Abstract
Purpose
Investigate the survival and risk factors that affect the survival of aged patients in a palliative care center (PCC).
Methods
A total of 180 inpatients (aged ≥ 65 years) who were admitted to a PCC from January 2018 to March 2020 were included. Information regarding patients’ demographic characteristics, chronic diseases, length of hospital stay, nutrition provided at the first hospital stay, pressure wound, pain, and laboratory results were evaluated.
Results
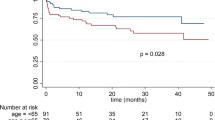
The patients 50% were women (n = 90). The mean age, mean comorbidity, and mean follow-up duration was 77.6 years, 3.4, and 115 days (median: 29 days), respectively. The mean NRS2002 score of patients was 4.0 ± 1.0 and the risk of malnutrition was 93%. The mortality rate of the patients was 91.7%. The life expectancy of patients without malignancy was higher than those with malignancy (p < 0.001). Enteral nutrition (EN) via percutaneous endoscopic gastrostomy (PEG) was associated with up to two-fold increase in the survival rates of patients with PCC (p = 0.049, HR: 2.029). High neutrophil/lymphocyte ratio (p = 0.002, HR: 1.017) and high ferritin (p = 0.001, HR: 1.000) and C-reactive protein (CRP) levels (p < 0.001, HR: 1.006) were adverse risk factors affecting life expectancy. Malignity reduced the survival rate of aged patients with PCC by 40% (p = 0.008).
Conclusion
EN via PEG was found to be a positive factor affecting survival rates of older adult patients in palliative care, whereas malignity, high neutrophil/lymphocyte ratio, high CRP and ferritin levels, and prolonged hospital stays were negative risk factors.


Similar content being viewed by others
References
Turkey statistical institution elderly with statistics (2020). Available from: https://data.tuik.gov.tr/Bulten/Index?p=Elderly-Statistics-2020-37227. Accessed 21 Dec 2021
World Health Organization. WHO definition of palliative care. (2020). Available from: https://www.who.int/news-room/fact-sheets/detail/palliative-care. Accessed 9 Feb 2022
Vanbutsele G, Van Belle S, Surmont V et al (2020) The effect of early and systematic integration of palliative care in oncology on quality of life and health care use near the end of life: a randomised controlled trial. Eur J Cancer 124:186–193. https://doi.org/10.1016/j.ejca.2019.11.009
Balducci L (2019) Geriatric oncology, spirituality, and palliative care. J Pain Symptom Manage 57(1):171–175. https://doi.org/10.1016/j.jpainsymman.2018.05.009. Epub 2018 Jun 19 PMID: 29772281
Digwood G, Lustbader D, Pekmezaris R et al (2011) The impact of a palliative care unit on mortality rate and length of stay for medical intensive care unit patients. Palliat Support Care 9(4):387–392. https://doi.org/10.1017/S147895151100040X
Martins BDCPCC, Oliveira RA, Cataneo AJM (2017) Palliative care for terminally ill patients in the intensive care unit: systematic review and metaanalysis. Palliat Support Care 15(3):376–383. https://doi.org/10.1017/S1478951516000584. Epub 2016 Jul 27. PMID: 27460968
Souza Cunha M, Wiegert EVM, Calixto-Lima L, Oliveira LC (2018) Relationship of nutritional status and inflammation with survival in patients with advanced cancer in palliative care. Nutrition 51–52:98–103. https://doi.org/10.1016/j.nut.2017.12.004
Kondrup J, Allison SP, Elia M et al (2003) ESPEN guidelines for nutrition screening 2002. Clin Nutr 22(4):415–421
Bergstrom N, Braden BJ, Laguzza A, Holman V (1987) The Braden scale for predicting pressure sore risk. Nurs Res 36(4):205–210
Hawker GA, Mian S, Kendzerska T et al (2011) Measures of adult pain: visual analog scale for pain (VAS Pain), numeric rating scale for pain (NRS Pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP). Arthritis Care Res (Hoboken) 63(Suppl 11):240–252
Temel JS, Greer JA, Muzikansky A et al (2010) Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 363(8):733–742. https://doi.org/10.1056/NEJMoa1000678
Kavalieratos D, Corbelli J, Zhang D et al (2016) Association between palliative care and patient and caregiver outcomes: a systematic review and meta-analysis. JAMA 316(20):2104–2114. https://doi.org/10.1001/jama.2016.16840
Irmak İ, Adıgüzel N, Yıldız E et al (2020) The comparison of the survival rates of intensive and palliative care units. Yoğun bakım ve palyatif bakım ünitelerinin sağkalım oranlarının karşılaştırılması. Tuberk Toraks 68(3):245–251. https://doi.org/10.5578/tt.69753
Malmgren A, Hede GW, Karlström B et al (2011) Indications for percutaneous endoscopic gastrostomy and survival in old adults. Food Nutr Res 55. https://doi.org/10.3402/fnr.v55i0.6037
