Abstract
Direct thrombin inhibitors (DTIs) are a new class of therapeutics possessing theoretic advantages over unfractionated heparin (UFH). In contrast to UFH, DTIs do not activate platelets, have no circulating inhibitors, and bind to both free and clot-bound thrombin. These theoretical advantages have spurred clinical trials investigating DTIs in a variety of cardiovascular indications. Currently, the major role for DTIs in cardiology is as an adjunct during percutaneous coronary intervention (PCI). Such a role stems from the results of the Randomized Evaluation in PCI Linking Angiomax to Reduced Clinical Events (REPLACE)-2 randomized trial, in which bivalirudin with provisional abciximab was demonstrated to be equivalent to UFH plus planned abciximab with respect to ischemic endpoints, while being associated with less bleeding. Ongoing clinical trials will define the role of bivalirudin as an adjunct to primary PCI for ST-segment elevation myocardial infarction and in non-ST segment elevation acute coronary syndrome as an adjunct to an early invasive strategy.
Similar content being viewed by others
References and Recommended Reading
Serruys PW, Herrman JP, Simon R, et al.: A comparison of hirudin with heparin in the prevention of restenosis after coronary angioplasty. Helvetica Investigators. N Engl J Med 1995, 333:757–763.
Bittl JA, Strony J, Brinker JA, et al.: Treatment with bivalirudin (Hirulog) as compared with heparin during coronary angioplasty for unstable or postinfarction angina. Hirulog Angioplasty Study Investigators. N Engl J Med 1995, 333:764–769.
Bittl JA, Chaitman BR, Feit F, et al.: Bivalirudin versus heparin during coronary angioplasty for unstable or postinfarction angina: Final report reanalysis of the Bivalirudin Angioplasty Study. Am Heart J 2001, 142:952–959.
Lincoff AM, Kleiman NS, Kottke-Marchant K, et al.: Bivalirudin with planned or provisional abciximab versus low-dose heparin and abciximab during percutaneous coronary revascularization: results of the Comparison of Abciximab Complications with Hirulog for Ischemic Events Trial (CACHET). Am Heart J 2002, 143:847–853.
Lincoff AM, Bittl JA, Kleiman NS, et al.: Comparison of bivalirudin versus heparin during percutaneous coronary intervention (the Randomized Evaluation of PCI Linking Angiomax to Reduced Clinical Events [REPLACE]-1 trial). Am J Cardiol 2004, 93:1092–1096.
Lincoff AM, Bittl JA, Harrington RA, et al.: Bivalirudin and provisional glycoprotein IIb/IIIa blockade compared with heparin and planned glycoprotein IIb/IIIa blockade during percutaneous coronary intervention: REPLACE-2 randomized trial. JAMA 2003, 289:853–863. This landmark trial definitively demonstrated the equivalence of bivalirudin with provisional abciximab as compared with UFH with planned abciximab during PCI. Bivalirudin was also associated with less bleeding.
Lincoff AM, Kleiman NS, Kereiakes DJ, et al.: Long-term efficacy of bivalirudin and provisional glycoprotein IIb/IIIa blockade vs heparin and planned glycoprotein IIb/IIIa blockade during percutaneous coronary revascularization: REPLACE-2 randomized trial. JAMA 2004, 292:696–703. This analysis of REPLACE-2 demonstrated the long-term equivalence of bivalirudin as compared with UFH with GP IIb/IIIa inhibitors during PCI.
Cohen DJ, Lincoff AM, Lavelle TA, et al.: Economic evaluation of bivalirudin with provisional glycoprotein IIB/IIIA inhibition versus heparin with routine glycoprotein IIB/IIIA inhibition for percutaneous coronary intervention: results from the REPLACE-2 trial. J Am Coll Cardiol 2004, 44:1792–1800.
Dangas GD, Lasic Z, Mehran R, et al.: Bivalirudin is a safe replacement to heparin during percutaneous coronary intervention with drug-eluting stents: final results of the multicenter ADEST study. Am J Cardiol 2004, 94(Suppl 6A):37E.
A comparison of recombinant hirudin with heparin for the treatment of acute coronary syndromes. The Global Use of Strategies to Open Occluded Coronary Arteries (GUSTO) IIb investigators. N Engl J Med 1996, 335:775–782.
Effects of recombinant hirudin (lepirudin) compared with heparin on death, myocardial infarction, refractory angina, and revascularisation procedures in patients with acute myocardial ischaemia without ST elevation: a randomised trial. Organisation to Assess Strategies for Ischemic Syndromes (OASIS-2) Investigators. Lancet 1999, 353:429–438.
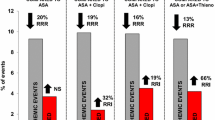
Direct thrombin inhibitors in acute coronary syndromes: principal results of a meta-analysis based on individual patients' data. Lancet 2002, 359:294–302. This meta-analysis of 35,970 patients from 11 randomized trials provides the most comprehensive analysis of DTIs in ACS.
Cannon CP, Weintraub WS, Demopoulos LA, et al.: Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glycoprotein IIb/ IIIa inhibitor tirofiban. N Engl J Med 2001, 344:1879–1887.
Comparison of angiomax versus heparin in acute coronary syndromes. http://www.clinicaltrials.gov/ct/gui/show/ NCT00093158
Randomized trial of intravenous heparin versus recombinant hirudin for acute coronary syndromes. The Global Use of Strategies to Open Occluded Coronary Arteries (GUSTO) IIa Investigators. Circulation 1994, 90:1631–1637.
Neuhaus KL, von Essen R, Tebbe U, et al.: Safety observations from the pilot phase of the randomized r-Hirudin for Improvement of Thrombolysis (HIT-III) study. A study of the Arbeitsgemeinschaft Leitender Kardiologischer Krankenhausarzte (ALKK). Circulation 1994, 90:1638–1642.
Antman EM: Hirudin in acute myocardial infarction. Safety report from the Thrombolysis and Thrombin Inhibition in Myocardial Infarction (TIMI) 9A Trial. Circulation 1994, 90:1624–1630.
Antman EM: Hirudin in acute myocardial infarction. Thrombolysis and Thrombin Inhibition in Myocardial Infarction (TIMI) 9B trial. Circulation 1996, 94:911–921.
White H: Thrombin-specific anticoagulation with bivalirudin versus heparin in patients receiving fibrinolytic therapy for acute myocardial infarction: the HERO-2 randomised trial. Lancet 2001, 358:1855–1863. This large randomized trial assessed the efficacy and safety of bivalirudin as an adjunct to thrombolytics in STEMI.
Keeley EC, Boura JA, Grines CL: Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 2003, 361:13–20.
Cardiovascular Research Foundation News. http://www.crf.org/news.html
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Chen, M.S., Lincoff, A.M. Direct thrombin inhibitors. Curr Cardiol Rep 7, 255–259 (2005). https://doi.org/10.1007/s11886-005-0046-y
Issue Date:
DOI: https://doi.org/10.1007/s11886-005-0046-y