Abstract
Purpose of Review
Aging is associated with an increased prevalence of both cancer and heart disease. The progression of aortic valve calcification to aortic stenosis may be accelerated by both cardiovascular risk factors and cancer treatments, such as radiotherapy with mediastinal involvement. Symptomatic aortic stenosis is occasionally diagnosed in cancer patients undergoing cardiovascular evaluation; likewise, cancer is often recognized during assessment preceding aortic valve interventions. In these complex cases, physicians face difficult treatment decisions. Due to a myriad of clinical presentations of cancer and valve disease, specific guidelines for this patient population are not currently in place. Management is currently based on clinical judgment, on an individual basis.
Recent Findings
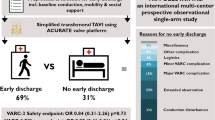
Patients with cancer in remission or with a favorable prognosis should be treated according to current cardiovascular guidelines. In these patients, aortic valve replacement can be performed either by surgery or transcatheter. Significant challenges arise in patients with active cancer, especially those receiving anti-cancer treatment. Recent data suggests that these patients can be offered aortic valve replacement, with a trend of favoring the transcatheter route in order to minimize perioperative risk and complications associated with major surgery. Patients with advanced cancer and severe aortic stenosis should be offered palliative care and can benefit from aortic balloon valvuloplasty if indicated. Modern cancer treatments associated with improved long-term prognosis may allow the appropriate cure of aortic stenosis.
Summary
We discuss the protocol, outcomes, and evolving recommendations of aortic valve replacement in cancer patients with aortic stenosis.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368(9540):1005–11.
Lindman B, Clavel M, Mathieu P, Lung P, Otto C, Pibarot P. Calcific aortic stenosis. Nat Rev. 2016;2:1–28.
Luise G, Lars A, George BBB, Philip M, Francesco M, Pepe Z, et al. Heart valve disease awareness survey 2017: what did we achieve since 2015? Clin Res Cardiol. 2018;108:61–7. https://doi.org/10.1007/s00392-018-1312-5.
Sengeløv M, Cheng S, Biering-Sørensen T, Matsushita K, Konety S, Solomon S, et al. Ideal cardiovascular health and the prevalence and severity of aortic stenosis in elderly patients. J Am Heart Assoc. 2018;7(3):e007234. https://doi.org/10.1161/JAHA.117.
Hemingway H, McCallum A, Shipley M, Manderbacka K, Martikainen P, Keskimaki I. Incidence and prognostic implications of stable angina pectoris among women and men. JAMA. 2006;295(12):1404–11.
Eyre H, Kahn R, Robertson R. ACS/ADA/AHA collaborative writing committee. Preventing cancer, cardiovascular disease, and diabetes: a common agenda for the American Cancer Society, the American Diabetes Association, and the American Heart Association. CA Cancer J Clin. 2004;54(4):190–207.
Rasmussen-Torvik L, Shay C, Abramson J, Friedrich C, Nettleton J, Prizment A, et al. Ideal cardiovascular health is inversely associated with incident cancer: the atherosclerosis risk in communities study. Circulation. 2013;127:1270–5.
Giza DE, Iliescu G, Hassan S, Marmagkiolis K, Iliescu C. Cancer as a risk factor for cardiovascular disease. Curr Oncol Rep. 2017;19(6):39.
Liu VY, Agha AM, Lopez-Mattei J, Palaskas N, Kim P, Thompson K, et al. Interventional cardio-oncology: adding a new dimension to the cardio-oncology field. Front Cardiovasc Med. 2018;5:48.
Guha A, Armanious M, Fradley MG. Update on cardio-oncology: novel cancer therapeutics and associated cardiotoxicities. Trends Cardiovasc Med. 2018.
Hassan SA, Palaskas N, Kim P, Iliescu C, Lopez-Mattei J, Mouhayar E, et al. Chemotherapeutic agents and the risk of ischemia and arterial thrombosis. Curr Atheroscler Rep. 2018;20(2):10.
