Abstract
Introduction
This systematic review was performed to evaluate the results of transcatheter mitral valve implantation (TMVI) in the native mitral valve.
Evidence acquisition
Medline, EMBASE, and the Cochrane Central register were systematically searched for studies that reported results of TMVI in mitral valve regurgitation and/or stenosis and mitral annular calcification. To improve the sensitivity of the literature search, we performed citation chasing in Google Scholar, Scopus, and Web of Science.
Evidence synthesis
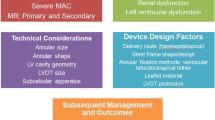
Twelve studies reporting results of TMVI in mitral regurgitation were retrieved and included 347 patients. The transseptal approach represented 28% of cases. Secondary mitral regurgitation was the predominant indication in 63% of cases. Thirty-day mortality was 11% and was lowered with the transseptal approach (7%). Technical success was 92%. Surgical conversion was needed in 5% of patients. Only one patient presented moderate to severe mitral regurgitation. These hemodynamic results were sustainable up to one year of follow-up. Three series focused on results of TMVI in mitral annulus calcification including 167 patients. Only nine patients were treated with TMVI dedicated prosthesis. Eighty-seven patients had their prosthesis delivered through a transseptal approach. Mitral stenosis was present in 63% of cases. Thirty-day mortality was 24%, and none with TMVI prosthesis. Technical success was achieved in 71% of cases and was improved by using TMVI prosthesis (89%). The main complication was left ventricular outflow tract obstruction (20%). Post procedural moderate to severe mitral regurgitation was observed in 4% of cases.
Conclusion
TMVI seems to be feasible, achieving good technical success and predictable and durable MR reduction.




Similar content being viewed by others
Change history
03 April 2021
A Correction to this paper has been published: https://doi.org/10.1007/s11886-021-01502-6
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Coffey S, Cairns BJ, Iung B. The modern epidemiology of heart valve disease. Heart. 2016;102:75–85.
Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population- based study. Lancet. 2006;368:1005–11. https://doi.org/10.1016/S0140-6736(06)69208-8.
Mirabel M, Iung B, Baron G, et al. What are the characteristics of patients with severe, symptomatic, mitral regurgitation who are denied surgery? Eur Heart J. 2007;28:1358–65. https://doi.org/10.1093/eurheartj/ehm001.
Goel SS, Bajaj N, Aggarwal B, et al. Prevalence and outcomes of unoperated patients with severe symptomatic mitral regurgitation and heart failure: comprehensive analysis to determine the potential role of MitraClip for this unmet need. J Am Coll Cardiol. 2014;63:185–6.
•• Chiarito M, Pagnesi M, Martino EA, Pighi M, Scotti A, Biondi-Zoccai G, et al. Outcome after percutaneous edge-to-edge mitral repair for functional and degenerative mitral regurgitation: a systematic review and meta-analysis. Heart. 2018;104:306–12. A significant proportion of patients are considered to be suboptimal candidates for transcatheter mitral valve repair. Residual moderate or severe MR rates of up to 10% have been reported in this large meta-analysis of real-world patients undergoing transcatheter mitral valve repair. https://doi.org/10.1136/heartjnl-2017-311412.
Maisano F, Alfieri O, Banai S, et al. The future of transcatheter mitral valve interventions: competitive or complementary role of repair vs. replacement? Eur Heart J. 2015;36:1651–9. https://doi.org/10.1093/eurheartj/ehv123.
Korn D, Desanctis RW, Sell S. Massive calcification of the mitral annulus. A clinicopathological study of fourteen cases. N Engl J Med. 1962;267:900–9. https://doi.org/10.1056/NEJM196211012671802.
Fertman MH, Wolff L. Calcification of the mitral valve. Am Heart J. 1946;31:580–9. https://doi.org/10.1016/0002-8703(46)90004-X.
Okada Y. Surgical management of mitral annular calcification. Gen Thorac Cardiovasc Surg. 2013;61:619–25. https://doi.org/10.1007/s11748-013-0207-7.
Genoni M, Franzen D, Vogt P, Seifert B, Jenni R, Kunzli A, et al. Paravalvular leakage after mitral valve replace- ment: improved long-term survival with aggressive surgery? Eur J Cardiothorac Surg. 2000;17(1):14–9.
Deniz H, Sokullu O, Sanioglu S, Sargin M, Ozay B, Ayoglu U, et al. Risk factors for posterior ventricular rupture after mitral valve replacement: results of 2560 patients. Eur J Cardiothorac Surg. 2008;34(4):780–4.
Guerrero M, Dvir D, Himbert D, Urena M, Eleid M, Wang DD, et al. Transcatheter mitral valve replacement in native mitral valve disease with severe mitral annular calcification: results from the first multicenter global registry. JACC Cardiovasc Interv.63. 2016;9(13):1361–71.
Stroup D, Berlin J, Morton S, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) Group. JAMA. 2000;283:2008–12.
Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;g7647:349.
El Hajj SC, Eleid MF. Transcatheter mitral valve replacement: an update on the current literature. Curr Treat Options Cardiovasc Med. 2019;21(7):35.
Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27:1785–805. https://doi.org/10.1177/0962280216669183.
Wan X, Wang W, Liu J. TongT. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135.
Sterne JAC, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ. 2016;i4919:355.
Sorajja P, Moat N, Badhwar V, et al. Initial Feasibility Study of a New Transcatheter Mitral Prosthesis: The First 100 Patients. J Am Coll Cardiol. 2019;73(11):1250–60.
Cheung A. Latest updates from the world of TMVR: transapical Neovasc. Paper presented at: PCR London Valves. London, United Kingdom: 2019.
