Abstract
Purpose of Review
The aim of this paper is to provide an update on the classification of urethral syndrome and explore some of the current hypotheses and management options for patients suffering from this common condition.
Recent Findings
Ever since urethral syndrome was first reported in the mid-twentieth century, there has been much mystery and confusion around this condition. This was primarily due to lack of clear definitions and limited understanding of its aetiology and pathogenesis.
Summary
Recent advances have led to a paradigm shift, resulting in urethral syndrome no longer being seen as a condition in itself but as part of the spectrum of chronic pelvic pain syndromes.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Gallagher DJA, Montgomerie JZ, North JDK. Acute infections of the urinary tract and urethral syndrome in general practice. Br Med J. 1965;1:622–6.
Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology in lower urinary tract function: report from the Standardisation Sub-Committee of the International Continence Society. Urology. 2003;61:37–49.
•• Doggweiler R, Whitmore KE, Meijlink JM, et al. A standard for terminology in chronic pelvic pain syndromes: a report from the Chronic Pelvic Pain Working Group of the International Continence Society. Neurourol Urodyn. 2016;36(4):984–1008. Last year, the International Continence Society (ICS) published this paper to enable standardization of terms and clear definitions of conditions falling under the umbrella term of chronic pelvic pain syndromes (CPPS). Over the last two decades, there has been a shift away from the use of the term urethral syndrome/urethral pain syndrome reflecting the current paradigm that this symptom complex, rather than being a discreet entity, is in fact related to other pelvic syndromes
•• Engeler DS, Baranowski AP, Borovicka J et al. EAU guidelines on Chronic Pelvic Pain. Retrived from https://uroweb.org.uk/guideline/chronic-pelvic-pain/ Accessed date 20th May 2017. The European Association of Urology (EAU) guidelines provide clinicians with up to date (2016), evidence based information on the management of chronic pelvic pain syndromes, which includes urethral pain syndrome. They recommend a holistic and multi-modal approach with patient’ active participation.
Phillip H, Okewole I, Chilaka V. Enigma of urethral pain syndrome: why are there so many ascribed etiologies and therapeutic approaches? Int J Urol. 2014;21(6):544–8.
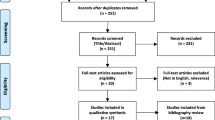
•• Hanno P, Dinis P, Lin A, et al. Bladder Pain Syndrome. In: Abrams P, Cardozo L, Khoury S, et al., editors. Incontinence. Paris: International Consultation on urological Diseases/European Association of Urology; 2013. p. 1583–649. Within this chapter in ‘Incontinence’, the ICS discuss the possible pathological processes behind chronic pain syndromes. Whilst there have been no significant advances in understanding the aetiology or pathogenesis of this condition, they provide a helpful algorithm (Figure 1) which illustrates the interplay between various factors and the pathways that may be involved.
Stamm WE, Wagner KF, Amsel R, et al. Causes of the acute urethral syndrome in women. N Engl J Med. 1980;303:409–15.
Brumfitt W, Hamilton-Miller JM, Gillespie WA. The mysterious ‘urethral syndrome’. BMJ. 1991;303(6793):1–2.
Maskell R, Pead L, Allan J. The puzzle of the ‘urethral syndrome’: a possible answer? Lancet. 1979;ii:1277–80.
Gillespie WA, Henderson EP, Linton KB, Smith PJB. Microbiology of the urethral syndrome. A controlled study with 5-year review. Br J Urol. 1989;64:270–4.
Duncan JL, Schaeffer AJ. Do infectious agents cause interstitial cystitis? Urology. 1997;49(5A Suppl):48–51.
Parsons CL. The role of a leaky epithelium and potassium in the generation of bladder symptoms in interstitial cystitis/overactive bladder, urethral syndrome, prostatitis ad gynaecological chronic pelvic pain. BJU Int. 2010;107:370–5.
Parsons CL, Rosenberg MT, Sassani P, Ebrahimi K, Kpziol JA, Zupkas P. Quantifying symptoms in men with interstitial cystitis/prostatitis, and its correlation with potassium-sensitivity testing. BJU Int. 2005;95:86–90.
Peeker R, Enerback L, Fall M, Aldenborg F. Recruitment, distribution and phenotypes of mast cells in interstitial cystitis. J Urol. 2000;163(3):1009–15.
Chaiken DC, Blaivas JG, Blaivas ST. Behavioural therapy for the treatment of refractory interstitial cystitis. J Urol. 1993;149(6):1445–8.
Parsons CL, Koprowski PF. Interstitial cystitis: successful management by increasing urinary voiding intervals. Urology. 1991;37(3):207–12.
Clemens JQ, Brown SO, Calhoun EA. Mental health diagnoses in patients with interstitial cystitis/painful bladder syndrome and chronic prostatitis/chronic pelvic pain syndrome: a case/control study. J Urol. 2008;180(4):1378–82.
