
Cercek A, Roxburgh CSD, Strombom P, Smith JJ, Temple LKF, Nash GM, et al. Adoption of total neoadjuvant therapy for locally advanced rectal cancer. JAMA Oncol. 2018;4:e180071.
Garcia-Aguilar J, Chow OS, Smith DD, Marcet JE, Cataldo PA, Varma MG, et al. Effect of adding mFOLFOX6 after neoadjuvant chemoradiation in locally advanced rectal cancer: a multicentre, phase 2 trial. Lancet Oncol. 2015;16:957–66.
Smith RK, Fry RD, Mahmoud NN, Paulson EC. Surveillance after neoadjuvant therapy in advanced rectal cancer with complete clinical response can have comparable outcomes to total mesorectal excision. Int J Color Dis. 2015;30:769–74.
Fokas E, Allgäuer M, Polat B, et al. Randomized phase II trial of chemoradiotherapy plus induction or consolidation chemotherapy as total neoadjuvant therapy for locally advanced rectal cancer: CAO/ARO/AIO-12. J Clin Oncol. 2019;37:3212–22 Phase IIR study showing increased pCR with consolidation (i.e., post-chemoradiation) chemotherapy as opposed to induction chemotherapy (i.e., pre-chemoradiation).
Lezoche E, Baldarelli M, Lezoche G, Paganini AM, Gesuita R, Guerrieri M. Randomized clinical trial of endoluminal locoregional resection versus laparoscopic total mesorectal excision for T2 rectal cancer after neoadjuvant therapy. Br J Surg. 2012;99:1211–8 RCT of 100 Stage I, T2 N0 M0 rectal cancer patients who all received chemoradiation randomized to either LE or TME, with equivalent outcomes noted and no nodal failures despite no requirement for completion TME in the LE group for poor treatment response.
Garcia-Aguilar J, Renfro LA, Chow OS, Shi Q, Carrero XW, Lynn PB, et al. Organ preservation for clinical T2N0 distal rectal cancer using neoadjuvant chemoradiotherapy and local excision (ACOSOG Z6041): results of an open-label, single-arm, multi-institutional, phase 2 trial. Lancet Oncol. 2015;16:1537–46.
Rullier E, Rouanet P, Tuech J-J, et al. Organ preservation for rectal cancer (GRECCAR 2): a prospective, randomised, open-label, multicentre, phase 3 trial. Lancet. 2017;390:469–79 Phase III study of T2-3 N0-1 M0 patients showing no difference in outcomes following LCRT for LE vs. TME, although completion TME was required for adverse pathologic features at LE. Following LCRT, QoL was worst in the completion TME group, followed by the upfront TME patients and then LE alone patients.
Rullier E, Vendrely V, Asselineau J, Rouanet P, Tuech JJ, Valverde A, et al. Organ preservation with chemoradiotherapy plus local excision for rectal cancer: 5-year results of the GRECCAR 2 randomised trial. Lancet Gastroenterol Hepatol. 2020;5:465–74.
Vallam KC, Engineer R, Desouza A, Patil P, Saklani A. High nodal positivity rates even in good clinical responders after chemoradiation of rectal cancer: is organ preservation feasible? Color Dis. 2016;18:976–82.
Baucom RB, Maguire LH, Kavalukas SL, Geiger TM, Ford MM, Muldoon RL, et al. Nodal disease in rectal cancer patients with complete tumor response after neoadjuvant chemoradiation: danger below calm waters. Dis Colon Rectum. 2017;60:1260–6.
Creavin B, Ryan E, Martin ST, Hanly A, O’Connell PR, Sheahan K, et al. Organ preservation with local excision or active surveillance following chemoradiotherapy for rectal cancer. Br J Cancer. 2017;116:169–74.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Lynn PB, Strombom P, Garcia-Aguilar J. Organ-preserving strategies for the management of near-complete responses in rectal cancer after neoadjuvant chemoradiation. Clin Colon Rectal Surg. 2017;30:395–403.
Habr-Gama A, Lynn PB, Jorge JMN, Sao Juliao GP, Proscurshim I, Gama-Rodrigues J, et al. Impact of organ-preserving strategies on anorectal function in patients with distal rectal cancer following neoadjuvant chemoradiation. Dis Colon Rectum. 2016;59:264–9.
Mcmullen C, Liu L, Bulkley JE, Hornbrook MC, Wendel C, Grant M, et al. Participation in activities associated with quality of life for long-term survivors of rectal cancer. Perm J. 2017;21:16–011.