Suhrie EM, Hanlon JT, Jaffe EJ et al (2009) Impact of a geriatric nursing home palliative care service on unnecessary medication prescribing. Am J Geriatr Pharmacother 7(1):20–25
Yürüyen M, Özbaş Tevetoğlu I , Tekmen Y et al (2018) Prognostic factors and clinical features in palliative care patients. Konuralp Med J 10(1):74–80. https://doi.org/10.18521/ktd.368570
Cederholm T, Barazzoni R, Austin P et al (2017) ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr 36(1):49–64. https://doi.org/10.1016/j.clnu.2016.09.004
Van Venrooij LMW, de Vos R, Borgmeijer-Hoelen AMMJ et al (2007) Quick-and-easy nutritional screening tools to detect disease-related undernutrition in hospital in- and outpatient settings: a systematic review of sensitivity and specificity. Eur E J Clin Nutr Metabol 2:21–37. https://doi.org/10.1016/j.eclnm.2007.03.001
Waitzberg DL, Caiaffa WT, Correia MI (2001) Hospital malnutrition: the Brazilian national survey (IBRANUTRI): a study of 4000 patients. Nutrition 17(7–8):573–580. https://doi.org/10.1016/s0899-9007(01)00573-1
Raslan M, Gonzalez MC, Torrinhas RS et al (2011) Complementarity of subjective global assessment (SGA) and nutritional risk screening 2002 (NRS 2002) for predicting poor clinical outcomes in hospitalized patients. Clin Nutr 30(1):49–53. https://doi.org/10.1016/j.clnu.2010.07.002
Efendioglu EM, Cigiloglu A, Turkbeyler IH (2021) Malnutrition and depressive symptoms in elderly palliative care patients. J Palliat Care 14:8258597211045500. https://doi.org/10.1177/08258597211045500. Epub ahead of print. PMID: 34647838
Pezzana A, Cereda E, Avagnina P et al (2015) Nutritional care needs in elderly residents of long-term care institutions: potential implications for policies. J Nutr Health Aging 19(9):947–954. https://doi.org/10.1007/s12603-015-0537-5
Lelovics ZA (2009) Nutritional status and nutritional rehabilitation of elderly people living in long-term care institutions. Orv Hetil 150(44):2028–2036. https://doi.org/10.1556/OH.2009.28723
Volkert D, Beck AM, Cederholm T et al (2022) ESPEN practical guideline: clinical nutrition and hydration in geriatrics. Clin Nutr 41(4):958–989. https://doi.org/10.1016/j.clnu.2022.01.024
Higaki F, Yokota O, Ohishi M (2008) Factors predictive of survival after percutaneous endoscopic gastrostomy in the elderly: is dementia really a risk factor? Am J Gastroenterol 103(4):1011–1017. https://doi.org/10.1111/j.1572-0241.2007.01719.x
Amano K, Maeda I, Ishiki H et al (2021) Effects of enteral nutrition and parenteral nutrition on survival in patients with advanced cancer cachexia: analysis of a multicenter prospective cohort study. Clin Nutr 40(3):1168–1175. https://doi.org/10.1016/j.clnu.2020.07.027
Blomberg J, Lagergren P, Martin L et al (2011) Albumin and C-reactive protein levels predict short-term mortality after percutaneous endoscopic gastrostomy in a prospective cohort study. Gastrointest Endosc 73(1):29–36. https://doi.org/10.1016/j.gie.2010.09.012. Epub 2010 Nov 12 PMID: 21074760
Limpias Kamiya KJL, Hosoe N, Takabayashi K et al (2021) Factors predicting major complications, mortality, and recovery in percutaneous endoscopic gastrostomy. JGH Open 5(5):590–598. Published 2021 Mar 31. https://doi.org/10.1002/jgh3.12538
Barbosa M, Magalhaes J, Marinho C, Cotter J (2016) Predictive factors of early mortality after percutaneous endoscopic gastrostomy placement: the importance of C-reactive protein. Clin Nutr ESPEN 14:19–23. https://doi.org/10.1016/j.clnesp.2016.04.029. Epub 2016 May 17 PMID: 28531394
Soysal P, Stubbs B, Lucato P et al (2017) Ageing Res Rev 35:364–365. https://doi.org/10.1016/j.arr.2016.12.007. Epub 2017 Jan 13
McMillan DC (2008) An inflammation-based prognostic score and its role in the nutrition-based management of patients with cancer. Proc Nutr Soc 67(3):257–262. https://doi.org/10.1017/S0029665108007131
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Our study was approved by the University of Health Science, Bakirkoy Dr. Sadi Konuk Education and Research Hospital Ethics Committee (protocol code: 2021/311, decision number:2021–11-17). The authors assert that all procedures contributing to this work comply with the ethical standards in Bakırkoy Dr. Sadi Konuk Training and Research Hospital and the Helsinki Declaration of 1975, as revised in 2008.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yuruyen, M., Polat, O., Denizli, B.O. et al. Survival and factors affecting the survival of older adult patients in palliative care. Ir J Med Sci 192, 1561–1567 (2023). https://doi.org/10.1007/s11845-022-03186-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-022-03186-5