Abstract
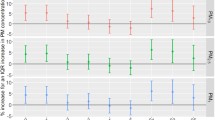
Multiple studies have noted an association between ambient air pollution and cardiovascular and pulmonary disease. Our goal was to investigate the potential relationship between fine particulate air pollution and emergency medical services (EMS) calls with a particular focus on cardiovascular and respiratory complaints. Utilizing a database of 911 emergency calls from the National EMS Information System, we analyzed 322,097 eligible EMS encounters in Utah over a 4-year period. We evaluated the relationship between the health emergency, as noted by the EMS provider’s primary impression, and short-term exposure to fine particulate matter (aerodynamic diameter ≤2.5-μm cut point (PM2.5)), as recorded by the United States Environmental Protection Agency (EPA) Air Quality System (AQS). Using a case crossover design and conditional logistic regression, we analyzed the association between health emergencies and PM2.5 concentrations over varying time exposures. At the 95 % confidence level, we found significant associations only between pollution exposure and EMS calls for diabetic symptoms (using pollution from the concurrent day) and syncope/fainting (using pollution from the concurrent day and from 2- to 5-day lagged moving averages). We found no other significant positive associations between health emergencies and PM2.5 concentration. In particular, we noted no association between daily PM2.5 concentration and EMS calls for cardiac arrest, chest pain, or respiratory distress. We found limited association between ambient air pollution and health emergencies, as classified by the EMS provider’s impression. We noted no association with primary cardiovascular or respiratory complaints.


Similar content being viewed by others
References
Atkinson R, Andreson H, Sunyer J, et al. (2001) Acute effects of particulate air pollution on respiratory admissions—results from APHEA 2 project. Am J Respir Crit Care Med. 164:1860–1866
Delfino RJ, Murphy-Moulton AM, Burnett RT, Brook JR, Becklake MR (1997) Effects of air pollution on emergency room visits for respiratory illnesses in Montreal, Quebec. Am J Respir Crit Care Med 155:568–576
Dennekamp M, Akram M, Abramson M, et al. (2010) Outdoor air pollution as a trigger for out-of-hospital cardiac arrests. Epidemiology 21(4):494–500
Dockery DW, Pope CA III (1994) Acute respiratory effects of particulate air pollution. Annu Rev Public Health 15:107–132
Ensor KB, Raun LH, Persse D (2013) A case-crossover analysis of out-of-hospital cardiac arrest and air pollution. Circulation 127:1192–1199
Janes H, Sheppard L, Lumley T (2005a) Case-crossover analyses of air pollution exposure data: referent selection strategies and their implications for bias. Epidemiology 16:717–726
Janes H, Sheppard L, Lumley T (2005b) Overlap bias in the case-crossover design, with application to air pollution exposures. Stat Med 24:285–300
Kan H, Jia J, Chen B (2003) Acute stroke mortality and air pollution: new evidence from Shanghai. China J Occup Health 45:321–323
Kettunen J et al. (2007) Associations of fine and ultrafine particulate air pollution with stroke mortality in an area of low air pollution levels. Stroke 38:918–992
Pope CA III (1989) Respiratory disease associated with community air pollution and a steel mill, Utah valley. Am J Public Health 79:623–628
Pope CA III (1991) Respiratory hospital admissions associated with PM10 pollution in Utah, Salt Lake, and Cache Valleys. Arch Environ Health 46:90–97
Pope CA III (1996) Particulate pollution and health: a review of the Utah valley experience. J Expo Anal Environ Epidemiol 6:23–34
Pope CA III, Dockery DW (1992) Acute health-effects of PM10 pollution on symptomatic and asymptomatic children. Am Rev Respir Dis 145:1123–1128
Pope CA III, Muhlestein J, May H, et al. (2006) Ischemic heart disease events triggered by short-term exposure to fine particulate air pollution. Circulation 114:2443–2448
Raza A, Bellander T, Bero-Bedada G, et al. (2014) Short-term effects of air pollution on out-of hospital cardiac arrest in Stockholm. Eur Heart J 35(13):861–868
Rosenthal F, Kuisma M, Lanki T, et al. (2013) Association of ozone and particulate air pollution with out-of hospital cardiac arrest in Helsinki, Finland: evidence for two different etiologies. J Expo Sci Environ Epidemiol 23:281–288
Samet JM, Speizer FE, Bishop Y, Spengler JD, Ferris BG (1981) The relationship between air-pollution and emergency room visits in an industrial community. J Air Pollut Control Assoc 31:236–240
Schwartz J, Salter D, Larson TV, Pierson WE, Koenig JQ. Particulate air pollution and hospital emergency room visits for asthma in Seattle. Am Rev Respir Dis 1993;147:826–833.
United States Environmental Protection Agency Technology Transfer Network (TTN) Air Quality System (AQS). Retrieved from http://www.epa.gov/ttn/airs/airsaqs/.
Wellenius GA, Schwartz J, Mittleman MA (2006) Particulate air pollution and hospital admissions for congestive heart failure in seven United States cities. Am J Cardiol 97:404–408
World Health Organization. Burden of disease from household air pollution 2012. Retrieved from http://www.who.int/phe/health_topics/outdoorair/databases/FINAL_HAP_AAP_BoD_24March2014.pdf?ua=1.
Zanobetti A, Schwartz J (2005) The effect of particulate air pollution on emergency admissions for myocardial infarction: a multicity case-crossover analysis. Environ Health Perspect 113:978–982
Zanobetti A, Franklin M, Koutrakis P, Schwartz J (2009) Fine particulate air pollution and its components in association with cause-specific emergency admissions. Environ Heal 8:58
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no competing interests.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Youngquist, S.T., Hood, C.H., Hales, N.M. et al. Association between EMS calls and fine particulate air pollution in Utah. Air Qual Atmos Health 9, 887–897 (2016). https://doi.org/10.1007/s11869-016-0392-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11869-016-0392-5