Abstract
Background
Smartwatches have gained tremendous attention in recent years and have become widely accepted by patients, despite not being intended for medical diagnosis.
Objective
This study aimed to determine the accuracy of Apple Watch oxygen saturation measurement in patients with acute exacerbation of COPD by comparing it with medical-grade pulse oximetry and ABG.
Method
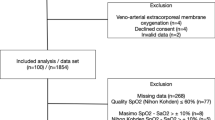
This single-center, prospective, cross-sectional study involved 167 patients. Patients presenting with cardiac arrest, life-threatening symptoms, severe hypoxia, or obvious jaundice were excluded. Additionally, patients whose SpO2 measurements with the Apple Watch took more than 2 min or required eight attempts were also excluded. Vital signs were measured simultaneously using the IntelliVue MX500 monitor with the Masimo Rainbow Set pulse oximeter and the Apple Watch. Concurrently, arterial blood gas (ABG) samples were drawn.
Results
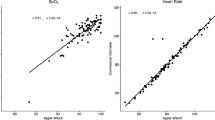
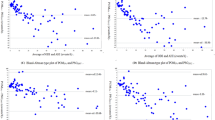
A strong correlation between the Apple Watch 6 and medical-grade pulse oximetry (r = 0.89, ICC = 0.940) was noted. The Bland-Altman analysis revealed a mean error of 0.458% between the Apple Watch 6 and ABG (SD: 2.78, level of agreement: − 5.912 to 4.996). The mean error between pulse oximetry and ABG (SD: 5.086, level of agreement; − 10.983 to 8.953) was 1.015%. There was a correlation between respiratory rate and the number of attempts to measure SpO2 with the Apple Watch 6 (r = 0.75, p < 0.05).
Conclusion
Apple Watch 6 is an accurate and reliable method for measuring SpO2 levels in emergency patients who presented with acute exacerbation of COPD. However, tachypneic patients may encounter challenges due to the potential need for multiple attempts to measure their oxygen saturation.




Similar content being viewed by others
Availability of data and materials
The datasets generated during the current study are available from the corresponding author.
Abbreviations
- ABG:
-
Arterial blood gas
- AF:
-
Atrial fibrillation
- COPD:
-
Chronic obstructive pulmonary disease.
- CHF:
-
Congestive heart failure
- ED:
-
Emergency department
- SpO2 :
-
Peripheral oxygen saturation
- SaO2 :
-
Arterial oxygen saturation
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- HR:
-
Heart rate
- HT:
-
Hypertension
- PaO2 :
-
Partial pressure of oxygen in the arterial blood
- RR:
-
Respiratory rate
- VBG:
-
Venous blood gas
References
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease. Updated 2019. Available from https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf. Accessed 25 Aug 2022
World Health Organization (2019) Chronic obstructive pulmonary disease (COPD). http://www.who.int/respiratory/copd/en/webcite
Rabe KF, Hurd S, Anzueto A et al (2007) Global strategy for the diagnosis, management, and prevention of COPD—2006 Update. Am J Respir Crit Care Med. Published online May 16. https://doi.org/10.1164/rccm.200703-456SO
Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease: 2019 Report (2019) Fontana, WI: Global Initiative for Chronic Obstructive Lung Disease (GOLD). https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdfwebcite. PubMed: 17507545
MacIntyre N, Huang YC (2008) Acute exacerbations and respiratory failure in chronic obstructive pulmonary disease. Proc Am Thorac Soc 5(4):530–535. https://doi.org/10.1513/pats.200707-088ET.PMID:18453367;PMCID:PMC2645331
Pauwels R, Calverley P, Buist AS et al (2004) COPD exacerbations: the importance of a standard definition. Respir Med 98(2):99–107. https://doi.org/10.1016/j.rmed.2003.09.001. PMID: 14971871
Shah SA, Velardo C, Farmer A, Tarassenko L (2017) Exacerbations in chronic obstructive pulmonary disease: identification and prediction using a digital health system. J Med Internet Res 19(3):e69. https://doi.org/10.2196/jmir.7207. PMID: 28270380; PMCID: PMC5360891
Pedone C, Chiurco D, Scarlata S, Incalzi RA (2013) Efficacy of multiparametric telemonitoring on respiratory outcomes in elderly people with COPD: a randomized controlled trial. BMC Health Serv Res 6(13):82. https://doi.org/10.1186/1472-6963-13-82. PMID: 23497109; PMCID: PMC3680224
