Abstract
Purpose of Review
To provide an overview of mitral annular disjunction (MAD) and to discuss important challenges in diagnosis and management of MAD.
Recent Findings
MAD has regained interest in the context of sudden cardiac death (SCD) in patients with mitral valve prolapse (MVP), coined as the “arrhythmic” MVP syndrome. In addition, MAD in isolation was recently suggested to be associated with severe arrhythmia and SCD.
Summary
There is a lack of consensus on the definition of MAD and the imaging modality to be used for diagnosing MAD, and the therapeutic implications of MAD remain uncertain. Furthermore, the exact mechanism underlying the association of MAD with SCD remains largely unexplored.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Freed LA, Benjamin EJ, Levy D, Larson MG, Evans JC, Fuller DL, et al. Mitral valve prolapse in the general population. J Am Coll Cardiol Foundation. 2002;40:1298–304.
Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. The Lancet Elsevier. 2006;368:1005–11.
Antoine C, Benfari G, Michelena HI, Maalouf JF, Nkomo VT, Thapa P, et al. Clinical outcome of degenerative mitral regurgitation. Circulation American Heart Association. 2018;138:1317–26.
Nishimura RA, McGoon MD, Shub C, Miller FA, Ilstrup DM, Tajik AJ. Echocardiographically documented mitral-valve prolapse: long-term follow-up of 237 patients. N Engl J Med. 1985;313:1305–9.
Düren DR, Becker AE, Dunning AJ. Long-term follow-up of idiopathic mitral valve prolapse in 300 patients: a prospective study. J Am Coll Cardiol Foundation. 1988;11:42–7.
Marks AR, Choong CY, Sanfilippo AJ, Ferré M, Weyman AE. Identification of high-risk and low-risk subgroups of patients with mitral-valve prolapse. N Engl J Med. 1989;320:1031–6.
Zuppiroli A, Mori F, Favilli S, Barchielli A, Corti G, Montereggi A, et al. Arrhythmias in mitral valve prolapse: relation to anterior mitral leaflet thickening, clinical variables, and color Doppler echocardiographic parameters. Am Heart J. 1994;128:919–27.
Kim S, Kuroda T, Nishinaga M, Yamasawa M, Watanabe S, Mitsuhashi T, et al. Relationship between severity of mitral regurgitation and prognosis of mitral valve prolapse: echocardiographic follow-up study. Am Heart J. 1996;132:348–55.
Freed LA, Levy D, Levine RA, Larson MG, Evans JC, Fuller DL, et al. Prevalence and clinical outcome of mitral-valve prolapse. New Eng J Med. Massachusetts Med Soc. 1999;341:1–7.
•• Essayagh B, Sabbag A, Antoine C, Benfari G, Batista R, Yang L-T, et al. The mitral annular disjunction of mitral valve prolapse. JACC: Cardiovascular Imaging. 2021;14:2073–87. This study indicates that MAD is linked to advanced myxomatous degeneration and is associated with excess incidence of arrythmias.
Jeresaty RM. Sudden death in the mitral valve prolapse-click syndrome. Am J Cardiol. 1976;37:317–8.
Winkle RA, Lopes MG, Popp RL, Hancock EW. Life-threatening arrhythmias in the mitral valve prolapse syndrome. Am J Med. 1976;60:961–7.
DeMaria AN, Amsterdam EA, Vismara LA, Neumann A, Mason DT. Arrhythmias in the mitral valve prolapse syndrome. Prevalence, nature, and frequency. Ann Intern Med. 1976;84:656–60.
Martini B, Basso C, Thiene G. Sudden death in mitral valve prolapse with Holter monitoring-documented ventricular fibrillation: evidence of coexisting arrhythmogenic right ventricular cardiomyopathy. Int J Cardiol. 1995;49:274–8.
Avierinos J-F, Gersh BJ, Melton LJ, Bailey KR, Shub C, Nishimura RA, et al. Natural history of asymptomatic mitral valve prolapse in the community. Circulation. 2002;106:1355–61.