Leon M, Smith C, Mack M, Miller G, Moses J, Svensson L, et al. Transcatheter aortic-valve implantation for aortic stenosis in patient who cannot undergo surgery. The New England journal of medicine, vol. 363; 2010. p. 1597–607.
Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med. 2019.
Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O'Hair D, et al. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med. 2019.
Carrascal Y, Gualis J, Arevalo A, Fulquet E, Florez S, Rey J, et al. Cardiac surgery with extracorporeal circulation in cancer patients: influence on surgical morbidity and mortality and on survival. Rev Esp Cardiol. 2008;61(4):369–75.
•• Yusuf SW, Sarfaraz A, Durand JB, Swafford J, Daher IN. Management and outcomes of severe aortic stenosis in cancer patients. Am Heart J. 2011;161(6):1125–32 This study is one of the first to support aortic valve replacement and demonstrate improved outcomes in cancer patients with severe aortic stenosis.
Wu W, Masri A, Popovic ZB, Smedira NG, Lytle BW, Marwick TH, et al. Long-term survival of patients with radiation heart disease undergoing cardiac surgery: a cohort study. Circulation. 2013;127(14):1476–85.
Dijos M, Reynaud A, Leroux L, Reant P, Cornolle C, Roudaut R, et al. Efficacy and follow-up of transcatheter aortic valve implantation in patients with radiation-induced aortic stenosis. Open Heart. 2015;2(1):e000252.
Paven E, Cimadevilla C, Urena M, Dilly MP, Nataf P, Raffoul R, et al. Management of radiation-induced valvular heart disease due to Hodgkin’s Lymphoma in the modern era. EuroIntervention. 2018;13(15):e1771–e3.
Sari C, Ayhan H, Bastug S, Kasapkara HA, Karaduman BD, Aslan AN, et al. Transcatheter aortic valve implantation in the presence of hematologic malignancies. Turk Kardiyol Dern Ars. 2015;43(6):529–35.
Watanabe Y, Kozuma K, Hioki H, Kawashima H, Nara Y, Kataoka A, et al. Comparison of results of transcatheter aortic valve implantation in patients with versus without active cancer. Am J Cardiol. 2016;118(4):572–7.
Berkovitch A, Guetta V, Barbash IM, Fink N, Regev E, Maor E, et al. Favorable short-term and long-term outcomes among patients with prior history of malignancy undergoing transcatheter aortic valve implantation. J Invasive Cardiol. 2018;30(3):105–9.
Donnellan E, Griffin BP, Johnston DR, Popovic ZB, Alashi A, Kapadia SR, et al. Rate of progression of aortic stenosis and its impact on outcomes in patients with radiation-associated cardiac disease: a matched cohort study. JACC Cardiovasc Imaging. 2018. https://doi.org/10.1016/j.jcmg.2018.04.019.
Mangner N, Woitek FJ, Haussig S, Holzhey D, Stachel G, Schlotter F, et al. Impact of active cancer disease on the outcome of patients undergoing transcatheter aortic valve replacement. J Interv Cardiol. 2018;31(2):188–96.
• Minamino-Muta E, Kato T, Morimoto T, Taniguchi T, Nakatsuma K, Kimura Y, et al. Malignant disease as a comorbidity in patients with severe aortic stenosis: clinical presentation, outcomes, and management. Eur Heart J Qual Care Clin Outcomes. 2018;4(3):180–8 This paper presents one of the largest analyses of clinical data, outcomes, and management of severe aortic stenosis in cancer patients.
Schechter M, Balanescu DV, Donisan T, Dayah TJ, Kar B, Gregoric I, et al. An update on the management and outcomes of cancer patients with severe aortic stenosis. Catheter Cardiovasc Interv. 2018.
•• Landes U, Iakobishvili Z, Vronsky D, Zusman O, Barsheshet A, Jaffe R, et al. Transcatheter aortic valve replacement in oncology patients with severe aortic stenosis. JACC Cardiovasc Interv. 2019;12(1):78–86 This pivotal study presents data from a large TAVR registry and is one of the largest analyses of TAVR outcomes in cancer patients.
