Abstract
Purpose of the Review
Ischemic heart disease is among the most common causes of morbidity and mortality worldwide. In its stable manifestation, obstructing coronary artery stenoses prevent myocardial blood flow from matching metabolic needs of the heart under exercise conditions, which manifests clinically as dyspnea or chest pain. Prolonged bouts of ischemia may result in permanent myocardial dysfunction, heart failure, and eventually reduced survival. The aim of the present work is to review currently available approaches to provide relief of ischemia in stable coronary artery disease (CAD).
Recent Findings
Several pharmacological and interventional approaches have proven effectiveness in reducing the burden of ischemia in stable CAD and allow for symptom control and quality of life improvement. However, substantial evidence in favor of improved survival with ischemia relief is lacking, and recently published randomized controlled trial suggests that only selected groups of patients may substantially benefit from this approach.
Summary
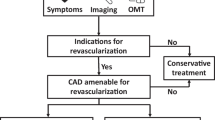
Pharmacological treatments aimed at reducing ischemia were shown to significantly reduce ischemic symptoms but failed to provide prognostic benefit. Myocardial revascularization is able to re-establish adequate coronary artery flow and was shown to improve survival in selected groups of patients, i.e., those with significant left main CAD or severe left ventricular dysfunction in multivessel CAD. Outside the previously mentioned categories, revascularization appears to improve symptoms control over medical therapy, but does not confer prognostic advantage. More studies are needed to elucidate the role of systematic invasive functional testing to identify individuals more likely to benefit from revascularization and to evaluate the prognostic role of chronic total occlusion recanalization.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2012;60(24):e44–164.
Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes: the task force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC). Eur Heart J. 2019;41(3):407–77. Available from:. https://doi.org/10.1093/eurheartj/ehz425.
Libby P, Pasterkamp G, Crea F, Jang I-K. Reassessing the mechanisms of acute coronary syndromes. Circ Res. 2019;124(1):150–60.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018;72(18):2231–64.
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart Disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation. 2020;141(9):e139–596.
Barbato E, Toth GG, Johnson NP, Pijls NHJ, Fearon WF, Tonino PAL, et al. A prospective natural history study of coronary atherosclerosis using fractional flow reserve. J Am Coll Cardiol. 2016;68(21):2247–55.
Kaski J-C, Crea F, Gersh BJ, Camici PG. Reappraisal of ischemic heart disease. Circulation. 2018;138(14):1463–80.
Gould KL, Lipscomb K. Effects of coronary stenoses on coronary flow reserve and resistance. Am J Cardiol. 1974;34(1):48–55. Available from:. https://doi.org/10.1016/0002-9149(74)90092-7.
Ardehali A, Ports TA. Myocardial oxygen supply and demand. Chest. 1990;98(3):699–705.
Rosano GMC, Fini M, Caminiti G, Barbaro G. Cardiac metabolism in myocardial ischemia. Curr Pharm Des. 2008;14(25):2551–62.
Janse MJ, Wit AL. Electrophysiological mechanisms of ventricular arrhythmias resulting from myocardial ischemia and infarction. Physiol Rev. 1989;69(4):1049–169.
Nesto RW, Kowalchuk GJ. The ischemic cascade: temporal sequence of hemodynamic, electrocardiographic and symptomatic expressions of ischemia. Am J Cardiol. 1987;59(7):23C–30C.
Wijns W, Serruys PW, Slager CJ, Grimm J, Krayenbuehl HP, Hugenholtz PG, et al. Effect of coronary occlusion during percutaneous transluminal angioplasty in humans on left ventricular chamber stiffness and regional diastolic pressure-radius relations. J Am Coll Cardiol. 1986;7(3):455–63.
Ohara T, Little WC. Evolving focus on diastolic dysfunction in patients with coronary artery disease. Curr Opin Cardiol. 2010;25(6):613–21.
Guaricci AI, Bulzis G, Pontone G, Scicchitano P, Carbonara R, Rabbat M, et al. Current interpretation of myocardial stunning. Trends Cardiovasc Med. 2018;28(4):263–71.
Foreman RD, Garrett KM, Blair RW. Mechanisms of cardiac pain. Compr Physiol. 2015;5(2):929–60.
Ryan MJ, Perera D. Identifying and managing hibernating myocardium: what’s new and what remains unknown? Curr Heart Fail Rep. 2018;15(4):214–23.