Sriram CS, Syed FF, Ferguson ME, Johnson JN, Enriquez-Sarano M, Cetta F, et al. Malignant bileaflet mitral valve prolapse syndrome in patients with otherwise idiopathic out-of-hospital cardiac arrest. J Am Coll Cardiol. 2013;62:222–30.
Hourdain J, Clavel MA, Deharo J-C, Asirvatham S, Avierinos JF, Habib G, et al. Common phenotype in patients with mitral valve prolapse who experienced sudden cardiac death. Circulation American Heart Association. 2018;138:1067–9.
Nalliah CJ, Mahajan R, Elliott AD, Haqqani H, Lau DH, Vohra JK, et al. Mitral valve prolapse and sudden cardiac death: a systematic review and meta-analysis. Heart. 2019;105:144–51.
Perazzolo Marra M, Basso C, De Lazzari M, Rizzo S, Cipriani A, Giorgi B, et al. Morphofunctional abnormalities of mitral annulus and arrhythmic mitral valve prolapse. Circulation: cardiovascular imaging. Am Heart Assoc. 2016;9:e005030.
Basso C, Perazzolo Marra M, Rizzo S, De Lazzari M, Giorgi B, Cipriani A, et al. Arrhythmic mitral valve prolapse and sudden cardiac death. Circulation. 2015;132:556–66.
Dejgaard LA, Skjølsvik ET, Lie ØH, Ribe M, Stokke MK, Hegbom F, et al. The Mitral annulus disjunction arrhythmic syndrome. J Am Coll Cardiol. 2018;72:1600–9.
Miller MA, Dukkipati SR, Turagam M, Liao SL, Adams DH, Reddy VY. Arrhythmic mitral valve prolapse. J Am Coll Cardiol Foundation. 2018;72:2904–14.
Essayagh B, Sabbag A, Antoine C, Benfari G, Yang L-T, Maalouf J, et al. Presentation and outcome of arrhythmic mitral valve prolapse. J Am Coll Cardiol. 2020;76:637–49.
Hutchins GM, Moore GW, Skoog DK. The association of floppy mitral valve with disjunction of the mitral annulus fibrosus. New Eng J Med. Massachusetts Med Soc. 1986;314:535–40.
Eriksson MJ, Bitkover CY, Omran AS, David TE, Ivanov J, Ali MJ, et al. Mitral annular disjunction in advanced myxomatous mitral valve disease: echocardiographic detection and surgical correction. J Am Soc Echocardiogr United States. 2005;18:1014–22.
Zimmerman J. The functional and surgical anatomy of the heart. Ann R Coll Surg Engl. 1966;39:348–66.
Bharati S, Granston AS, Liebson PR, Loeb HS, Rosen KM, Lev M. The conduction system in mitral valve prolapse syndrome with sudden death. Am Heart J. 1981;101:667–70.
Henle J. Handbuch der systematischen Anatomie des Menschen: Bd. 1. Abt. Gefässlehre. 2. verb. Aufl.. 2. Abt. Nervenlehre. 2. verb. Aufl. Vieweg; 1876.
McAlpine WA. Heart and coronary arteries: an anatomical atlas for clinical diagnosis, radiological investigation, and surgical treatment. na. 1975.
Angelini A. Disjunction of the mitral annulus in floppy mitral valve: [Letter]. N Engl J Med. Boston, United States: Massachusetts Medical Society. 1988;318:188–9.
Angelini A, Ho SY, Anderson RH, Davies MJ, Becker AE. A histological study of the atrioventricular junction in hearts with normal and prolapsed leaflets of the mitral valve. Heart. 1988;59:712–6.
Bennett S, Thamman R, Griffiths T, Oxley C, Khan JN, Phan T, et al. Mitral annular disjunction: a systematic review of the literature. Echocardiography. 2019;36:1549–58.
Toh H, Mori S, Izawa Y, Fujita H, Miwa K, Suzuki M, et al. Prevalence and extent of mitral annular disjunction in structurally normal hearts: comprehensive 3D analysis using cardiac computed tomography. European Heart Journal - Cardiovascular Imaging. 2021;22:614–22.