Hupkens BJP, Martens MH, Stoot JH, Berbee M, Melenhorst J, Beets-Tan RG, et al. Quality of life in rectal cancer patients after chemoradiation: watch-and-wait policy versus standard resection - a matched-controlled study. Dis Colon Rectum. 2017;60:1032–40 Matched controlled study of 41 patients who received NOM vs. 41 who received chemoradiation and surgery after minimum f/u of 2 years, with the NOM group having improved QoL in numerous domains based on validated questionnaires although significant side effects noted in each group.
Keane C, O’Grady G, Bissett I, Woodfield J. Comparison of bowel dysfunction between colorectal cancer survivors and a non-operative non-cancer control group. Color Dis. 2020;22:806–13.
Quezada-Diaz FF, Smith JJ, Jimenez-Rodriguez RM, Wasserman I, Pappou EP, Patil S, et al. Patient-reported bowel function in patients with rectal cancer managed by a watch-and-wait strategy after neoadjuvant therapy: a case-control study. Dis Colon Rectum. 2020;63:897–902.
Miller JA, Wang H, Chang DT, Pollom EL. Cost-effectiveness and quality-adjusted survival of watch and wait after complete response to chemoradiotherapy for rectal cancer. J Natl Cancer Inst. 2020;112:792–801 Markov decision analysis showing improved quality adjusted life years (QALYs) and decreased costs with comparable oncologic outcomes with NOM as compared to neoadjuvant CRT followed by surgery.
de Buck van Overstraeten A, Khorasani S, Kennedy E, Look Hong NJ. Nonoperative management versus radical surgery of rectal cancer after neoadjuvant therapy-induced clinical complete response: a Markov decision analysis. Dis Colon Rectum. 2020;63:1080–9.
Sclafani F, Brown G, Cunningham D, Wotherspoon A, Mendes LST, Balyasnikova S, et al. Comparison between MRI and pathology in the assessment of tumour regression grade in rectal cancer. Br J Cancer. 2017;117:1478–85.
van der Sande ME, Maas M, Melenhorst J, Breukink SO, van Leerdam ME, Beets GL. Predictive value of endoscopic features for a complete response after Chemoradiotherapy for rectal Cancer. Ann Surg. 2019. https://doi.org/10.1097/SLA.0000000000003718.
Nagtegaal ID, Glynne-Jones R. How to measure tumour response in rectal cancer? An explanation of discrepancies and suggestions for improvement. Cancer Treat Rev. 2020;84:101964.
Perez RO, Habr-Gama A, Pereira GV, Lynn PB, Alves PA, Proscurshim I, et al. Role of biopsies in patients with residual rectal cancer following neoadjuvant chemoradiation after downsizing: can they rule out persisting cancer? Color Dis. 2012;14:714–20.
van der Sande ME, Beets GL, Hupkens BJ, Breukink SO, Melenhorst J, Bakers FC, et al. Response assessment after (chemo)radiotherapy for rectal cancer: why are we missing complete responses with MRI and endoscopy? Eur J Surg Oncol. 2019;45:1011–7.
Liu S, Zhong G-X, Zhou W-X, Xue HD, Pan WD, Xu L, et al. Can endorectal ultrasound, MRI, and mucosa integrity accurately predict the complete response for mid-low rectal cancer after preoperative chemoradiation? A prospective observational study from a single medical center. Dis Colon Rectum. 2018;61:903–10.
Sao Juliao GP, Ortega CD, Vailati BB, Habr-Gama A, Fernandez LM, Gama-Rodrigues J, et al. Magnetic resonance imaging following neoadjuvant chemoradiation and transanal endoscopic microsurgery for rectal cancer. Color Dis. 2017;19:O196–203.
Hupkens BJP, Maas M, Martens MH, et al. Organ preservation in rectal cancer after chemoradiation: should we extend the observation period in patients with a clinical near-complete response? Ann Surg Oncol. 2018;25:197–203 Retrospective analysis of 102 patients found > 90% of patients with a near cCR 8-10 weeks after CRT will achieve a cCR 6–12 weeks later.
Habr-Gama A, Sao Juliao GP, Fernandez LM, Vailati BB, Andrade A, Araujo SEA, et al. Achieving a complete clinical response after neoadjuvant chemoradiation that does not require surgical resection: it may take longer than you think! Dis Colon Rectum. 2019;62:802–8. https://doi.org/10.1097/DCR.0000000000001338.
Sammour T, Price BA, Krause KJ, Chang GJ. Nonoperative management or “watch and wait” for rectal cancer with complete clinical response after neoadjuvant chemoradiotherapy: a critical appraisal. Ann Surg Oncol. 2017;24:1904–15.
