Abstract
Purpose of Review
Influenza is the cause of millions of deaths yearly in the USA and globally. It presents a significant health burden in millions of people and is associated with chronic disease exacerbations including acute cardiovascular events such as myocardial infarction and stroke. We reviewed recent studies and a meta-analysis to assess the part that influenza vaccination plays in cardiovascular system protection.
Recent Findings
A sizable study measured the effect of influenza vaccination on cardiovascular health and mortality. This retrospective observational study used the 2012–2015 US National Inpatient Sample (NIS) database and included 22,634,643 hospitalizations. The patients who received the vaccine against influenza were associated with lower myocardial infarction (MI) (RR = 0.84, 95% CI: 0.82–0.87, p < 0.001), transient ischemic attack (TIA) (RR = 0.93, 95% CI: 0.9–0.96, p < 0.001), cardiac arrest (RR = 0.36, 95% CI: 0.33–0.39, p < 0.001), stroke (RR = 0.94, 95% CI: 0.91, 0.97, p < 0.001), and mortality (RR = 0.38, 95% CI: 0.36–0.4, p < 0.001).
Summary
Recent studies have reported a decrease in cardiovascular risk and mortality with influenza vaccine administration. Therefore, it is recommended to obtain the influenza vaccine (if there are no contraindications), especially individuals who are at risk of chronic disease exacerbations including acute cardiovascular events.
Similar content being viewed by others
Introduction
According to the Centers for Diseases and Control and Prevention (CDC), the burden of influenza in the USA varies, and the statistical data of influenza-related deaths is measured by taking several factors into account. These factors include the season timing, individual immunity, vaccine efficacy, and vaccine administration rates [1••]. Regardless of this variation, the burden of influenza continues to affect the health of the population in the USA. The CDC annually estimates the burden of seasonal influenza by obtaining rates of hospitalization with laboratory-confirmed influenza from Hospitalization Surveillance Network (FluSurv-NET) including outpatient medical visits and symptomatic community illness [2]. The FluSurv-NET includes an estimated 9% of the US population [3]. In the 2021–2022 season, the burden of influenza in the US was estimated to be between 8.0 and 13.0 million influenza illnesses, 3.7 and 6.1 million influenza-related medical visits, 82,000 and 170,000 hospitalizations, and 5000 and 14,000 influenza deaths [4]. Furthermore, a preliminary in-season burden from October 1, 2022, to December 31, 2022, estimates 22 to 43 million influenza illnesses, 10 to 21 million influenza medical visits, 230,000 to 490,000 influenza hospitalizations, and 14,000 to 43,000 influenza deaths [5].
The Global Influenza Programme of the WHO (World Health Organization) provides influenza surveillance information, which is distributed through FluNet and FluID (epidemiological data reported by national focal points) by Global Influenza Surveillance and Response System (GISRS) [6]. The implementation of these methods is imperative for the development of public health policy, identification of risk groups, and to plan for a future influenza pandemic. In a study, there were estimated influenza-associated excess mortality rates from countries with and without estimates using data from 1999 to 2015 from countries with annual influenza-associated excess mortality estimates. There is an estimation of 291,243 and 645,832 influenza-associated respiratory deaths (4.0–8.8 per 100 000 individuals) occurring annually [7]. This study does not account for cardiovascular exacerbations related to influenza. There is a high probability of seasonal influenza leading to death from other causes such as cardiovascular disease, chronic obstructive pulmonary disease, and pneumonia. We assessed recent studies and a meta-analysis about the cardiovascular outcomes in relation to influenza infection, and the benefits of influenza vaccine administration to cardiovascular health.
Influenza and Heightened Cardiovascular Risk
Influenza infection aggravates chronic conditions such as cardiovascular disease. Studies reported the association of influenza and acute cardiovascular events, such as myocardial infarction (MI), stroke, unstable angina, and hospitalizations due to heart failure exacerbations, as well as acute respiratory events. Influenza can lead to an MI by causing an inflammatory cytokine release, atherosclerotic disruption, and events causing thrombosis [8••].