Basso C, Iliceto S, Thiene G, Perazzolo MM. Mitral valve prolapse, ventricular arrhythmias, and sudden death. Circulation United States. 2019;140:952–64.
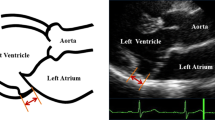
Carmo P, Andrade MJ, Aguiar C, Rodrigues R, Gouveia R, Silva JA. Mitral annular disjunction in myxomatous mitral valve disease: a relevant abnormality recognizable by transthoracic echocardiography. Cardiovasc Ultrasound. 2010;8:53.
Essayagh B, Mantovani F, Benfari G, Maalouf JF, Mankad S, Thapa P, et al. Mitral annular disjunction of degenerative mitral regurgitation: three-dimensional evaluation and implications for mitral repair. J Am Soc Echocardiogr United States. 2022;35:165–75.
Lee AP-W, Jin C-N, Fan Y, Wong RHL, Underwood MJ, Wan S. Functional implication of mitral annular disjunction in mitral valve prolapse. JACC: Cardiovascular Imaging. 2017;10:1424–33.
Perazzolo Marra M, Basso C, De Lazzari M, Rizzo S, Cipriani A, Giorgi B, et al. Morphofunctional abnormalities of mitral annulus and arrhythmic mitral valve prolapse. Circ Cardiovasc Imaging. 2016;9: e005030.
Toh H, Mori S, Izawa Y, Toba T, Watanabe Y, Kono AK, et al. Varied extent of mitral annular disjunction among cases with different phenotypes of mitral valve prolapse. JACC: Case Reports. 2021;3:1251–7.
Haugaa KH, Aabel EW. Mitral annulus disjunction. JACC Cardiovasc Imaging. 2021;14:2088–90.
Lee AP-W, Hsiung MC, Salgo IS, Fang F, Xie J-M, Zhang Y-C, et al. Quantitative analysis of mitral valve morphology in mitral valve prolapse with real-time 3-dimensional echocardiography: importance of annular saddle shape in the pathogenesis of mitral regurgitation. Circulation. 2013;127:832–41.
Konda T, Tani T, Suganuma N, Nakamura H, Sumida T, Fujii Y, et al. The analysis of mitral annular disjunction detected by echocardiography and comparison with previously reported pathological data. J Echocardiogr. 2017;15:176–85.
Tani T, Konda T, Kitai T, Ota M, Furukawa Y. Mitral annular disjunction—a new disease spectrum. Cardiol Clin. 2021;39:289–94.
Zoghbi WA, Adams D, Bonow RO, Enriquez-Sarano M, Foster E, Grayburn PA, et al. Recommendations for noninvasive evaluation of native valvular regurgitation. J Am Soc Echocardiogr. 2017;30:303–71.
•• Demolder A, Timmermans F, Duytschaever M, Muiño-Mosquera L, De Backer J. Association of mitral annular disjunction with cardiovascular outcomes among patients with Marfan syndrome. JAMA Cardiology. 2021;6:1177–86. This study indicates that MAD is associated with more need for mitral valve intervention, occurrence of malignant ventricular arrhythmias and (in patients with extensive MAD) more aortic events.
Mantegazza V, Tamborini G, Muratori M, Gripari P, Fusini L, Italiano G, et al. Mitral annular disjunction in a large cohort of patients with mitral valve prolapse and significant regurgitation. JACC: Cardiovascular Imaging. 2019;12:2278–80.
Kukavica D, Guglielmo M, Baggiano A, Muscogiuri G, Fusini L, Muratori M, et al. Arrhythmic mitral valve prolapse: introducing an era of multimodality imaging-based diagnosis and risk stratification. Diagnostics (Basel). 2021;11:467.
