Abstract
Objective
We aimed to explore maternal and paternal risk factors with risk of congenital heart disease in infants.
Methods
A total of 125 congenital heart disease (CHD) infants and 125 controls were included in Heping Hospital Affiliated to Changzhi Medical College, Shanxi, China. Subjects were diagnosed between Jan 1, 2016 and Dec 31, 2021 in the present study. All the characteristics were collected with questionnaire by face-to-face interview, including maternal and paternal risk factors. Conditional logistic regression was conducted to explore the risk factors with risk of congenital heart disease in infants.
Results
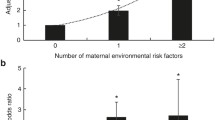
For maternal risk factors, we found that age, number of pregnancies, systolic blood pressure (SBP), diastolic blood pressure (DBP), and body mass index (BMI) were risk factors for CHD infants, and the ORs (95%CIs) were 1.15 (1.06–1.23) for age, 1.13 (1.02–1.29) for SBP, 1.06 (1.02–1.18) for DBP, 1.22 (1.16–1.31) for BMI. Compared with one pregnancy, the ORs (95%CIs) were 1.17 (1.05–1.29) for two pregnancies and 1.25 (1.16–1.47) for more pregnancies. For paternal risk factors, we found that age (OR = 1.07, 95%CI = 1.01–1.19), smoking (OR = 1.11, 95%CI = 1.03–1.27), drinking (OR = 1.04, 95%CI = 1.02–1.19), and BMI (OR = 1.15, 95%CI = 1.03–1.28) were risk factors for CHD infants.
Conclusion
We found that age, number of pregnancies, SBP, DBP, and BMI are maternal risk factors for CHD infants. And age, smoking, drinking, and BMI are paternal risk factors for CHD infants.
Similar content being viewed by others
Data availability
Data could be available on reasonable request from the corresponding author.
References
Griffin EL, Nees SN, Morton SU et al (2023) Evidence-based assessment of congenital heart disease genes to enable returning results in a genomic study. Circ Genom Prec Med e003791
Mery CM, Well A, Taylor K et al (2023) Examining the Real-life journey of individuals and families affected by single-ventricle congenital heart disease. J Am Heart Assoc e027556
Simões EAF, Madhi SA, Muller WJ et al (2023) Efficacy of nirsevimab against respiratory syncytial virus lower respiratory tract infections in preterm and term infants, and pharmacokinetic extrapolation to infants with congenital heart disease and chronic lung disease: a pooled analysis of randomised controlled trials. The Lancet Child & Adolescent Health 7:180–189
Tsao PC, Chiang SH, Shiau YS et al (2023) Comparing strategies for critical congenital heart disease newborn screening. Pediatrics
Lammers AE, Diller GP, Lober R et al (2021) Maternal and neonatal complications in women with congenital heart disease: a nationwide analysis. Eur Heart J 42:4252–4260
Kuehn BM (2020) New guideline emphasizes need for life-long care for congenital heart disease. Circulation 142:2276–2277
Liu D, Liu QQ, Guan LH et al (2016) BMPR2 mutation is a potential predisposing genetic risk factor for congenital heart disease associated pulmonary vascular disease. Int J Cardiol 211:132–136
Lee TM, Bacha EA (2016) Copy number variants in congenital heart disease: a new risk factor impacting outcomes? J Thorac Cardiovasc Surg 151:1152–1153
Jenkins KJ, Correa A, Feinstein JA et al (2007) Noninherited risk factors and congenital cardiovascular defects: current knowledge: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young: endorsed by the American Academy of Pediatrics. Circulation 115:2995–3014
Rankin J, Chadwick T, Natarajan M et al (2009) Maternal exposure to ambient air pollutants and risk of congenital anomalies. Environ Res 109:181–187
van Driel LM, de Jonge R, Helbing WA et al (2008) Maternal global methylation status and risk of congenital heart diseases. Obstet Gynecol 112:277–283
Begić H, Tahirović HF, Dinarević S, Ferković V (2002) Pranjić N [Risk factors for the development of congenital heart defects in children born in the Tuzla Canton]. Med Arh 56:73–77
Goldmuntz E (2001) The epidemiology and genetics of congenital heart disease. Clin Perinatol 28:1–10
Hollier LM, Leveno KJ, Kelly MA et al (2000) Maternal age and malformations in singleton births. Obs Gynecol 96:701–6
Verkleij-Hagoort AC, Verlinde M, Ursem NT et al (2006) Maternal hyperhomocysteinaemia is a risk factor for congenital heart disease. BJOG : an international journal of obstetrics and gynaecology 113:1412–1418
Gencheva DG, Nikolov FP, Uchikova EH et al (2022) Hypertension in pregnancy as an early sex-specific risk factor for cardiovascular diseases: evidence and awareness. Folia Med 64:380–387
Choi SK (2021) Editorial: Diabetes, Hypertension and cardiovascular diseases. Front Physiol 12:765767
Sun J, Chen X, Chen H et al (2015) Maternal alcohol consumption before and during pregnancy and the risks of congenital heart defects in offspring: a systematic review and meta-analysis. Congenit Heart Dis 10:E216–E224
Karunamuni G, Gu S, Doughman YQ et al (2014) Ethanol exposure alters early cardiac function in the looping heart: a mechanism for congenital heart defects? Am J Physiol Heart Circ Physiol 306:H414–H421
Serrano M, Han M, Brinez P, Linask KK (2010) Fetal alcohol syndrome: cardiac birth defects in mice and prevention with folate. Am J Obstet Gynecol 203(75):e7–e15
Gianicolo EA, Cresci M, Ait-Ali L et al (2010) Smoking and congenital heart disease: the epidemiological and biological link. Curr Pharm Des 16:2572–2577
Edwards JJ, Gelb BD (2016) Genetics of congenital heart disease. Curr Opin Cardiol 31:235–241
Acknowledgements
The contributions of all the participants and all members of study team are greatly acknowledged.
Author information
Authors and Affiliations
Contributions
JXD and TYH designed the research, conducted the research, and performed statistical analysis. JXD wrote the paper. TYH revised the paper. TYH had primary responsibility for final content. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Ethics and Human Subject Committee of Changzhi Medical College (no. 1754235).
Consent to participate
Written informed consent was obtained from all the participants.
Consent for publication
This is not applicable.
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dong, J., Hao, T. Association of maternal and paternal risk factors with risk of congenital heart disease in infants: a case–control study. Ir J Med Sci 193, 95–99 (2024). https://doi.org/10.1007/s11845-023-03409-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-023-03409-3