Abstract
Purpose of review
Heart failure (HF) is one of the main causes of cardiovascular mortality in the western world. Despite great advances in treatment, recurrence and mortality rates remain high. Soluble guanylate cyclase is an enzyme which, by producing cGMP, is responsible for the effects of vasodilation, reduction of cardiac pre- and after-load and, therefore, the improvement of myocardial performance. Thus, a new therapeutic strategy is represented by the stimulators of soluble guanylate cyclase (sGCs). The aim of this meta-analysis was to analyze the effects deriving from the administration of sGCs, in subjects affected by HF.
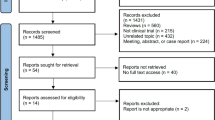
A systematic literature search of Medline, SCOPUS, and Google Scholar was conducted up to December 2022 to identify RCTs assessing the cardiovascular effects, as NT-pro-BNP values and ejection fraction (EF), and all-cause mortality, of the sGCs. Quantitative data synthesis was performed using a random-effects model, with weighted mean difference (WMD) and 95% confidence interval (CI) as summary statistics.
Recent findings
The results obtained documented a statistically significant improvement in NT-proBNP values (SMD: − 0.258; 95% CI: − 0.398, − 0.118; p < 0.001) and EF (WMD: 0.948; 95% CI: 0.485, 1.411; p < 0.001) in subjects treated with sGCs; however, no significant change was found in the all-cause mortality rate (RR 0.96; 95% CI 0.868 to 1.072; I2, p = 0).
Summary
The sGCs represent a valid therapeutic option in subjects suffering from HF, leading to an improvement in cardiac performance.






Similar content being viewed by others
Data Availability
The data are available upon request.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Aspromonte N, Gulizia MM, Di Lenarda A, et al. ANMCO/SIC Consensus Document: cardiology networks for outpatient heart failure care. Eur Heart J Suppl. 2017;19(Suppl D):D89–101.
Tavazzi L, Senni M, Metra M, et al. INHF (Italian Network on Heart Failure) Outcome Investigators. Multicenter prospective observational study on acute and chronic heart failure: one-year follow-up results of IN-HF (Italian Network on Heart Failure) outcome registry. Circ Heart Fail. 2013;6:473–81.
D’Elia E, Stamerra CA, Vecchi A, Duino V, Grosu A, Abete R, Baio P, Gori M, Gavazzi A, Ferri C, Senni M. Association between sleep disordered breathing, neurocognitive impairment and diastolic function in acute heart failure patients: an insight after the vulnerable phase of the hospitalization. Intern Emerg Med. 2021;16(2):369–77. https://doi.org/10.1007/s11739-020-02397-x.
Stamerra CA, D’Elia E, Gori M, Roncali F, Cereda A, Gavazzi A, Ferri C, Senni M. Red cell distribution width (RDW) is correlated to time of oxygen desaturation < 90% and length of sleep apneas in patients with sleep disorder breathing (SDB) and acute heart failure with preserved ejection fraction (HFpEF). Front Cardiovasc Med. 2023;3(10):1045702.
McDonagh TA, Metra M, Adamo M; ESC Scientific Document Group et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2021;42:3599–3726. The ESC guidelines represent the cornerstone of HF treatment.
Mebazaa A, Davison B, Chioncel O, Cohen-Solal A, Diaz R, Filippatos G, Metra M, Ponikowski P, Sliwa K, Voors AA, Edwards C, Novosadova M, Takagi K, Damasceno A, Saidu H, Gayat E, Pang PS, Celutkiene J, Cotter G. Safety, tolerability and efficacy of up-titration of guideline-directed medical therapies for acute heart failure (STRONG-HF): a multinational, open-label, randomised, trial. Lancet. 2022;400(10367):1938–52.
Bender AT, Beavo JA. Cyclic nucleotide phosphodiesterases: molecular regulation to clinical use. Pharmacol Rev. 2006;58:488–520.