Rahimtoola SH. The hibernating myocardium. Am Heart J. 1989;117(1):211–21.
Garcia MJ, Kwong RY, Scherrer-Crosbie M, Taub CC, Blankstein R, Lima J, et al. State of the art: imaging for myocardial viability: a scientific statement from the American Heart Association. Circ Cardiovasc Imaging. 2020;13(7):e000053.
Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation. 2003;107(23):2900–7.
Zipes DP, Wellens HJ. Sudden cardiac death. Circulation. 1998;98(21):2334–51.
Bairey Merz CN, Pepine CJ, Walsh MN, Fleg JL. Ischemia and no obstructive coronary artery disease (INOCA): developing evidence-based therapies and research agenda for the next decade. Circulation. 2017;135(11):1075–92.
Kunadian V, Chieffo A, Camici PG, Berry C, Escaned J, Maas AHEM, et al. An EAPCI Expert consensus document on ischaemia with non-obstructive coronary arteries in collaboration with European society of cardiology working group on coronary pathophysiology & microcirculation endorsed by coronary vasomotor disorders international study group. Eur Heart J. 2020;41(37):3504–20. Available from. https://doi.org/10.1093/eurheartj/ehaa503.
Husted SE, Ohman EM. Pharmacological and emerging therapies in the treatment of chronic angina. Lancet. 2015;386(9994):691–701.
Murad F. Cyclic guanosine monophosphate as a mediator of vasodilation. J Clin Invest. 1986;78(1):1–5.
Bolotina VM, Najibi S, Palacino JJ, Pagano PJ, Cohen RA. Nitric oxide directly activates calcium-dependent potassium channels in vascular smooth muscle. Nature. 1994;368(6474):850–3.
Parker JD, Parker JO. Nitrate therapy for stable angina pectoris. N Engl J Med. 1998;338(8):520–31.
Bøttcher M, Madsen MM, Randsbaek F, Refsgaard J, Dørup I, Sørensen K, et al. Effect of oral nitroglycerin and cold stress on myocardial perfusion in areas subtended by stenosed and nonstenosed coronary arteries. Am J Cardiol. 2002;89(9):1019–24.
Thadani U. Challenges with nitrate therapy and nitrate tolerance: prevalence, prevention, and clinical relevance. Am J Cardiovasc Drugs. 2014;14(4):287–301.
Rousan TA, Mathew ST, Thadani U. Drug therapy for stable angina pectoris. Drugs. 2017;77(3):265–84.
Thadani U, Davidson C, Singleton W, Taylor SH. Comparison of the immediate effects of five beta-adrenoreceptor-blocking drugs with different ancillary properties in angina pectoris. N Engl J Med. 1979;300(14):750–5.
Huang HL, Fox KAA. The impact of beta-blockers on mortality in stable angina: a meta-analysis. Scott Med J. 2012;57(2):69–75.
Bangalore S, Steg G, Deedwania P, Crowley K, Eagle KA, Goto S, et al. β-Blocker use and clinical outcomes in stable outpatients with and without coronary artery disease. JAMA. 2012;308(13):1340–9.
Chatterjee S, Biondi-Zoccai G, Abbate A, D’Ascenzo F, Castagno D, Van Tassell B, et al. Benefits of β blockers in patients with heart failure and reduced ejection fraction: network meta-analysis. BMJ. 2013;346:f55.
Abernethy DR, Schwartz JB. Calcium-antagonist drugs. N Engl J Med. 1999;341(19):1447–57.
Rehnqvist N, Hjemdahl P, Billing E, Björkander I, Eriksson SV, Forslund L, et al. Effects of metoprolol vs verapamil in patients with stable angina pectoris. The Angina Prognosis Study in Stockholm (APSIS). Eur Heart J. 1996;17(1):76–81.
Poole-Wilson PA, Lubsen J, Kirwan B-A, van Dalen FJ, Wagener G, Danchin N, et al. Effect of long-acting nifedipine on mortality and cardiovascular morbidity in patients with stable angina requiring treatment (ACTION trial): randomised controlled trial. Lancet. 2004;364(9437):849–57.
Joannides R, Moore N, Iacob M, Compagnon P, Lerebours G, Menard J-F, et al. Comparative effects of ivabradine, a selective heart rate-lowering agent, and propranolol on systemic and cardiac haemodynamics at rest and during exercise. Br J Clin Pharmacol. 2006;61(2):127–37.