A cross-sectional study evaluated acute cardiovascular events and determined risk factors for acute heart failure (aHF) and acute ischemic heart disease (alHD) in adults with a hospitalization associated with laboratory-confirmed influenza during influenza seasons from 2010 through 2018 using data from FluSurv-NET of 89,999 adults [9••]. Most patients experiencing aHF or alHD were aged 65 years or older and most patients experiencing acute myocarditis, acute pericarditis, or cardiogenic shock were aged 18 to 64 years. Among those patients experiencing an acute cardiovascular event, 53.5% had aHF, 49.3% alHD, 8.3% hypertensive crisis, 2.7% cardiogenic shock, 0.8% acute myocarditis, 0.5% acute pericarditis, and 0.2% cardiac tamponade. One in eight patients had sudden heart complications; almost one-third of these patients got admitted to the ICU and 7% died.
In a self-controlled case-series study, there was an association between laboratory-confirmed influenza infection and acute myocardial infarction [10]. There were 364 hospitalizations for acute myocardial infarction that happened within 1 year before and 1 year after tested positive for influenza. The incidence of admissions for acute myocardial infarction was six times as high during the 7 days after a positive laboratory-confirmed result of influenza infection as during the control interval.
In a recent meta-analysis of 6 RCTs published between 2000 and 2021, 9001 adults who were randomized to influenza vaccination versus matching placebo or standard care, 3.6% of vaccinated patients developed a major adverse cardiovascular event within 12 months compared with 5.4% of those who received placebo or control [11••]. From 4510 patients who received the influenza vaccine, 162 patients (3.6%) developed a major adverse cardiovascular event compared with 242 (5.4%) of the 4491 patients who received placebo or control within 12 months of follow-up (RR, 0.66; 95% CI, 0.53–0.83; I2 = 19%; p < 0.001).
Evidence on Influenza Vaccine in Mitigating Cardiovascular Risk
A retrospective observational study was conducted utilizing the NIS database between the years of 2012 and 2015 to evaluate the demographics and outcomes of combined vaccination among hospitalized patients in the USA [8••]. It was reported that from January 1, 2012, to September 30, 2015, there were 22,634,643 total hospitalizations recorded. There was a total of 696,399 hospitalizations where the patients were vaccinated. In this study, within the vaccinated group, patients were subcategorized to patients who received the influenza vaccine, patients who received the vaccine against pneumococcal pneumonia (PPV), and patients who received both vaccines during the hospital stay. The patients who received the vaccine against influenza with average age of 50 years old were associated with lower MI (RR = 0.84, 95% CI: 0.82–0.87, p < 0.001), transient ischemic attack (TIA) (RR = 0.93, 95% CI: 0.9–0.96, p < 0.001), cardiac arrest (RR = 0.36, 95% CI: 0.33–0.39, p < 0.001), stroke (RR = 0.94, 95% CI: 0.91, 0.97, p < 0.001), and mortality (RR = 0.38, 95% CI: 0.36–0.4, p < 0.001). There was a significant overall mortality risk reduction with combined vaccination, and the individual administration of pneumococcal and influenza vaccine was associated with improved cardiovascular outcomes. In this study, there was a mainly reduction in mortality for patients experiencing an MI. In addition, administration of pneumonia and influenza vaccines appears safe and supports the use of combined vaccination since the combined vaccination group also had a reduced risk of mortality among those admitted with MI (RR = 0.46), transient ischemic attacks (RR = 0.58), and stroke (RR = 0.42) compared to the unvaccinated group.