Faggiano P, Frattini S, Zilioli V, Rossi A, Nistri S, Dini FL, et al. Prevalence of comorbidities and associated cardiac diseases in patients with valve aortic stenosis. Potential implications for the decision-making process. Int J Cardiol. 2012;159(2):94–9.
Okura Y, Ishigaki S, Sakakibara S, Yumoto C, Hashitate M, Sekine C, et al. Prognosis of cancer patients with aortic stenosis under optimal cancer therapies and conservative cardiac treatments. Int Heart J. 2018;6:750–8. https://doi.org/10.1536/ihj.17-320.
Ong DS, Aertker RA, Clark AN, Kiefer T, Hughes GC, Harrison JK, et al. Radiation-associated valvular heart disease. J Heart Valve Dis. 2013;22(6):883–92.
Marmagkiolis K, Finch W, Tsitlakidou D, Josephs T, Iliescu C, Best JF, et al. Radiation toxicity to the cardiovascular system. Curr Oncol Rep. 2016;18(3):15.
Yusuf SW, Howell RM, Gomez D, Pinnix CC, Iliescu CA, Banchs J. Radiation-related heart and vascular disease. Future Oncol. 2015;11(14):2067–76.
Chang HM, Okwuosa TM, Scarabelli T, Moudgil R, Yeh ETH. Cardiovascular complications of cancer therapy: best practices in diagnosis, prevention, and management: part 2. J Am Coll Cardiol. 2017;70(20):2552–65.
Nadlonek NA, Weyant MJ, Yu JA, Cleveland JC Jr, Reece TB, Meng X, et al. Radiation induces osteogenesis in human aortic valve interstitial cells. J Thorac Cardiovasc Surg. 2012;144(6):1466–70.
Beohar N, Kirtane AJ, Blackstone E, Waksman R, Holmes D Jr, Minha S, et al. Trends in complications and outcomes of patients undergoing transfemoral transcatheter aortic valve replacement: Experience From the PARTNER Continued Access Registry. JACC Cardiovasc Interv. 2016;9(4):355–63.
Latib A, Montorfano M, Figini F, Maisano F, Chieffo A, Benussi S, et al. Percutaneous valve replacement in a young adult for radiation-induced aortic stenosis. J Cardiovasc Med (Hagerstown). 2012;13(6):397–8.
Gujral DM, Lloyd G, Bhattacharyya S. Radiation-induced valvular heart disease. Heart. 2016;102(4):269–76.
Taylor CW, Wang Z, Macaulay E, Jagsi R, Duane F, Darby SC. Exposure of the heart in breast cancer radiation therapy: a systematic review of heart doses published during 2003 to 2013. Int J Radiat Oncol Biol Phys. 2015;93(4):845–53.
Boekel NB, Jacobse JN, Schaapveld M, Hooning MJ, Gietema JA, Duane FK, et al. Cardiovascular disease incidence after internal mammary chain irradiation and anthracycline-based chemotherapy for breast cancer. Br J Cancer. 2018;119:408–18.
Ben-Dor I, Waksman R, Hann N, Raizon A, Satler L, Torguson R, et al. Utility of radiologic review for noncardiac findings on multislice computed tomography in patients with severe aortic stenosis evaluated for transcatheter aortic valve implantation. Am J Cardiol. 2010;105:1461–4.
Gufler H, Schulze C, Wagner S. Incidental findings in computed tomographic angiography for planning percutaneous aortic valve replacement: advanced age, increased cancer prevalence? Acta Radiol. 2014;55(4):420–6.
Schmidt LH, Vietmeier B, Kaleschke G, Schulke C, Gorlich D, Schliemann C, et al. Thoracic malignancies and pulmonary nodules in patients under evaluation for transcatheter aortic valve implantation (TAVI): incidence, follow up and possible impact on treatment decision. PLoS One. 2016;11(5):e0155398.