Tardif J-C, Ford I, Tendera M, Bourassa MG, Fox K. Efficacy of ivabradine, a new selective I(f) inhibitor, compared with atenolol in patients with chronic stable angina. Eur Heart J. 2005;26(23):2529–36.
Werdan K, Ebelt H, Nuding S, Höpfner F, Hack G, Müller-Werdan U. Ivabradine in combination with beta-blocker improves symptoms and quality of life in patients with stable angina pectoris: results from the ADDITIONS study. Clin Res Cardiol. 2012;101(5):365–73.
Fox K, Ford I, Steg PG, Tendera M, Ferrari R. Ivabradine for patients with stable coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a randomised, double-blind, placebo-controlled trial. Lancet. 2008;372(9641):807–16.
Tarkin JM, Kaski JC. Nicorandil and long-acting nitrates: vasodilator therapies for the management of chronic stable angina pectoris. Eur Cardiol. 2018;13(1):23–8.
Thadani U. Can nicorandil treat angina pectoris effectively? Nat Clin Pract Cardiovasc Med. 2005;2(4):186–7.
Cocco G, Rousseau MF, Bouvy T, Cheron P, Williams G, Detry JM, et al. Effects of a new metabolic modulator, ranolazine, on exercise tolerance in angina pectoris patients treated with beta-blocker or diltiazem. J Cardiovasc Pharmacol. 1992;20(1):131–8.
Belardinelli L, Shryock JC, Fraser H. Inhibition of the late sodium current as a potential cardioprotective principle: effects of the late sodium current inhibitor ranolazine. Heart. 2006;92 Suppl 4(Suppl 4):iv6–14.
Thadani U, Ezekowitz M, Fenney L, Chiang YK. Double-blind efficacy and safety study of a novel anti-ischemic agent, ranolazine, versus placebo in patients with chronic stable angina pectoris. Ranolazine Study Group. Circulation. 1994;90(2):726–34.
Chaitman BR, Skettino SL, Parker JO, Hanley P, Meluzin J, Kuch J, et al. Anti-ischemic effects and long-term survival during ranolazine monotherapy in patients with chronic severe angina. J Am Coll Cardiol. 2004;43(8):1375–82.
Peng S, Zhao M, Wan J, Fang Q, Fang D, Li K. The efficacy of trimetazidine on stable angina pectoris: a meta-analysis of randomized clinical trials. Int J Cardiol. 2014;177(3):780–5.
Marzilli M, Klein WW. Efficacy and tolerability of trimetazidine in stable angina: a meta-analysis of randomized, double-blind, controlled trials. Coron Artery Dis. 2003;14(2):171–9.
Driessen RS, Danad I, Stuijfzand WJ, Schumacher SP, Knuuti J, Mäki M, et al. Impact of revascularization on absolute myocardial blood flow as assessed by serial [(15)O]H(2)O positron emission tomography imaging: a comparison with fractional flow reserve. Circ Cardiovasc Imaging. 2018;11(5):e007417.
Boden WE, O’Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356(15):1503–16.
Maron DJ, Hochman JS, Reynolds HR, Bangalore S, O’Brien SM, Boden WE, et al. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med. 2020;382(15):1395–407 Main results of the ISCHEMIA Trial, again showing comparable outcomes for revascularization of non left main stem lesions in stable coronary artery disease and optimal medical therapy.
Al-Lamee R, Thompson D, Dehbi H-M, Sen S, Tang K, Davies J, et al. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet. 2018;391(10115):31–40 First randomized-controlled study on myocardial revascularization to include a sham procedure to serve as placebo arm. It showed substantial placebo effect associated with the procedure.
Tonino PAL, De Bruyne B, Pijls NHJ, Siebert U, Ikeno F. van’ t Veer M, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360(3):213–24.
Xaplanteris P, Fournier S, Pijls NHJ, Fearon WF, Barbato E, Tonino PAL, et al. Five-year outcomes with pci guided by fractional flow reserve. N Engl J Med. 2018;379(3):250–9 Five year follow up of the FAME 2 study, showing that FFR-guided revascularization provides a significant prognostic advantage over optimal medical therapy in stable ischemic heart disease.
Rahimtoola SH. Coronary bypass surgery for chronic angina--1981. A perspective. Circulation. 1982;65(2):225–41.