Fesenko EE, Kolesnikov SS, Lyubarsky AL. Induction by cyclic GMP of cationic conductance in plasma membrane of retinal rod outer segment. Nature. 1985;313:310–3.
Krüger M, Kötter S, Grützner A, Lang P, Andresen C, Redfield MM, Butt E, dos Remedios CG, Linke WA. Protein kinase G modulates human myocardial passive stiffness by phosphorylation of the titin springs. Circ Res. 2009;104:87–94.
Kovács Á, Alogna A, Post H, Hamdani N. Is enhancing cGMP-PKG signalling a promising therapeutic target for heart failure with preserved ejection fraction? Neth Heart J. 2016;24:268–74.
Tsai EJ, Kass DA. Cyclic GMP signaling in cardiovascular pathophysiology and therapeutics. Pharmacol Ther. 2009;122:216–38.
Beuve A. Thiol-based redox modulation of soluble guanylyl cyclase, the nitric oxide receptor. Antioxid Redox Signal. 2017;26:137–49.
Sutton AJ, Abrams KR, Jones DR, Jones DR, Sheldon TA, Song F. Methods for meta-analysis in medical research: Wiley Chichester; 2000.
Borenstein M. Comprehensive meta‐analysis software. Systematic reviews in health research: meta‐analysis in context. 2022:535–48.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):1–10.
Sahebkar A, Serban C, Ursoniu S, Wong ND, Muntner P, Graham IM, Mikhailidis DP, Rizzo M, Rysz J, Sperling LS, Lip GY, Banach M. Lipid and Blood Pressure Meta-analysis Collaboration Group. Lack of efficacy of resveratrol on C-reactive protein and selected cardiovascular risk factors–Results from a systematic review and meta-analysis of randomized controlled trials. Int J Cardiol. 2015;189:47–55. https://doi.org/10.1016/j.ijcard.2015.04.008.
Sahebkar A. Effects of resveratrol supplementation on plasma lipids: a systematic review and meta-analysis of randomized controlled trials. Nutr Rev. 2013;71(12):822–35. https://doi.org/10.1111/nure.12081.
Duval S, Tweedie R. Trim and fill: a simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–63.
Dachs TM, Duca F, Rettl R, Binder-Rodriguez C, Dalos D, Ligios LC, et al. Riociguat in pulmonary hypertension and heart failure with preserved ejection fraction: the haemoDYNAMIC trial. Eur Heart J. 2022;43(36):3402–13.
Armstrong PW, Roessig L, Patel MJ, Anstrom KJ, Butler J, Voors AA, Lam CSP, Ponikowski P, Temple T, Pieske B, Ezekowitz J, Hernandez AF, Koglin J, O'Connor CM. (2018) A multicenter, randomized, double-blind, placebo-controlled trial of the efficacy and safety of the oral soluble guanylate cyclase stimulator: the VICTORIA trial. JACC Heart Fail 6(2):96–104. Based on the VICTORIA trials’ findings, vericiguat is currently recommended by both the European and American HF guidelines for HFrEF patients.
Armstrong PW, Lam CS, Anstrom KJ, Ezekowitz J, Hernandez AF, O’Connor CM, et al. Effect of vericiguat vs placebo on quality of life in patients with heart failure and preserved ejection fraction: the VITALITY-HFpEF randomized clinical trial. JAMA. 2020;324(15):1512–21.
Udelson JE, Lewis GD, Shah SJ, Zile MR, Redfield MM, Burnett J, et al. Effect of praliciguat on peak rate of oxygen consumption in patients with heart failure with preserved ejection fraction: the CAPACITY HFpEF randomized clinical trial. JAMA. 2020;324(15):1522–31.
Pieske B, Maggioni AP, Lam CS, Pieske-Kraigher E, Filippatos G, Butler J, et al. Vericiguat in patients with worsening chronic heart failure and preserved ejection fraction: results of the SOluble guanylate Cyclase stimulatoR in heArT failurE patientS with PRESERVED EF (SOCRATES-PRESERVED) study. Eur Heart J. 2017;38(15):1119–27.