Kent BD, Mitchell PD, McNicholas WT (2011) Hypoxemia in patients with COPD: cause, effects, and disease progression. Int J Chron Obstruct Pulmon Dis 6:199–208. https://doi.org/10.2147/COPD.S10611. Epub 2011 Mar 14. PMID: 21660297; PMCID: PMC3107696
Plüddemann A, Thompson M, Heneghan C, Price C (2011) Pulse oximetry in primary care: primary care diagnostic technology update. Br J Gen Pract 61(586):358–359. https://doi.org/10.3399/bjgp11X572553. PMID: 21619771; PMCID: PMC3080222
Jubran A (1999) Pulse oximetry. Crit Care 3(2):R11–R17. https://doi.org/10.1186/cc341. PMID: 11094477; PMCID: PMC137227
Lee H, Ko H, Lee J (2016) Reflectance pulse oximetry: practical issues and limitations. ICT Exp 2(4):195–198. ISSN 2405–9595. https://doi.org/10.1016/j.icte.2016.10.004
Macworld.co.uk. Available online: https://www.macworld.co.uk/news/how-many-apple-watches-sold-3801687/. Accessed 6 Nov 2022
Apple.com. https://www.apple.com/healthcare/docs/site/Blood_Oxygen_app_on_Apple_Watch_October_2022.pdf. Accessed 6 Nov 2022
Pipek LZ, Nascimento RFV, Acencio MMP, Teixeira LR (2021) Comparison of SpO2 and heart rate values on Apple Watch and conventional commercial oximeters devices in patients with lung disease. Sci Rep 11(1):18901. https://doi.org/10.1038/s41598-021-98453-3. PMID: 34556765; PMCID: PMC8460792
Spaccarotella C, Polimeni A, Mancuso C et al (2022) Assessment of non-invasive measurements of oxygen saturation and heart rate with an Apple Smartwatch: comparison with a standard pulse oximeter. J Clin Med 11(6):1467. https://doi.org/10.3390/jcm11061467. PMID: 35329793; PMCID: PMC8951323
Van de Louw A, Cracco C, Cerf C et al (2001) Accuracy of pulse oximetry in the intensive care unit. Intensive Care Med 27(10):1606–1613. https://doi.org/10.1007/s001340101064
Perkins GD, McAuley DF, Giles S et al (2003) Do changes in pulse oximeter oxygen saturation predict equivalent changes in arterial oxygen saturation? Crit Care 7(4):R67. https://doi.org/10.1186/cc2339
Wilson BJ, Cowan HJ, Lord JA et al (2010) The accuracy of pulse oximetry in emergency department patients with severe sepsis and septic shock: a retrospective cohort study. BMC Emerg Med 5(10):9. https://doi.org/10.1186/1471-227X-10-9. PMID: 20444248; PMCID: PMC2876142
Amalakanti S, Pentakota MR (2016) Pulse oximetry overestimates oxygen saturation in COPD. Respir Care 61(4):423–427. https://doi.org/10.4187/respcare.04435. Epub 2015 Dec 29 PMID: 26715772
Hermand E, Coll C, Richalet J-P et al (2021) Accuracy and reliability of pulse O2 saturation measured by a wrist-worn oximeter. Int J Sports Med 42:1268–1273
Lauterbach CJ, Romano PA, Greisler LA et al (2021) Accuracy and reliability of commercial wrist-worn pulse oximeter during normobaric hypoxia exposure under resting conditions. Res Q Exerc Sport 92(3):549–558. https://doi.org/10.1080/02701367.2020.1759768. Epub 2020 Jul 7 PMID: 32633688
Acknowledgements
Apple Inc. was not involved in the design, implementation, data analysis, or manuscript preparation of the study.
Author information
Authors and Affiliations
Contributions
Arslan B. is the research principal. She also wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The present research was approved by the Ethics and Research Committee of the Basaksehir Cam and Sakura City Hospital. The registration number is 2021.03.3.
Animal and human rights statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. No animal studies were carried out by the authors for this article.
Informed consent
Written informed consent was obtained from the patients for their anonymized information to be published in this article.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arslan, B., Sener, K., Guven, R. et al. Accuracy of the Apple Watch in measuring oxygen saturation: comparison with pulse oximetry and ABG. Ir J Med Sci 193, 477–483 (2024). https://doi.org/10.1007/s11845-023-03456-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-023-03456-w