Reul GJJ, Cooley DA, Wukasch DC, Kyger ER 3rd, Sandiford FM, Hallman GL, et al. Long-term survival following coronary artery bypass. Analysis of 4,522 consecutive patients. Arch Surg. 1975;110(11):1419–24.
Spencer FC, Isom OW, Glassman E, Boyd AD, Engelman RM, Reed GE, et al. The long-term influence of coronary bypass grafts on myocardial infarction and survival. Ann Surg. 1974;180(4):439–51.
Long-term results of prospective randomised study of coronary artery bypass surgery in stable angina pectoris. European Coronary Surgery Study Group. Lancet. 1982;2(8309):1173–80.
Detre K, Peduzzi P, Murphy M, Hultgren H, Thomsen J, Oberman A, et al. Effect of bypass surgery on survival in patients in low- and high-risk subgroups delineated by the use of simple clinical variables. Circulation. 1981;63(6):1329–38.
Coronary artery surgery study (CASS): a randomized trial of coronary artery bypass surgery. Survival data. Circulation. 1983;68(5):939–50.
Yusuf S, Zucker D, Peduzzi P, Fisher LD, Takaro T, Kennedy JW, et al. Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the coronary artery bypass graft surgery trialists collaboration. Lancet. 1994;344(8922):563–70 Provides formal demonstration of prognostic impact of revascularization of the left main stem.
Bittl JA, He Y, Jacobs AK, Yancy CW, Normand S-LT. Bayesian methods affirm the use of percutaneous coronary intervention to improve survival in patients with unprotected left main coronary artery disease. Circulation. 2013;127(22):2177–85.
Tam DY, Bakaeen F, Feldman DN, Kolh P, Lanza GA, Ruel M, et al. Modality selection for the revascularization of left main disease. Can J Cardiol. 2019;35(8):983–92.
Azzalini L, Stone GW. Percutaneous coronary intervention or surgery for unprotected left main disease: excel trial at 5 years. Interv Cardiol Clin. 2020;9(4):419–32.
Feldman DN, Gade CL, Slotwiner AJ, Parikh M, Bergman G, Wong SC, et al. Comparison of outcomes of percutaneous coronary interventions in patients of three age groups (<60, 60 to 80, and >80 years) (from the New York State Angioplasty Registry). Am J Cardiol. 2006;98(10):1334–9.
Katritsis DG, Ioannidis JPA. Percutaneous coronary intervention versus conservative therapy in nonacute coronary artery disease: a meta-analysis. Circulation. 2005;111(22):2906–12.
Sedlis SP, Hartigan PM, Teo KK, Maron DJ, Spertus JA, Mancini GBJ, et al. Effect of PCI on Long-term survival in patients with stable ischemic heart disease. N Engl J Med. 2015;373(20):1937–46 Long-term follow up of the COURAGE trial, showing the lack of advantage of percutaneous revascularization over optimal medical therapy in stable ischemic heart disease.
Sedlis SP, Jurkovitz CT, Hartigan PM, Kolm P, Goldfarb DS, Lorin JD, et al. Health status and quality of life in patients with stable coronary artery disease and chronic kidney disease treated with optimal medical therapy or percutaneous coronary intervention (post hoc findings from the COURAGE trial). Am J Cardiol. 2013;112(11):1703–8.
Shaw LJ, Berman DS, Maron DJ, Mancini GBJ, Hayes SW, Hartigan PM, et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the clinical outcomes utilizing revascularization and aggressive drug evaluation (COURAGE) trial nuclear substudy. Circulation. 2008;117(10):1283–91.
Maron DJ, Hochman JS, O’Brien SM, Reynolds HR, Boden WE, Stone GW, et al. International study of comparative health effectiveness with medical and invasive approaches (ISCHEMIA) trial: rationale and design. Am Heart J. 2018;201:124–35.
Spertus JA, Jones PG, Maron DJ, O’Brien SM, Reynolds HR, Rosenberg Y, et al. Health-status outcomes with invasive or conservative care in coronary disease. N Engl J Med. 2020;382(15):1408–19.
Bangalore S, Maron DJ, O’Brien SM, Fleg JL, Kretov EI, Briguori C, et al. Management of coronary disease in patients with advanced kidney disease. N Engl J Med. 2020;382(17):1608–18.
Al-Lamee R, Howard JP, Shun-Shin MJ, Thompson D, Dehbi H-M, Sen S, et al. Fractional flow reserve and instantaneous wave-free ratio as predictors of the placebo-controlled response to percutaneous coronary intervention in stable single-vessel coronary artery disease. Circulation. 2018;138(17):1780–92.