The IAMI trial (Influenza Vaccination After Myocardial Infarction) was a randomized, double-blind, placebo-controlled trial conducted to determine whether influenza vaccination early after admission with myocardial infarction or high-risk coronary artery disease reduces cardiovascular events [12•]. Thirty centers in 8 countries participated and the study was conducted from October 2016 through February 2020. A total of 1290 participants were assigned to the influenza vaccine and 1281 participants were assigned to placebo. A total of 1868 participants (74.3%) were treated with PCI, and 587 (23.4%) received medical treatment only. The composite of all-cause death, MI, or stent thrombosis at 12 months after randomization compared with placebo occurred in 67 patients (5.3%) assigned to influenza vaccine and 91 patients (7.2%) assigned to placebo (HR, 0.72 [95% CI, 0.52–0.99]; p = 0.040). Rates of cardiovascular death were 2.7% and 4.5%, respectively (HR, 0.59 [95% CI, 0.39–0.90]; p = 0.014), and rates of MI were 2.0% and 2.4%, respectively (HR, 0.86 [95% CI, 0.50–1.46]; p = 0.57). Although the country subgroup was not part of the prespecified subgroups, the treatment was tested for any effect that might differ by country and there was no evidence of treatment effect difference (interaction p = 0.75). In a recent review, several studies were evaluated and suggested that seasonal influenza vaccination is significantly effective in attenuating cardiovascular risk [13••]. The result of these studies included lower risk for acute heart failure and acute ischemic heart disease, myocardial infarction, stroke, pulmonary embolism, and cardiac arrest. Sen et al. [14••] explored the relationship between influenza vaccination and risk for acute myocardial infarction, stroke, and pulmonary embolism during the 2009 pandemic in Norway. During this time, vaccination was recommended for all adults. This cohort of 9952 individuals included 5524 vaccinated individuals who suffered from an acute MI (with mean age of 67.2 years; 68.3% males), 3434 from a stroke (with mean age of 69.9 years; 57.9% males), and 994 from pulmonary embolism (with mean age of 63.4 years; 51.3% males) during the study period from May 1, 2009, through September 30, 2010. There was an overall lower risk for cardiovascular events among those at higher risk following influenza vaccination in the period 1–14 days following vaccination when compared to the background period. The relative risks were 0.72 (0.59–0.88) for acute MI, 0.77 (0.59–0.99) for stroke, and 0.73 (0.45–1.19) for pulmonary embolism in that period. These associations remained the same up to 180 days after vaccination.
CDC and Public Health Guidance
In a cross-sectional study, there were 476,227 records of adults extracted with a self-reported history of cardiovascular disease from the Behavioral Risk Factor Surveillance System from January 2011 through December 2020 [15••]. The purpose of the study was to calculate the prevalence and likelihood of annual influenza vaccination by sociodemographic characteristics, healthcare characteristics, and cardiovascular disease risk factors. The annual trends of influenza vaccination by geographic region were also evaluated. The population included adults 65 years or older with or without CVD (51.2% vs 16.9%), male (55.4% vs 47.8%), non-Hispanic White (71.5% vs 64.3%), and a high school graduate or less (52.0% vs 40.3%), and have an annual household income of less than 50,000 (69.4% vs 50.4%). The majority of adults with CVD had health insurance (91.8%), healthcare provider (91.0%), and a visit with the healthcare provider within the year (85.5%). Adults with CVD were more compliant with influenza vaccination than adults without CVD. Overall, there has been an improvement in influenza vaccination coverage among adults with CVD during the past decade, but it is far from the targeted national goals. Only 16 states achieved a vaccination rate of 50% with no state achieving the Healthy People 2020 goal of 70%.
According to the CDC, everyone 6 months and older should get an influenza vaccine every season in the USA. This practice has been made a universal recommendation since the influenza season of 2010–2011 [16]. This recommendation is especially important to high-risk groups such as individuals with cardiovascular, and/or pulmonary disease. It is important to be up-to-date on influenza vaccine options to improve overall health. During 2022–2023 influenza season, vaccine options for individuals younger than 65 years include inactivated influenza vaccine [IIV], recombinant influenza vaccine [RIV], or live-attenuated influenza vaccine [LAIV], with no preference of any influenza vaccine over another. For this season, all influenza vaccines are quadrivalent vaccines [17]. These aim to protect against four different influenza viruses, including two influenza A and two influenza B. The standard-dose flu shots are approved for use in children from 6 months to 64 years only. Another alternative includes a cell-based influenza shot (Flucelvax Quadrivalent), which is approved to be administered on people who are 6 months and older. This vaccine is also egg-free.
In addition, the CDC recommends using the SHARE method by healthcare providers to increase influenza vaccine awareness and help patients make informed decisions about getting vaccinated [18]. Heart disease was one of the most common chronic conditions seen in hospitalized adults with influenza during recent seasons [19]. In 2020, CDC launched the Partnering for Vaccine Equity (P4VE) program that focuses on increasing adult immunization, especially targeting those groups that suffer from disparities in immunization such as racial and ethnic communities. The program provides funding and support to national, state, local, and community partners, who are prioritizing equity in vaccination access and uptake [20].