Gheorghiade M, Greene SJ, Butler J, Filippatos G, Lam CS, Maggioni AP, et al. Effect of vericiguat, a soluble guanylate cyclase stimulator, on natriuretic peptide levels in patients with worsening chronic heart failure and reduced ejection fraction: the SOCRATES-REDUCED randomized trial. JAMA. 2015;314(21):2251–62.
Bonderman D, Pretsch I, Steringer-Mascherbauer R, Jansa P, Rosenkranz S, Tufaro C, et al. Acute hemodynamic effects of riociguat in patients with pulmonary hypertension associated with diastolic heart failure (DILATE-1): a randomized, double-blind, placebo-controlled, single-dose study. Chest. 2014;146(5):1274–85.
Ghofrani H-A, Galiè N, Grimminger F, Grünig E, Humbert M, Jing Z-C, et al. Riociguat for the treatment of pulmonary arterial hypertension. N Engl J Med. 2013;369(4):330–40.
Ghofrani H-A, D’Armini AM, Grimminger F, Hoeper MM, Jansa P, Kim NH, et al. Riociguat for the treatment of chronic thromboembolic pulmonary hypertension. N Engl J Med. 2013;369(4):319–29.
Bonderman D, Ghio S, Felix SB, Ghofrani H-A, Michelakis E, Mitrovic V, et al. Riociguat for patients with pulmonary hypertension caused by systolic left ventricular dysfunction: a phase IIb double-blind, randomized, placebo-controlled, dose-ranging hemodynamic study. Circulation. 2013;128(5):502–11.
Tran N, Garcia T, Aniqa M, Ali S, Ally A, Nauli SM. Endothelial Nitric Oxide Synthase (eNOS) and the Cardiovascular System: in Physiology and in disease states. Am J Biomed Sci Res. 2022;15(2):153–77.
Sharma R, Davidoff MN. Oxidative stress and endothelial dysfunction in heart failure. Congest Heart Fail. 2002;8(3):165–72. https://doi.org/10.1111/j.1527-5299.2002.00714.x.
Stamerra CA, Di Giosia P, Giorgini P, Ferri C, Sukhorukov VN, Sahebkar A. Mitochondrial dysfunction and cardiovascular disease: pathophysiology and emerging therapies. Oxid Med Cell Longev. 2022;2(2022):9530007.
Gianni D, Chan J, Gwathmey JK, Del Monte F, Hajjar RJ. SERCA2a in heart failure: role and therapeutic prospects. J Bioenerg Biomembr. 2005;37(6):375–80.
Franssen C, Chen S, Unger A, Korkmaz HI, De Keulenaer GW, Tschöpe C, et al. Myocardial microvascular inflammatory endothelial activation in heart failure with preserved ejection fraction. JACC Heart Fail. 2016;4(4):312–24.
van Heerebeek L, Hamdani N, Falcão-Pires I, Leite-Moreira AF, Begieneman MP, Bronzwaer JG, van der Velden J, Stienen GJ, Laarman GJ, Somsen A, Verheugt FW, Niessen HW, Paulus WJ. Low myocardial protein kinase G activity in heart failure with preserved ejection fraction. Circulation. 2012;126(7):830–9.
Gheorghiade M, Marti CN, Sabbah HN, Roessig L, Greene SJ, Böhm M, et al. Soluble guanylate cyclase: a potential therapeutic target for heart failure. Heart Fail Rev. 2013;18(2):123–34.
Schulz E, Jansen T, Wenzel P, Daiber A, Münzel T. Nitric oxide, tetrahydrobiopterin, oxidative stress and endothelial dysfunction in hypertension. Antioxid Redox Sig. 2008;10:1115–26.
Calderone A, Thaik CM, Takahashi N, Chang DL, Colucci WS. Nitric oxide, atrial natriuretic peptide, and cyclic GMP inhibit the growth promoting effects of norepinephrine in cardiac myocytes and fibroblasts. J Clin Invest. 1998;101:812–8.