Lima RSL, Watson DD, Goode AR, Siadaty MS, Ragosta M, Beller GA, et al. Incremental value of combined perfusion and function over perfusion alone by gated SPECT myocardial perfusion imaging for detection of severe three-vessel coronary artery disease. J Am Coll Cardiol. 2003;42(1):64–70.
Topol EJ, Nissen SE. Our preoccupation with coronary luminology. The dissociation between clinical and angiographic findings in ischemic heart disease. Circulation. 1995;92(8):2333–42.
Pijls NH, De Bruyne B, Peels K, Van Der Voort PH, Bonnier HJ, Bartunek J, et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med. 1996;334(26):1703–8.
Ciccarelli G, Barbato E, Toth GG, Gahl B, Xaplanteris P, Fournier S, et al. Angiography versus hemodynamics to predict the natural history of coronary stenoses: fractional flow reserve versus angiography in multivessel evaluation 2 substudy. Circulation. 2018;137(14):1475–85.
Gheorghiade M, Sopko G, De Luca L, Velazquez EJ, Parker JD, Binkley PF, et al. Navigating the crossroads of coronary artery disease and heart failure. Circulation. 2006;114(11):1202–13.
Pitt M, Lewis ME, Bonser RS. Coronary artery surgery for ischemic heart failure: risks, benefits, and the importance of assessment of myocardial viability. Prog Cardiovasc Dis. 2001;43(5):373–86.
O’Connor CM, Velazquez EJ, Gardner LH, Smith PK, Newman MF, Landolfo KP, et al. Comparison of coronary artery bypass grafting versus medical therapy on long-term outcome in patients with ischemic cardiomyopathy (a 25-year experience from the Duke cardiovascular disease databank). Am J Cardiol. 2002;90(2):101–7.
Velazquez EJ, Lee KL, Deja MA, Jain A, Sopko G, Marchenko A, et al. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med. 2011;364(17):1607–16.
Velazquez EJ, Lee KL, Jones RH, Al-Khalidi HR, Hill JA, Panza JA, et al. Coronary-artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med. 2016;374(16):1511–20 Long term follow up of the STICH trial.
Bonow RO, Maurer G, Lee KL, Holly TA, Binkley PF, Desvigne-Nickens P, et al. Myocardial viability and survival in ischemic left ventricular dysfunction. N Engl J Med. 2011;364(17):1617–25.
Panza JA, Ellis AM, Al-Khalidi HR, Holly TA, Berman DS, Oh JK, et al. Myocardial viability and long-term outcomes in ischemic cardiomyopathy. N Engl J Med. 2019;381(8):739–48.
Azzalini L, Jolicoeur EM, Pighi M, Millán X, Picard F, Tadros V-X, et al. Epidemiology, management strategies, and outcomes of patients with chronic total coronary occlusion. Am J Cardiol. 2016;118(8):1128–35.
Werner GS, Surber R, Ferrari M, Fritzenwanger M, Figulla HR. The functional reserve of collaterals supplying long-term chronic total coronary occlusions in patients without prior myocardial infarction. Eur Heart J. 2006;27(20):2406–12.
Råmunddal T, Hoebers LP, Henriques JPS, Dworeck C, Angerås O, Odenstedt J, et al. Prognostic impact of chronic total occlusions: a report from SCAAR (Swedish coronary angiography and angioplasty registry). JACC Cardiovasc Interv. 2016;9(15):1535–44.
Christakopoulos GE, Christopoulos G, Carlino M, Jeroudi OM, Roesle M, Rangan BV, et al. Meta-analysis of clinical outcomes of patients who underwent percutaneous coronary interventions for chronic total occlusions. Am J Cardiol. 2015;115(10):1367–75.
Werner GS, Martin-Yuste V, Hildick-Smith D, Boudou N, Sianos G, Gelev V, et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J. 2018;39(26):2484–93.
Obedinskiy AA, Kretov EI, Boukhris M, Kurbatov VP, Osiev AG, Ibn Elhadj Z, et al. The IMPACTOR-CTO Trial. JACC Cardiovasc Interv. United States. 2018;11:1309–11.
Lee S-W, Lee PH, Ahn J-M, Park D-W, Yun S-C, Han S, et al. Randomized trial evaluating percutaneous coronary intervention for the treatment of chronic total occlusion. Circulation. 2019;139(14):1674–83.