Faletra FF, Leo LA, Paiocchi VL, Schlossbauer SA, Pavon AG, Ho SY, et al. Morphology of mitral annular disjunction in mitral valve prolapse. J Am Soc Echocardiogr United States. 2022;35:176–86.
Constant Dit Beaufils A-L, Huttin O, Jobbe-Duval A, Senage T, Filippetti L, Piriou N, et al. Replacement myocardial fibrosis in patients with mitral valve prolapse. Circulation. American Heart Association; 2021;143:1763–74.
Enriquez-Sarano M. Mitral annular disjunction. JACC Cardiovasc Imaging. 2017;10:1434–6.
Roselli C, Yu M, Nauffal V, Georges A, Yang Q, Love K, et al. Genome-wide association study reveals novel genetic loci: a new polygenic risk score for mitral valve prolapse. Eur Heart J. 2022;ehac049.
Pedersen H. Mitral valve prolapse in the dog: a model of mitral valve prolapse in man. Cardiovasc Res. 2000;47:234–43.
Padang R, Bagnall RD, Semsarian C. Genetic basis of familial valvular heart disease. Circulation: Cardiovascular Genetics. American Heart Association; 2012;5:569–80.
Trenkwalder T, Krane M. Mitral valve prolapse: will genetics finally solve the puzzle? Eur Heart J. 2022;ehac048.
Ng CM, Cheng A, Myers LA, Martinez-Murillo F, Jie C, Bedja D, et al. TGF-β–dependent pathogenesis of mitral valve prolapse in a mouse model of Marfan syndrome. J Clin Invest. 2004;114:1586–92.
van Wijngaarden AL, de Riva M, Hiemstra YL, van der Bijl P, Fortuni F, Bax JJ, et al. Parameters associated with ventricular arrhythmias in mitral valve prolapse with significant regurgitation. Heart England. 2021;107:411–8.
De Backer JF, Devos D, Segers P, Matthys D, François K, Gillebert TC, et al. Primary impairment of left ventricular function in Marfan syndrome. Int J Cardiol. 2006;112:353–8.
El-Tallawi KC, Kitkungvan D, Xu J, Cristini V, Yang EY, Quinones MA, et al. Resolving the disproportionate left ventricular enlargement in mitral valve prolapse due to Barlow disease. JACC: Cardiovascular Imaging. 2021;14:573–84.
Yang L-T, Ahn SW, Li Z, Benfari G, Mankad R, Takeuchi M, et al. Mitral valve prolapse patients with less than moderate mitral regurgitation exhibit early cardiac chamber remodeling. J Am Soc Echocardiogr. 2020;33:815-825.e2.
Belhassen B. Radiofrequency ablation of “benign” right ventricular outflow tract extrasystoles*. J Am Coll Cardiol Foundation. 2005;45:1266–8.
Millar LM, Fanton Z, Finocchiaro G, Sanchez-Fernandez G, Dhutia H, Malhotra A, et al. Differentiation between athlete’s heart and dilated cardiomyopathy in athletic individuals. Heart. BMJ Publishing Group Ltd and British Cardiovascular Society; 2020;106:1059–65.
Pelliccia A, Culasso F, Di Paolo FM, Maron BJ. Physiologic left ventricular cavity dilatation in elite athletes. Ann Intern Med. 1999;130:23–31.
Paterick TE, Gordon T, Spiegel D. Echocardiography: profiling of the athlete’s heart. J Am Soc Echocardiogr. 2014;27:940–8.
Zia MI, Valenti V, Cherston C, Criscito M, Uretsky S, Wolff S. Relation of mitral valve prolapse to basal left ventricular hypertrophy as determined by cardiac magnetic resonance imaging. Am J Cardiol. 2012;109:1321–5.
Muthukumar L, Rahman F, Jan MF, Shaikh A, Kalvin L, Dhala A, et al. The Pickelhaube sign: novel echocardiographic risk marker for malignant mitral valve prolapse syndrome. JACC Cardiovasc Imaging. 2017;10:1078–80.