Conclusions
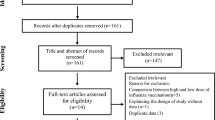
Influenza is affecting millions of people in the USA every year. There is evidence that influenza can exacerbate symptoms of chronic diseases such as heart failure and acute coronary syndromes. In these studies and the meta-analysis evaluated, there was an increase in cardiovascular protection with influenza vaccine administration. The characteristics of recent studies in relation to influenza vaccination status are summarized in Table 1. The CDC recommends routine annual influenza vaccination and especially for individuals with chronic conditions. The American College of Cardiology emphasizes the importance for all members of the cardiovascular team to incorporate the Standards for Adult Immunization Practice on every patient encounter by using the SHARE Model recommended by the CDC [21]. Furthermore, these findings showed the importance of social determinants of health that may be affecting the influenza vaccination rates among individuals who lack health insurance and primary care, have comorbidities, are of young age, and are part of racial and ethnic minority populations [15].
The recommendations for the 2022–2023 season include two updates compared with the recommended composition of last season’s US influenza vaccines. There were updates on the influenza A and the influenza B vaccine virus components [4]. As we currently see the potential cardiovascular effects of the coronavirus, it is especially important for high-risk individuals to remain consistent with annual influenza vaccination to attenuate health complications and be up-to-date on influenza vaccine for optimum protection.
Data Availability
The authors confirm that the data supporting the content of this review are available within the article.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Lu PJ, Hung MC, Srivastav A, Grohskopf LA, Kobayashi M, Harris AM, et al. Surveillance of vaccination coverage among adult population — United States, 2018. MMWR. Surveillance Summaries; 202;2021;70:1–26. https://doi.org/10.15585/mmwr.ss7003a1. This Morbidity and Mortality Weekly Report mentions the importance of maintaining update with vaccines as there are still a significant number of adults unprotected against vaccine-preventable diseases.
Rolfes MA, Foppa IM, Garg S, Flannery B, Brammer L, Singleton JA, et al. Annual estimates of the burden of seasonal influenza in the United States: a tool for strengthening influenza surveillance and preparedness. Influenza Other Respir Viruses. 2018;12:132–7. https://doi.org/10.1111/irv.12486.
Grohskopf LA, Sokolow LZ, Broder KR, Walter EB, Fry AM, Jernigan DB. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices— United States, 2018–19 Influenza Season. MMWR. Recommendations and Reports; 2018;67:1–20. https://doi.org/10.15585/mmwr.rr6703a1.
Merced-Morales A, Daly P, Abd Elal Al, et al. Influenza activity and composition of the 2022–23 influenza vaccine — United States, 2021–22 Season. MMWR Morb Mortal Wkly Rep 2022;71:913–919. https://doi.org/10.15585/mmwr.mm7129a1.
Center for Disease Control. 2022–2023 Preliminary In-Season Burden Estimate. 2023. https://www.cdc.gov/flu/about/burden/preliminary-in-season-estimates.htm. Accessed 10 Jan 2023.
World Health Organization. Influenza Update N° 435. 2022. https://www.who.int/publications/m/item/influenza-update-n-435. Accessed 20 Jan 2023
Iuliano AD, Roguski KM, Chang HH, Muscatello DJ, Palekar R, Tempia S, et al. Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. The Lancet. 2018;391:1285–300. https://doi.org/10.1016/S0140-6736(17)33293-2.
•• Ma J, Mena M, Mandania R, A, Ghosh A, Dodoo C, Dwivedi A, K, Mukherjee D. Associations between combined influenza and pneumococcal pneumonia vaccination and cardiovascular outcomes. Cardiology 2021;146:772–780. https://doi.org/10.1159/000519469. This study included 22,634,643 hospitalizations in which 705,051 received the influenza vaccine. Influenza vaccination was associated with lower MI, TIA, cardiac arrest, stroke, and overall mortality.
•• Chow EJ, Rolfes MA, O’Halloran A, et al. Acute cardiovascular events associated with influenza in hospitalized adults: a cross-sectional study. Ann Intern Med. 2020;173:605–13. https://doi.org/10.7326/M20-1509. There was a total of 89,999 adults with laboratory-confirmed influenza in which only 80,261 had completed medical records and ICD codes, and 11.7% had an acute cardiovascular event.