Brilakis ES, Mashayekhi K, Tsuchikane E, Abi Rafeh N, Alaswad K, Araya M, et al. Guiding principles for chronic total occlusion percutaneous coronary intervention. Circulation. 2019;140(5):420–33.
Kennedy JA, Beck-Oldach K, McFadden-Lewis K, Murphy GA, Wong YW, Zhang Y, et al. Effect of the anti-anginal agent, perhexiline, on neutrophil, valvular and vascular superoxide formation. Eur J Pharmacol. 2006;531(1–3):13–9.
Schmidt-Schweda S, Holubarsch C. First clinical trial with etomoxir in patients with chronic congestive heart failure. Clin Sci (Lond). 2000;99(1):27–35.
Vicari RM, Chaitman B, Keefe D, Smith WB, Chrysant SG, Tonkon MJ, et al. Efficacy and safety of fasudil in patients with stable angina: a double-blind, placebo-controlled, phase 2 trial. J Am Coll Cardiol. 2005;46(10):1803–11.
Noman A, Ang DSC, Ogston S, Lang CC, Struthers AD. Effect of high-dose allopurinol on exercise in patients with chronic stable angina: a randomised, placebo controlled crossover trial. Lancet. 2010;375(9732):2161–7.
McGillion M, Cook A, Victor JC, Carroll S, Weston J, Teoh K, et al. Effectiveness of percutaneous laser revascularization therapy for refractory angina. Vasc Health Risk Manag. 2010;6:735–47.
Konigstein M, Giannini F, Banai S. The Reducer device in patients with angina pectoris: mechanisms, indications, and perspectives. Eur Heart J. 2018;39(11):925–33.
Verheye S, Jolicœur EM, Behan MW, Pettersson T, Sainsbury P, Hill J, et al. Efficacy of a device to narrow the coronary sinus in refractory angina. N Engl J Med. 2015;372(6):519–27.
Giannini F, Palmisano A, Baldetti L, Benedetti G, Ponticelli F, Rancoita PMV, et al. Patterns of regional myocardial perfusion following coronary sinus reducer implantation: insights by stress cardiac magnetic resonance. Circ Cardiovasc Imaging. 2019;12:e009148.
Fukumoto Y, Ito A, Uwatoku T, Matoba T, Kishi T, Tanaka H, et al. Extracorporeal cardiac shock wave therapy ameliorates myocardial ischemia in patients with severe coronary artery disease. Coron Artery Dis. 2006;17(1):63–70.
Ahlbom M, Hagerman I, Ståhlberg M, Manouras A, Förstedt G, Wu E, et al. Increases in cardiac output and oxygen consumption during enhanced external counterpulsation. Heart Lung Circ. 2016;25(11):1133–6.
Qin X, Deng Y, Wu D, Yu L, Huang R. Does enhanced external counterpulsation (EECP) significantly affect myocardial perfusion?: a systematic review & meta-analysis. PLoS One. 2016;11(4):e0151822.
Gallone G, Baldetti L, Tzanis G, Gramegna M, Latib A, Colombo A, et al. Refractory angina: from pathophysiology to new therapeutic nonpharmacological technologies. JACC Cardiovasc Interv. 2020;13(1):1–19.
Khan AR, Farid TA, Pathan A, Tripathi A, Ghafghazi S, Wysoczynski M, et al. Impact of cell therapy on myocardial perfusion and cardiovascular outcomes in patients with angina refractory to medical therapy: a systematic review and meta-analysis. Circ Res. 2016;118(6):984–93.
Henry TD, Losordo DW, Traverse JH, Schatz RA, Jolicoeur EM, Schaer GL, et al. Autologous CD34+ cell therapy improves exercise capacity, angina frequency and reduces mortality in no-option refractory angina: a patient-level pooled analysis of randomized double-blinded trials. Eur Heart J. 2018;39(23):2208–16.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Azzalini reports personal fees from Teleflex and Abiomed, outside the submitted work.
The other authors have no conflicts of interest to declare that are relevant to the content of this article.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Myocardial Disease
Rights and permissions
About this article
Cite this article
Moroni, F., Gertz, Z. & Azzalini, L. Relief of Ischemia in Ischemic Cardiomyopathy. Curr Cardiol Rep 23, 80 (2021). https://doi.org/10.1007/s11886-021-01520-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s11886-021-01520-4