Bapat V, Rajagopal V, Meduri C, et al. Early experience with new transcatheter mitral valve replacement. J Am Coll Cardiol. 2018;71(1):12–21.
Piazza N. The HIGHLIFE Program: Attributes, Challenges, and Clinical Data. Paper presented at: The Structural Heart Disease Summit (SHDS). Chicago, IL: 2018.
Piazza N. Transcatheter mitral valve replacement: HighLife. Paper presented at: Transcatheter cardiovascular therapeutics (TCT). Denver, CO: 2017.
Regueiro A, Ye J, Fam N, Bapat VN, Dagenais F, Peterson MD, et al. 2-Year outcomes after transcatheter mitral valve replacement. JACC Cardiovasc Intervent. 2017;10:1671–8. https://doi.org/10.1016/j.jcin.2017.05.032.
Webb J. Latest updates from the world of TMVR: transseptal SAPIEN M3 TMVR. Paper presented at: PCR London Valves. London, United Kingdom: 2019, DOI: https://doi.org/10.3389/fnint.2019.00071.
Williams M. Latest updates from the world of TMVR: Caisson TMVR. Paper presented at: PCR London Valves. London: United Kingdom; 2019.
Asgar AW. Percutaneous Mitral Valve Replacement Technology Update. Paper presented at: Transcatheter cardiovascular therapeutics (TCT). San Francisco, CA: 2019, DOI: https://doi.org/10.1016/j.jcin.2020.11.022.
Webb J. Latest updates from the world of TMVR: transseptal Evoque TMVR. Paper presented at: PCR London Valves. London. In: United Kingdom; 2019. https://doi.org/10.3389/fnint.2019.00071.
Modine T. Latest updates from the world of TMVR: Cephea TMVR. Paper presented at: PCR London Valves. London: United Kingdom; 2019. https://doi.org/10.4244/EIJV15I7A103.
Maisano F. CardiovalveDevice Attributes, Implant Procedure and Early Results. Paper presented at: Transcatheter cardiovascular therapeutics (TCT). San Diego, CA: 2018, DOI: https://doi.org/10.4244/EIJ-D-18-00343.
Guerrero M, Vemulapalli S, Xiang Q, et al. Thirty-day outcomes of transcatheter mitral valve replacement for degenerated mitral bioprotheses (valve-in-valve), failed surgical rings (valve-in-ring), and native valve with severe mitral annular calcification (valve-in-mitral annular calcification) in the United States: data from the Society of Thoracic Surgeons/American College of Cardiology/Transcatheter Valve Therapy Registry. Circ Cardiovasc Interv. 2020;13(3):e008425.
Yoon SH, Whisenant BK, Bleiziffer S, et al. Outcomes of transcatheter mitral valve replacement for degenerated bioprostheses, failed annuloplasty rings, and mitral annular calcification. Eur Heart J. 2019;40(5):441–51. https://doi.org/10.1093/eurheartj/ehy590.
• Sorajja P, Gössl M, Babaliaros V, et al. Novel Transcatheter Mitral Valve Prosthesis for Patients With Severe Mitral Annular Calcification. J Am Coll Cardiol. 2019;74(11):1431–40. Transcatheter mitral valve replacement in severe mitral annular calcification with a dedicated prosthesis is feasible and can result in MR relief with symptom improvement.
• Coisne A, Pontana F, Tchétché D, et al. Transcatheter mitral valve replacement: factors associated with screening success and failure. EuroIntervention. 2019;15(11):e983–9. Anatomical issues remain the most important factor limiting the feasibility of TMVI. https://doi.org/10.4244/EIJ-D-19-00444.
Ribeiro HB, Nombela-Franco L, Muñoz-García AJ, et al. Predictors and impact of myocardial injury after transcatheter aortic valve replacement: a multicenter registry. J Am Coll Cardiol. 2015;66(19):2075–88.
Nishimura RA, Vahanian A, Eleid MF, Mack MJ. Mitral valve disease–current management and future challenges. Lancet. 2016;387:1324–34. https://doi.org/10.1016/S0140-6736(16)00558-4.
Stone GW, Lindenfeld J, Abraham WT, et al. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N Engl J Med. 2018;379(24):2307–18. https://doi.org/10.1056/NEJMoa1806640.
Lim D. Contemporary Outcomes with MitraClipTM (NTR/XTR) System in Primary Mitral Regurgitation: Results from the Global EXPAND Study. Paper presented at ACC.20/WCC virtual 2020, DOI: https://doi.org/10.4250/jcvi.2020.0154.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
Thomas Modine is a consultant for Boston Scientific, Medtronic, Edwards, Microport, GE, and Abbott; and he received a research support grant from Edwards. Darren Mylotte is a consultant for Medtronic, Boston Scientific, and Microport. Dr. Ralph Stephan von Bardeleben is a consultant for Abbott, Boston Scientific, Cardiac Dimensions, Edwards Lifesciences, and Medtronic. Walid Ben Ali, Reda Ibrahim, and Josep Rhodès declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Affiliations 1 and 3 contain some typos and Dr. Modine was not affiliated to 3.
This article is part of the Topical Collection on Structural Heart Disease
Rights and permissions
About this article
Cite this article
Ben-Ali, W., Ibrahim, R., Rodès-Cabeau, J. et al. Transcatheter Mitral Valve Implantation Systematic Review: Focus on Transseptal Approach and Mitral Annulus Calcification. Curr Cardiol Rep 23, 37 (2021). https://doi.org/10.1007/s11886-021-01466-7
Accepted:
Published:
DOI: https://doi.org/10.1007/s11886-021-01466-7