Maron BJ, Sherrid MV, Haas TS, Lindberg J, Kitner C, Lesser JR. Novel hypertrophic cardiomyopathy phenotype: segmental hypertrophy isolated to the posterobasal left ventricular free wall. Am J Cardiol. 2010;106:750–2.
Nutter DO, Wickliffe C, Gilbert CA, Moody C, King SB. The pathophysiology of idiopathic mitral valve prolapse. Circulation. 1975;52:297–305.
Vergara P, Scarfò I, Esposito A, Colantoni C, Palmisano A, Altizio S, et al. Characterization of the electrophysiological substrate in patients with Barlow’s disease. J Cardiovasc Electrophysiol United States. 2021;32:3179–86.
Gornick CC, Tobler HG, Pritzker MC, Tuna IC, Almquist A, Benditt DG. Electrophysiologic effects of papillary muscle traction in the intact heart. Circulation. 1986;73:1013–21.
Avierinos J-F, Inamo J, Grigioni F, Gersh B, Shub C, Enriquez-Sarano M. Sex Differences in morphology and outcomes of mitral valve prolapse. Ann Intern Med. American College of Physicians; 2008;149:787–94.
Motwani M, Venetucci L. Mitral annular disjunction arrhythmia syndrome in Marfan syndrome. Eur Heart J Case Rep. 2020;4:1–2.
Delhomme C, Lasne A, Milleron O, Arnoult F, Delorme G, Eliahou L, et al. Mitral valve prolapse, mitral annular disjunction, left ventricular basal hypertrophy and ventricular repolarization abnormalities in Marfan patients. Europ Heart J. 2021;42:ehab724.1698.
Servato ML, Lopez-Sainz A, Valente F, Fernandez-Galera R, Casas-Masnou G, Gutierrez L, et al. Mitral annular disjunction in patients with syndromic hereditary aorthopaties. Europ Heart J. 2021;42:ehab724.1993.
Chivulescu M, Krohg-Sørensen K, Scheirlynck E, Lindberg BR, Dejgaard LA, Lie ØH, et al. Mitral annulus disjunction is associated with adverse outcome in Marfan and Loeys-Dietz syndromes. Eur Heart J Cardiovasc Imaging. 2021;22:1035–44.
Pandis D, Anyanwu AC, Adams DH. Mitral annular disjunction: a contrary view. J Am Soc Echocardiogr. United States; 2022;35:239.
Essayagh B, Mantovani F, Benfari G, Enriquez-Sarano M. Of causality and inferences: mitral annular disjunction and its consequences-reply. J Am Soc Echocardiogr United States. 2022;35:239–41.
Sabbag A, Essayagh B, Barrera JDR, et al. EHRA expert consensus statement on arrhythmic mitral valve prolapse and mitral annular disjunction complex in collaboration with the ESC Council on valvular heart disease and the European Association of Cardiovascular Imaging endorsed by the Heart Rhythm Society by the Asia Pacific Heart Rhythm Society and by the Latin American Heart Rhythm Society. EP Europace. 2022:euac125. https://doi.org/10.1093/europace/euac125
Priori SG, Blomström-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: the task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European Society of Cardiology (ESC) endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J. 2015;36:2793–867.
Elliott P. Sudden cardiac death in hypertrophic cardiomyopathy: time to change the narrative. Eur Heart J. 2021;42:3945–7.
Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022;43:561–632.
Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP, Gentile F, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation American Heart Association. 2021;143:e72-227.
Karangelis D, Mylonas KS, Krommydas A, Loggos S, Androutsopoulou V, Stakos D, et al. Mitral annular disjunction: pathophysiology, pro-arrhythmic profile and repair pearls. Reviews in cardiovascular medicine. IMR press; 2022;23:117.
Kay JH, Krohn BG, Zubiate P, Hoffman RL. Surgical correction of severe mitral prolapse without mitral insufficiency but with pronounced cardiac arrhythmias. J Thorac Cardiovasc Surg. 1979;78:259–68.
