Abstract
Purpose of Review
The purpose of this paper is to review allergic respiratory disease related to indoor and outdoor exposures and to examine the impact of known and projected changes in climate. The global burden of disease directly attributed to climate change is very difficult to measure and becomes more challenging when the capacity of humans to adapt to these changes is taken into consideration. Allergic respiratory disease, such as asthma, is quite heterogenous, though closely associated with environmental and consequently immunologic interaction. Where is the tipping point?
Recent Findings
Our climate has been measurably changing for the past 100 years. It may indeed be the most significant health threat of the twenty-first century, and consequently tackling climate change may be the greatest health opportunity. The impacts of climate change on human health are varied and coming more into focus. Direct effects, such as heatwaves, severe weather, drought, and flooding, are apparent and frequently in the news. Indirect or secondary effects, such as changes in ecosystems and the impact on health, are less obvious. It is these changes in ecosystems that may have the greatest impact on allergic and respiratory diseases.
Summary
This review will explore some ways that climate change, current and predicted, influences respiratory disease. Discussion will focus on changing pollen patterns, damp buildings with increased mold exposure, air pollution, and heat stress.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Watts N, Adger WN, Agnolucci P, Blackstock J, Byass P, Cai W, et al. Health and climate change: policy responses to protect public health. Lancet. 2015;386:1861–914.
•• Cubasch U, Wuebbles D, Chen D, Facchini MC, Frame D, Mahowald N, et al. Introduction. In: Stocker TF, Qin D, Plattner G-K, Tignor M, Allen SK, Boschung J, Nauels A, Xia Y, Bex V, Midgley PM, editors. Climate Change 2013: the physical science basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, United Kingdom and New York, NY, USA: Cambridge University Press; 2013.
•• Wuebbles DJ, Fahey DW, Hubbard KA, DeAngelo B, Doherty S, Hayhoe K, et al. Executive summary. In: Wuebbles DJ, Fahey DW, Hubbard KA, Dokken DJ, Stewart BC, Mavcock TK, editors. Climate Science Special Report: Fourth National Climate Assessment. Volume I. Washington, DC, USA.: U.S. Global Change Research Program; 2017. p. 12–34. https://doi.org/10.7930/J0DJ5RG.
•• Patz JA, Frumkin H, Holloway T, Vimont D, Haines A. Climate Change: challenges and opportunities for global health. JAMA. 2014;312(15):1565–80.
• D’Amato G, Vitale C, Lanza M, Molino A, D’Amato M. Climate change, air pollution and allergic respiratory diseases: an update. Curr Opin Allergy Clin Immunol. 2016;16(5):434–40.
Witt C, Schubert AJ, Jehn M, Holzgreve A, Liebers U, Endlicher W, Scherer d. The effects of climate change on patients with chronic lung disease. Dtsch Arztebl Int 2015; 112: 878–883.
Ziska LH, Gebhard DE, Frenz DA, Faulkner S, Singer BD, Straka JG. Cities as harbingers of climate change: common ragweed, urbanization, and public health. J Allergy Clin Immunol. 2003;111(2):290–5.
Ziska LH, Bunce JA, Goins EW. Characterization of an urban-rural CO2/temperature gradient and associated changes in initial plant productivity during secondary succession. Oecologia. 2004;139(3):454–8. Epub 2004 Mar 12
Singer BD, Ziska LH, Frenz DA, Gebhard DE, Straka JG. Increasing Amb a 1 content in ragweed pollen as a function of rising CO2 concentration. Func Plant Biol. 2005;32(US):667–70.
Wayne P, Foster S, Connolly J, Bazzaz F, Epstein P. Production of allergenic pollen by ragweed (Ambrosia artemisiifolia L.) is increased in CO2-enriched atmospheres. Ann Allergy Asthma Immunol. 2002;88:279–82.
Levetin E. Effects of climate change on airborne pollen. J Allergy Clin Immun . 2001;107:S172.
Rogers C, Wayne P, Macklin E, et al. Interaction of the onset of spring and elevated atmospheric CO2 on ragweed (Ambrosia artemisiifolia L.) pollen production. Environ Health Perspect. 2006;114:865–9.
• Ziska L, Knowlton K, Rogers C, Dalan D, Tierney N, Elder MA, et al. Recent warming by latitude associated with increased length of ragweed pollen season in central North America. Proc Natl Acad Sci. 2011;108(10):4248–51.
Ahlholm JU, Helander ML, Savolainen J. Genetic and environmental factors affecting the allergenicity of birch (Betula pubescens ssp. czerepanovii [Orl.] Hämet-ahti) pollen. Clin Exp Allergy. 1998;28(11):1384–8.
• Ariano R, Canonica GW, Passalacqua G. Possible role of climate changes in variations in pollen seasons and allergic sensitizations during 27 years. Ann Allergy Asthma Immunol. 2010;104(3):215–22. https://doi.org/10.1016/j.anai.2009.12.005.
U.S. Environmental Protection Agency. 2014. Climate change indicators in the United States, 2014. Third edition. EPA 430-R-14-004. Accessed at http://www.epa.gov/climatechange/indicators. Download on 4 December 2017.