Kwong JC, Schwartz KL, Campitelli MA, Chung H, Crowcroft NS, Karnauchow T, et al. Acute myocardial infarction after laboratory-confirmed influenza infection. New England Journal of Medicine; 2018;378:345–53. https://doi.org/10.1056/NEJMoa1702090.
•• Behrouzi B, Bhatt DL, Cannon CP, Vardeny O, Lee DS, Solomon SD, et al. Association of influenza vaccination with cardiovascular risk. JAMA Network Open; 2022;5:e228873. https://doi.org/10.1001/jamanetworkopen.2022.8873. This meta-analysis of several randomized controlled trials included 9001 patients where influenza vaccine was associated with a lower risk of cardiovascular events.
• Fröbert O, Götberg M, Erlinge D, Akhtar Z, Christiansen EH, Macintyre CR, et al. Influenza vaccination after myocardial infarction: a randomized, double-blind, placebo-controlled, multicenter trial. Circulation. 2021;144:1476–84. https://doi.org/10.1161/CIRCULATIONAHA.121.057042. There was a total of 2571 patients who were randomized between October 2016 and March 2020. Influenza vaccination early after an MI or high-risk coronary heart disease resulted in a lower risk of death, MI, stent thrombosis, and overall cardiovascular death at 12 months compared to placebo.
•• Mares AC, Mukherjee D. Influenza vaccination in mitigating vascular events and risk. Curr Opin Cardiol. 2022 Dec 29. Epub ahead of print. PMID: 36728725. https://doi.org/10.1097/hco.0000000000001018. This review article covers important results from recent studies about the association of cardiovascular health and influenza vaccine.
•• Sen A, Bakken IJ, Govatsmark RES, et al. Influenza vaccination and risk for cardiovascular events: a nationwide self-controlled case series study. BMC Cardiovasc Disord. 2021;21:31. https://doi.org/10.1186/s12872-020-01836-z. This study included vaccinated Norwegian individuals who have had myocardial infarction, stroke, or pulmonary embolism from May 2009 through September 2010. There was a lower risk for cardiovascular events after influenza vaccine administration.
•• Parekh T, Javed Z, Khan SU, Xue H, Nasir K. Disparities in influenza vaccination coverage and associated factors among adults with cardiovascular disease, United States, 2011–2020. Prev Chronic Dis 2022;19:220154. https://doi.org/10.5888/pcd19.220154. In this cross-sectional study, 476,227 records of adults were extracted with a self-reported history of cardiovascular disease from January 2011 through December 2020. As a result of existing disparities, it was reported that influenza vaccination rates are still falling behind the national goals.
For Clinicians: Vaccination Summary. Center for Disease Control and Prevention. 2022. https://www.cdc.gov/flu/professionals/vaccination/vax-summary.htm#vaccinated. Accessed 10 Feb 2023.
Grohskopf LA, Alyanak E, Ferdinands JM, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices, United States, 2021–22 influenza season. MMWR Recomm Rep 2021;70(No. RR-5):1–28. DOI: https://doi.org/10.15585/mmwr.rr7005a1
Make a strong flu vaccine recommendation. Centers for Disease Control and Prevention. 2022. https://www.cdc.gov/flu/professionals/vaccination/flu-vaccine-recommendation.htm. Accessed 13 Feb 2023.
Heart Disease & Stroke. Centers for Disease Control and Prevention. 2022. https://www.cdc.gov/flu/highrisk/heartdisease.htm. Accessed 15 Feb 2023.
Partnering for Vaccine Equity. Centers for Disease Control and Prevention. 2022. https://www.cdc.gov/vaccines/health-equity/index.html. Accessed 17 Feb 2023.
King SC, Fiebelkorn AP, Sperling LS. Influenza vaccination: proven and effective cardiovascular disease prevention. American College of Cardiology. 2020. https://www.acc.org/latest-in-cardiology/articles/2020/11/02/14/42/influenza-vaccination-proven-and-effective-cvd-prevention. Accessed 19 Feb 2023.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ngwudike, C.J., Villalobos, A. Correlation Between Cardiovascular Protection and Influenza Vaccination. Curr Cardiol Rep 25, 571–576 (2023). https://doi.org/10.1007/s11886-023-01875-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-023-01875-w