Shorter B, Lesser M, Moldwin RM, Kushner L. Effecr of comestibles on symptoms of interstitial cystitis. J Urol. 2007;178(1):145–52.
Sasaki K, Smith CP, Chuang YC, Lee JY, Kim JC, Chancellor MB. Oral gabapentin (Neurontin) treatment of refractory genitourinary tract pain. Tech Urol. 2001;7(1):47–9.
Lee JW, Han DY, Jeong HJ. Bladder pain syndrome treated with triple therapy with gabapentin, amitriptyline, and a nonsteroidal anti-inflammatory drug. Int Neurourol J. 2010;14(4):256–60.
Kirkemo AK, Miles BJ, Peters JM. Use of amitriptyline in the treatment of interstitial cystitis. J Urology. 1990;143:279A.
Foster HE, Hanno PM, Nickel JC, Payne CK, Mayer RD, Burks DA, et al. Effect of amitriptyline on symptoms in treatment naïve patients with interstitial cystitis/painful bladder syndrome. J Urol. 2010;83(5):1853–8.
Hanno PM. Amitriptyline in the treatment of interstitial cystitis. Urol Clin North Am. 1994;21(1):89–91.
Burkhard FC, Blick N, Hochreiter WW, Studer UE. Urinary urgency and frequency, and chronic urethral and/or pelvic pain in females. Can doxycycline help? J Urol. 2004;172(1):232–5.
Warren JW, Home LM, Hebel JR, Marvel RP, Keay SK, Chai TC. Pilot study of sequential oral antibiotics for the treatment of interstitial cystitis. J Urol. 2000;163(6):1685–8.
Bernstein AM, Phillips HC, Linden W, Fenster H. A psychophysiological evaluation of female urethral syndrome: evidence for a muscular abnormality. J Behav Med. 1992;15:299–312.
Raz S, Smith RB. External sphincter spacticity syndrome in female pateints. J Urol. 1976;115:443–6.
Holm-Bentzen M, Jacobsen F, Nerstrom B, Lose G, Kristensen JK, Pedersen RH, et al. A prospective double-blind clinically controlled multicentre trial of sodium pentosanpolysulphate in the treatment of interstitial cystitis and related painful bladder disease. J Urol. 1987;138(3):503–7.
Mulholland SG, Hanno P, Parsons CL, Sant GR, Staskin DR. Pentosan polysulfate sodium for therapy of interstitial systitis. A double blind placebo-controlled clinical study. Urology. 1990;35(6):552–8.
Parsons CL, Benson G, Childs SJ, Hanno P, Sant GR, Webster G. A quantitatively controlled method to study prospectively interstitial cystitis and demonstrate the efficacy of pentosanpolysulfate. J Urol. 1993;150(3):845–8.
Youngblood VH, Tomlin EM, Davies JB. Senile urethritis in women. J Urol. 1957;78:150–2.
Fowler JE. Prospective study of intravesical dimethyl sulfocide in treatment of suspected early interstitial cystitis. Urology. 1981;18(1):21–6.
Perez-Marrero R, Emerson LE, Feltis JT. A controlled study of dimethyl sulfoxide in interstitial cystitis. J Urol. 1988;140(1):36–9.
Peeker R, Haghsheno MA, Holmang S, Fall M. Intravesical bacillus Calmette-Guerin and dimethyl sulfoxide for treatment of classic and nonulcer interstitial cystitis: a prospective randomised double blind study. J Urol. 2000;164(6):1912–5.
Rosamilia A, Dwyer PL, Gibson J. Electromotive drug administration of lidocaine and dexamethasone followed by cystodistension in women with interstitial cystitis. Int Urogynecol J Pelvic Floor Dynsfunct. 1997;8(3):142–5.
Masarani M, Willis RG. Urethral dilatation in women: urologists’ practice patterns in the UK. Ann R Coll Surg Engl. 2006;88(5):496–8.
Bergman A, Karram M, Bhatia NN. Urethral syndrome. A comparison of different treatment modalities. J Reprod Med. 1989;34(2):157–60.
Costantini E, Zucchi A, Del Zingaro M, Mearini L. Treatment of urethral syndrome: a prospective randomized study with Nd:YAG laser. Urol Int. 2006;76:134–8.
Rofeim O, Hom D, Freid RM, Moldwin RM. Use of the neodymium:YAG laser for interstitial cystitis: a prospective study. J Urol. 2001;166(1):134–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs Mistry, Reddy, Ni Raghallaigh and Emara declare they have no conflicts of interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Inflammatory/Infectious Bladder Disorders
Rights and permissions
About this article
Cite this article
Mistry, K., Reddy, U., Ni Raghallaigh, H. et al. Urethral Syndrome: Updates and Highlights on Current Management. Curr Bladder Dysfunct Rep 12, 354–360 (2017). https://doi.org/10.1007/s11884-017-0450-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-017-0450-3