•• Crimmins AJ, Balbus JL, Gamble CB, Beard JE, Bell D, Dodgen RJ, et al. The impacts of climate change on human health in the United States: a scientific assessment. Washington DC. US Global Res Prog. 2016;
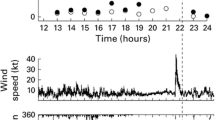
• D'Amato G, Vitale C, D'Amato M, Cecchi L, Liccardi G, Molino A, et al. Thunderstorm-related asthma: what happens and why. Clin Exp Allergy. 2016;46(3):390–6. https://doi.org/10.1111/cea.12709.
Bindoff N. "observations: oceanic climate change and sea level", climate change 2007: the physical science basis. Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge: Cambridge University Press; 2007.
Institute of Medicine. Clearing the air: asthma and indoor air exposures. Committee on the assessment of asthma and indoor air: national Acad Sci; 2000.
Barnes C, Alexis NE, Bernstein JA, Cohn JR, Demain JG, Horner E, et al. Climate change and our environment: the effect on respiratory and allergic disease. J Allergy Clin Immunol Pract. 2013;1(2):137–41.
Knutsen AP, Bush RK, Demain JG, Denning DW, Dixit A, Fairs A, Greenberger PA, Kariuki B, Kita H, Kurup VP, Moss RB, Niven RM, Pashley CH, Slavin RG, Vijay HM, Wardlaw AJ. Fungi and allergic lower respiratory tract diseases. J Allergy Clin Immunol 2012;129(2):280–291.
Fisk WJ, Lei-Gomez Q, Mendall MJ. Meta-analyses of the associations of respiratory health effects with dampness and mold in homes. Indoor Air. 2007;14:284–96.
U.S. Environmental Protection Agency. Health effects of Ozone in the general population. Washington DC: U.S. Environmental Protection Agency; 2017. Accessed at https://www.epa.gov/ozone-pollution/health-effects-ozone-pollution. Accessed December 8, 2017.
WHO, Air Quality Guidelines, Global Update 2005, particulate matter, ozone, nitrogen dioxide and sulfur dioxide. Germany, 2006, 480 pp.
D’Amato G, Vitale C, De Martino A, et al. Effects on asthma and respiratory allergy of climate change and air pollution. Multidicip Respir Med. 2015;10:39.
Beck I, Jochner S, Gilles S, McIntyre M, Buters JTM, Schmidt-Weber C, et al. High environmental ozone levels lead to enhanced allergenicity of birch pollen. PLoS One. 2013;8:e80147.
M J, Burnett RT, Pope CA 3rd, Ito K, Thurston G, Krewski D, et al. Long-term ozone exposure and mortality. N Engl J Med. 2009;360(11):1085–95.
McGeachie MJ, Yates KP, Zhou X, Guo F, Sternberg AL, Van Natta ML, et al. Patterns of growth and decline in lung function in persistent childhood asthma. N Engl J Med. 2016;374:1842–52.
McConnell R, Berhane K, Yao L, Jerrett M, Lurmann F, Gilliland F, et al. Traffic, susceptibility, and childhood asthma. Environ Health Perspect. 2006;114(5):766–72.
Gordian ME, Haneuse S, Wakefield J. An investigation of the association between traffic exposure and the diagnosis of asthma in children. J Expo Sci Environ Epidemiol 2006 Jan;16(1):49–55.
Jerrett M, Finkelstein MM, Brook JR, Arain MA, Kanaroglou P, Stieb DM, et al. A cohort study of traffic-related air pollution and mortality in Toronto, Ontario, Canada. Environ Health Perspect. 2009;117(5):772–7.
NASA Global Climate Change. Feature June 26, 2017. Accessed from: https://climate.nasa.gov/news/2602/lightning-sparking-more-boreal-forest-fires/. Accessed on December 8, 2017.
McMichael AJ. The urban environment and health in a world of increasing globalization: issues for developing countries. Bull World Health Organ. 2000;78(9):1117–26.
McCormack MC, Belli AJ, Waugh D, Matsui EC, Peng RD, Williams DL, et al. Respiratory Effects of Indoor Heat and the Interaction with Air Pollution in Chronic Obstructive Pulmonary Disease. Ann Am Thorac Soc. 2016;13(12):2125–31.
Lin S, Luo M, Walker RJ, Liu X, Hwang SA, Chinery R. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology. 2009;20(5):738–46.
• Sheehan WJ, Gaffin JM, Peden DB, Bush RK, Phipatanakul W. Advances in environmental and occupational disorders in 2016. J Allergy Clin Immunol. 2017;140(6):1683–92.
Centers for Disease Control and Prevention. National health interview survey data. Atlanta, GA. Centers for Disease Control and Prevention. https://www.cdc.gov/asthma/asthmadata.htm. Accessed December 8, 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Allergies and the Environment
Rights and permissions
About this article
Cite this article
Demain, J.G. Climate Change and the Impact on Respiratory and Allergic Disease: 2018. Curr Allergy Asthma Rep 18, 22 (2018). https://doi.org/10.1007/s11882-018-0777-7
Published:
DOI: https://doi.org/10.1007/s11882-018-0777-7