Lee HY, Kim SM, Lee KS, Park SW, Chung MJ, Cho H, et al. Quantification of aortic valve calcifications detected during lung cancer-screening CT helps stratify subjects necessitating echocardiography for aortic stenosis diagnosis. Medicine (Baltimore). 2016;95(19):e3710.
Sablotzki A, Welters I, Lehmann N, Menges T, Gorlach G, et al. Plasma levels of immunoinhibitory cytokine interleukin-10 and transforming growth factor-β in patients undergoing coronary artery bypass grafting. Eur J Cardio Thorac Surg. 1997;11(4):763–8.
Akbas H, Erdal A, Demiralp E, Alp M. Effects of coronary artery bypass grafting on cellular immunity with or without cardiopulmonary bypass. Cardiovasc Surg. 2002;10:586–9.
Voets A, Joesoef K, van Teeffelen M. The influence of open heart surgery on survival of patients with co-existent surgically amenable lung cancer (stage I and II). Eur J Cardiothorac Surg. 1997;12:898–902.
Suzuki S, Usui A, Yoshida K, Matsuura A, Ichihara T, Ueda Y. Effect of cardiopulmonary bypass on cancer prognosis. Asian Cardiovasc Thorac Ann. 2010;18:536–40.
Plumereau F, Pinaud F, Roch A, Baufreton C. Do patients with haematological malignancy who need cardiopulmonary bypass have a short-term higher mortality or a higher chance of disease progression? Interact Cardiovasc Thorac Surg. 2014;19(3):474–8.
Nguyen HG, Tilki D, Dall'Era MA, Durbin-Johnson B, Carballido JA, Chandrasekar T, et al. Cardiopulmonary bypass has no significant impact on survival in patients undergoing nephrectomy and level III-IV inferior vena cava thrombectomy: multi-institutional analysis. J Urol. 2015;194(2):304–8.
Pinto CA, Marcella S, August DA, Holland B, Kostis JB, Demissie K. Cardiopulmonary bypass has a modest association with cancer progression: a retrospective cohort study. BMC Cancer. 2013;13:519.
Szeto WY, Svensson LG, Rajeswaran J, Ehrlinger J, Suri RM, Smith CR, et al. Appropriate patient selection or health care rationing? Lessons from surgical aortic valve replacement in the placement of aortic transcatheter valves I trial. J Thorac Cardiovasc Surg. 2015;150(3):557–68.e11.
Mrak M, Ambrozic J, Music S, Terseglav S, Kontestabile B, Lakic N, et al. Transcatheter aortic valve implantation in a cancer patient denied for surgical aortic valve replacement-a case report. Wien Klin Wochenschr. 2016;128(13–14):516–20.
Komatsu H, Izumi N, Tsukioka T, Chung K, Toda M, Hara K, et al. Pulmonary resection for lung cancer following transcatheter aortic valve implantation for severe aortic valve stenosis: a case report. Ann Thorac Cardiovasc Surg. 2018. https://doi.org/10.5761/atcs.cr.18-00028.
Drevet G, Maury JM, Farhat F, Tronc F. Transcatheter aortic valve implantation: a safe and efficient procedure to treat an aortic valve stenosis before lung cancer resection. Gen Thorac Cardiovasc Surg. 2018.
Sakai T, Yahagi K, Miura S, Hoshino T, Yokota T, Tanabe K, et al. Transcatheter aortic valve implantation for patients with lung cancer and aortic valve stenosis. J Thorac Dis. 2018;10(5):E387–e90.
Kogoj P, Devjak R, Bunc M. Balloon aortic valvuloplasty (BAV) as a bridge to aortic valve replacement in cancer patients who require urgent non-cardiac surgery. Radiol Oncol. 2014;48(1):62–6.
Puri R, Iung B, Cohen DJ, Rodes-Cabau J. TAVI or No TAVI: identifying patients unlikely to benefit from transcatheter aortic valve implantation. Eur Heart J. 2016;37(28):2217–25.