Fiedler B, Lohmann SM, Smolenski A, Linnemuller S, Pieske B, Schroder F, Molkentin JD, Drexler H, Wollert KC. Inhibition of calcineurin-NFAT hypertrophy signaling by cGMP-dependent protein kinase type I in cardiac myocytes. Proc Natl Acad Sci U S A. 2002;99:11363–8.
Zhang M, Takimoto E, Hsu S, Lee DI, Nagayama T, Danner T, Koitabashi N, Barth AS, Bedja D, Gabrielson KL, Wang Y, Kass DA. Myocardial remodeling is controlled by myocyte-targeted gene regulation of phosphodiesterase type 5. J Am Coll Cardiol. 2010;56:2021–30.
Emdin M, Aimo A, Castiglione V, Vergaro G, Georgiopoulos G, Saccaro LF, et al. Targeting cyclic guanosine monophosphate to treat heart failure: JACC review topic of the week. J Am Coll Cardiol. 2020;76(15):1795–807.
Mercurio V, Ambrosio G, Correale M, Dini FL, Ghio S, Nodari S, et al. Innovations in medical therapy of heart failure with reduced ejection fraction. J Cardiovasc Med. 2023;24(Suppl 1):e47-54.
Irvine JC, Ganthavee V, Love JE, Alexander AE, Horowitz JD, Stasch JP, Kemp-Harper BK, Ritchie RH. The soluble guanylyl cyclase activator Bay 58–2667 selectively limits cardiomyocyte hypertrophy. PLoS ONE. 2012;7:e44481.
Masuyama H, Tsuruda T, Kato J, Imamura T, Asada Y, Stasch JP, Kitamura K, Eto T. Soluble guanylate cyclase stimulation on cardiovascular remodeling in angiotensin IIinduced hypertensive rats. Hypertension. 2006;48:972–8.
Masuyama H, Tsuruda T, Sekita Y, Hatakeyama K, Imamura T, Kato J, Asada Y, Stasch JP, Kitamura K. Pressure-independent effects of pharmacological stimulation of soluble guanylate cyclase on fibrosis in pressure-overloaded rat heart. Hypertens Res. 2009;32:597–603.
Sharkovska Y, Kalk P, Lawrenz B, Godes M, Hoffmann LS, Wellkisch K, Geschka S, Relle K, Hocher B, Stasch JP. Nitric oxide-independent stimulation of soluble guanylate cyclase reduces organ damage in experimental lowrenin and high-renin models. J Hypertens. 2010;28:1666–75.
Methner C, Buonincontri G, Hu CH, Vujic A, Kretschmer A, Sawiak S, Carpenter A, Stasch JP, Krieg T. Riociguat reduces infarct size and post-infarct heart failure in mouse hearts: insights from MRI/PET imaging. PLoS ONE. 2013;8:e83910. https://doi.org/10.1371/journal.pone.0083910.
Bice JS, Keim Y, Stasch JP, Baxter GF. NO-independent stimulation or activation of soluble guanylyl cyclase during early reperfusion limits infarct size. Cardiovasc Res. 2014;101(2):220–8. https://doi.org/10.1093/cvr/cvt257.
Matei AE, Beyer C, Györfi AH, Soare A, Chen CW, Dees C, Bergmann C, Ramming A, Friebe A, Hofmann F, et al. Protein kinases G are essential downstream mediators of the antifibrotic effects of sGC stimulators. Ann Rheum Dis. 2018;77:459.
Author information
Authors and Affiliations
Contributions
Authors' contributions: Conceptualization: CAS, AS Writing original draft: PDG, MG Writing review and editing: PG, TJ Approval of the final version: All authors
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stamerra, C.A., Di Giosia, P., Giorgini, P. et al. Cardiovascular Effects of Stimulators of Soluble Guanylate Cyclase Administration: A Meta-analysis of Randomized Controlled Trials. Curr Atheroscler Rep (2024). https://doi.org/10.1007/s11883-024-01197-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s11883-024-01197-4