Pocock WA, Barlow JB, Marcus RH, Barlow CW. Mitral valvuloplasty for life-threatening ventricular arrhythmias in mitral valve prolapse. Am Heart J. 1991;121:199–202.
Reece IJ, Cooley DA, Painvin GA, Okereke OUJ, Powers PL, Pechacek LW, et al. Surgical treatment of mitral systolic click syndrome: results in 37 patients. Ann Thorac Surg. 1985;39:155–8.
Naksuk N, Syed FF, Krittanawong C, Anderson MJ, Ebrille E, DeSimone CV, et al. The effect of mitral valve surgery on ventricular arrhythmia in patients with bileaflet mitral valve prolapse. Indian Pacing and Electrophysiology Journal. 2016;16:187–91.
Vaidya VR, DeSimone CV, Damle N, Naksuk N, Syed FF, Ackerman MJ, et al. Reduction in malignant ventricular arrhythmia and appropriate shocks following surgical correction of bileaflet mitral valve prolapse. J Interv Card Electrophysiol. 2016;46:137–43.
Brunec-Keller M, Scharf C, Radulovic J, Berdat PA, Attenhofer Jost CH, Vogt P, et al. Barlow disease: effect of mitral valve repair on ventricular arrhythmias in 82 patients in a retrospective long-term study. J Cardiovasc Surg (Torino). Italy; 2022;
Zhou N, Zhao Q, Zeng X, Zheng D, Yue J, Zhang K, et al. Association of mitral annular disjunction with premature cardiac mortality in a large series of autopsies. J Am Coll Cardiol United States. 2021;77:102–4.
Zienciuk A, Dabrowska-Kugacka A, Pazdyga A, Szwoch M, Raczak G, Danilowicz-Szmanowicz L. P875Arrhythmic mitral valve prolapse in a practice of an ICD implanting center - a real world data. EP Europace. 2018;20: i166.
Ermakov S, Gulhar R, Lim L, Bibby D, Fang Q, Nah G, et al. Left ventricular mechanical dispersion predicts arrhythmic risk in mitral valve prolapse. Heart. 2019;105:1063–9.
Konda T, Tani T, Suganuma N, Fujii Y, Ota M, Kitai T, et al. Mitral annular disjunction in patients with primary severe mitral regurgitation and mitral valve prolapse. Echocardiography. 2020;37:1716–22.
Mantegazza V, Volpato V, Gripari P, Ghulam Ali S, Fusini L, Italiano G, et al. Multimodality imaging assessment of mitral annular disjunction in mitral valve prolapse. Heart England. 2021;107:25–32.
Putnam AJ, Kebed K, Mor-Avi V, Rashedi N, Sun D, Patel B, et al. Prevalence of mitral annular disjunction in patients with mitral valve prolapse and severe regurgitation. Int J Cardiovasc Imaging. 2020;36:1363–70.
Christiansen J, Edwards C, Myerson S. Assessment of mitral annular disjunction by cardiac MRI in patients with mitral valve prolapse. Heart, Lung and Circulation. Elsevier; 2010;19:S165.
Van De Heyning CM, Holtackers RJ, Nazir MS, Grapsa J, Demetrescu C, Pype L, et al. Dark-blood late gadolinium enhancement CMR improves detection of papillary muscle fibrosis in patients with mitral valve prolapse. Eur J Radiol. 2022;147: 110118.
Clavel M, Hourdain J, Deharo J, Asirvatham SJ, Avierinos J, Ackerman MJ, et al. Mitral valve prolapse phenotypes associated with sudden cardiac death. Can J Cardiol. 2015;31:S159–60.
Funding
Dr. De Backer is supported as Senior Clinical Researcher by the Research Foundation–Flanders and by a grant for medical research from the Baillet Latour Funds.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None declared.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardiac PET, CT, and MRI
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Verbeke, J., Demolder, A., De Backer, J. et al. Mitral Annular Disjunction: Associated Pathologies and Clinical Consequences. Curr Cardiol Rep 24, 1933–1944 (2022). https://doi.org/10.1007/s11886-022-01806-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-022-01806-1