Gani C, Kirschniak A, Zips D. Watchful waiting after radiochemotherapy in rectal cancer: when is it feasible? Visc Med. 2019;35:119–23.
Gani C, Grosse U, Clasen S, Kirschniak A, Goetz M, Rodel C, et al. Cost analysis of a wait-and-see strategy after radiochemotherapy in distal rectal cancer. Strahlenther Onkol. 2018;194:985–90.
Song K-S, Park SC, Sohn DK, et al. Oncologic risk of rectal preservation against medical advice after chemoradiotherapy for rectal cancer: a multicenter comparative cross-sectional study with rectal preservation as supported by surgeon. World J Surg. 2019;43:3216–23.
Oh BY, Huh JW, Lee WY, Park YA, Cho YB, Yun SH, et al. Are we predicting disease progress of the rectal cancer patients without surgery after neoadjuvant chemoradiotherapy? Cancer Res Treat. 2018;50:634–45.
Maas M, Lambregts DMJ, Nelemans PJ, et al. Assessment of clinical complete response after chemoradiation for rectal cancer with digital rectal examination, endoscopy, and MRI: selection for organ-saving treatment. Ann Surg Oncol. 2015;22:3873–80 Prospective cohort study of 50 patients that assessed likelihood of determining cCR based on DRE, endoscopy, T2W-MRI, and DWI 6–8 weeks after CRT with best accuracy noted with combined modality approach.
Sao Juliao GP, Karagkounis G, Fernandez LM, Habr-Gama A, Vailati BB, Dattani M, et al. Conditional survival in patients with rectal cancer and complete clinical response managed by watch and wait after chemoradiation: recurrence risk over time. Ann Surg. 2020;272:138–44.
Stijns RCH, de Graaf EJR, Punt CJA, Nagtegaal ID, Nuyttens JJME, van Meerten E, et al. Long-term oncological and functional outcomes of chemoradiotherapy followed by organ-sparing transanal endoscopic microsurgery for distal rectal cancer: the CARTS study. JAMA Surg. 2019;154:47–54.
van Heeswijk MM, Lambregts DMJ, Palm WM, Hendriks BMF, Maas M, Beets GL, et al. DWI for assessment of rectal cancer nodes after chemoradiotherapy: is the absence of nodes at DWI proof of a negative nodal status? AJR Am J Roentgenol. 2017;208:W79–84.
Santiago I, Barata M, Figueiredo N, Pares O, Henriques V, Galzerano A, et al. The split scar sign as an indicator of sustained complete response after neoadjuvant therapy in rectal cancer. Eur Radiol. 2020;30:224–38.
Wo JY, Anker CJ, Ashman JB, et al. Radiation therapy for rectal cancer: executive summary of an ASTRO clinical practice guideline. Pract Radiat Oncol. 2020. https://doi.org/10.1016/j.prro.2020.08.004.
Russo S, Anker CJ, Abdel-Wahab M, Azad N, Das P, Dragovic J, et al. Executive summary of the American Radium Society Appropriate Use Criteria for Local Excision in Rectal Cancer. Int J Radiat Oncol Biol Phys. 2019;105:977–93.
Garcia-Aguilar J, Patil S, Kim J. Preliminary results of the organ preservation of rectal adenocarcinoma (OPRA) trial. J Clin Oncol. 2020;38(suppl; abstr 4008).
Smith JJ, Chow OS, Gollub MJ, et al. Organ preservation in rectal adenocarcinoma: a phase II randomized controlled trial evaluating 3-year disease-free survival in patients with locally advanced rectal cancer treated with chemoradiation plus induction or consolidation chemotherapy, and total mesorectal excision or nonoperative management. BMC Cancer. 2015;15:767.
Acknowledgments
We would like to thank Rebecca Wilcox, MD, Director of Gastrointestinal Pathology at the University of Vermont, for her thorough read of this manuscript’s first draft.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Radiation Therapy and Radiation Therapy Innovations in Colorectal Cancer
Appendices
Appendix 1. Literature search strategy for non-operative management (NOM) of rectal adenocarcinoma

Appendix 2. Study selection flowsheet for the non-operative treatment (NOM) of rectal adenocarcinoma

Appendix 3
Rights and permissions
About this article
Cite this article
Anker, C.J., Akselrod, D., Ades, S. et al. Non-operative Management (NOM) of Rectal Cancer: Literature Review and Translation of Evidence into Practice. Curr Colorectal Cancer Rep 17, 23–41 (2021). https://doi.org/10.1007/s11888-020-00463-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11888-020-00463-2