Chakravarty T, Sondergaard L, Friedman J, De Backer O, Berman D, Kofoed KF, et al. Subclinical leaflet thrombosis in surgical and transcatheter bioprosthetic aortic valves: an observational study. Lancet. 2017;389(10087):2383–92.
Hansson NC, Grove EL, Andersen HR, Leipsic J, Mathiassen ON, Jensen JM, et al. Transcatheter aortic valve thrombosis: incidence, predisposing factors, and clinical implications. J Am Coll Cardiol. 2016;68(19):2059–69.
Leroux L, Dijos M, Peltan J, Casassus F, Seguy B, Natsumeda M, et al. Lethal aorto-right ventricular defect after transcatheter aortic valve implantation in a patient with radiation-induced porcelain aorta: notes of caution. Can J Cardiol. 2016;32(1):135.e9–e11.
Iliescu CA, Grines CL, Herrmann J, Yang EH, Cilingiroglu M, Charitakis K, et al. SCAI expert consensus statement: evaluation, management, and special considerations of cardio-oncology patients in the cardiac catheterization laboratory (endorsed by the cardiological society of India, and sociedad Latino Americana de Cardiologia intervencionista). Catheter Cardiovasc Interv. 2016;87(5):E202–23.
Rodriguez-Manas L, Feart C, Mann G, Vina J, Chatterji S, Chodzko-Zajko W, et al. Searching for an operational definition of frailty: a Delphi method based consensus statement: the frailty operative definition-consensus conference project. J Gerontol A Biol Sci Med Sci. 2013;68(1):62–7.
Handforth C, Clegg A, Young C, Simpkins S, Seymour MT, Selby PJ, et al. The prevalence and outcomes of frailty in older cancer patients: a systematic review. Ann Oncol. 2015;26(6):1091–101.
Ness KK, Armstrong GT, Kundu M, Wilson CL, Tchkonia T, Kirkland JL. Frailty in childhood cancer survivors. Cancer. 2015;121(10):1540–7.
Kim DH, Kim CA, Placide S, Lipsitz LA, Marcantonio ER. Preoperative frailty assessment and outcomes at 6 months or later in older adults undergoing cardiac surgical procedures: a systematic review. Ann Intern Med. 2016;165(9):650–60.
Talbot-Hamon C, Afilalo J. Transcatheter aortic valve replacement in the care of older persons with aortic stenosis. J Am Geriatr Soc. 2017;65(4):693–8.
Afilalo J, Lauck S, Kim DH, Lefevre T, Piazza N, Lachapelle K, et al. Frailty in older adults undergoing aortic valve replacement: the FRAILTY-AVR study. J Am Coll Cardiol. 2017;70(6):689–700.
Hebeler KR, Baumgarten H, Squiers JJ, Wooley J, Pollock BD, Mahoney C, et al. Albumin is predictive of 1-year mortality after transcatheter aortic valve replacement. Ann Thorac Surg. 2018;106:1302–7.
Baumgartner H, Volkmar Falk V, Bax J, De Bonis M, Hamm C, Johan P, et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017;38:2739–91.
Nishimura R, Otto C, Bonow R, Carabello B, Erwin J, Fleisher L, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease. J Am Coll Cardiol. 2017;70:252–89.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Serban Mihai Balanescu, Dinu Valentin Balanescu, Teodora Donisan, Eric H. Yang, Nicolas Palaskas, Juan Lopez-Mattei, Saamir Hassan, Peter Kim, Mehmet Cilingiroglu, Konstantinos Marmagkiolis, Biswajit Kar, and Cezar Iliescu declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardio-Oncology
Rights and permissions
About this article
Cite this article
Balanescu, S.M., Balanescu, D.V., Donisan, T. et al. The Onco-cardiologist Dilemma: to Implant, to Defer, or to Avoid Transcatheter Aortic Valve Replacement in Cancer Patients with Aortic Stenosis?. Curr Cardiol Rep 21, 83 (2019). https://doi.org/10.1007/s11886-019-1166-0
Published:
DOI: https://doi.org/10.1007/s11886-019-1166-0